Introduction
The temporoparietal fascia flap (TPFF) is a versatile flap well-recognized in the reconstruction of craniofacial defects (see Image. Temporoparietal Fascia Flap).[1] Most commonly, the TPFF is utilized in a pedicled fashion for the reconstruction of the scalp, auricle, facial soft tissue, orbit, oral cavity, and nasopharynx, as well as for skull base defects.[2] Moreover, the flap may be harvested with the overlying scalp, making it particularly useful for defects of hair-bearing regions.[3] Additionally, if more substantial reconstruction is required, the TPFF may be elevated in a combined or chimeric fashion with temporalis muscle and/or adjacent calvarial bone.[4][5] When harvested for free microvascular anastomosis, the TPFF can be useful for a wide array of distal extremity reconstructions, particularly in the hands and feet.[6]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
To increase the chances of harvesting a viable temporoparietal fascia flap, it is critical to understand the relevant anatomy.
Layers (from superficial to deep) potentially encountered during harvesting of the TPFF include:
- Skin
- Subcutaneous tissue
- Temporoparietal fascia (within which the temporoparietalis muscle may be encountered)
- Loose areolar tissue
- The superficial layer of the deep temporal fascia
- Temporalis muscle
- The deep layer of the deep temporal fascia
- Pericranium
- Bone
The temporoparietal fascia (also known as the superficial temporal fascia) is a thin layer of connective tissue lying below the level of the subcutaneous adipose tissue and superficial to the fascia of the temporalis muscle (the deep temporal fascia).[7] The TPFF lies in continuity with the adjacent galea aponeurotica, which exists medial to the temporal line, and the superficial musculoaponeurotic system of the face, located inferior to the zygomatic arch (see Image. Fascial Planes of the Face).[8]
Blood Supply
- The superficial temporal artery (STA) has a well-described course within the substance of the flap itself. The main STA divides into multiple segments, roughly 3 cm above the level of the zygomatic arch. The terminal branches of the STA arborize with the vessels supplying the pericranium.
- The STA also gives rise to the middle temporal artery, which supplies the temporalis muscle. When dissected together, the surgeon may concomitantly harvest the deep temporal fascia and/or temporalis muscle during the TPFF harvest.[4]
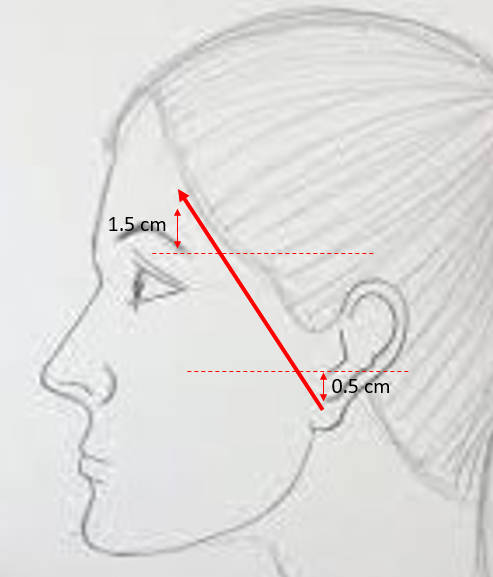
NOTE: Dissection along the anterior/frontal branch of the STA may put the frontotemporal branch of the facial nerve at risk. Injury to this nerve will result in ipsilateral brow ptosis and forehead paralysis. Various anatomic landmarks can be used to help identify the course and/or location of this nerve, including:
- Pitanguy’s line - line drawn from 0.5 cm inferior to the tragus to a 1.5 cm superolateral to the lateral brow (see Image. The Course of the Temporal Branch).[9]
- A point 2.85 cm superior and 2.54 cm lateral to the lateral canthus[10]
- A point 6.4 mm cephalad to the sentinel vein (useful landmark for endoscopic brow lifts)[11]
- A point 2.4 cm anterior to where the zygomatic arch meets the helix[11]
Indications
Temporoparietal fascia flap transfer is an important technique in head and neck, hand, and lower extremity reconstruction. The TPFF can be harvested as a pedicled flap, a composite flap (along with deep temporal fascia with or without the inclusion of surrounding calvarial bone), or as a free tissue flap, depending on the size and thickness of the defect needing to be repaired.[12][13][14] Without a doubt, however, the thin nature of the TPFF renders it a great choice for reconstructing a variety of defects involving the skull base, facial soft tissues, nasopharynx, oral cavity, orbit, ear, and scalp.[15]
TPFF transfer constitutes a routine part of auricular reconstruction for microtia, whether using autologous costal cartilage or porous polyethylene implants, and is frequently used for the salvage of these reconstructions after trauma or infection as well.[16] It is also commonly used for several other applications in the head and neck, including acting as a barrier between the parotid gland and the skin to reduce the symptoms of Frey syndrome and filling in the soft tissue deficit that remains after temporalis muscle flap transfer or parotidectomy.[17][18][19] In hand surgery, the thin and pliable nature of the TPFF is well-suited to ensuring tendons are able to glide smoothly within the hand and fingers, making the flap an ideal reconstructive option.[20][21]
Contraindications
There are a few contraindications to consider when performing a temporoparietal fascia flap transfer:
- When used as a pedicled flap, the surgeon should first consider the anatomical reach limitations of the proposed TPFF.
- The surgeon should be mindful that previous radiation therapy may have altered the microvascular anatomy of the flap and potentially can lead to a higher failure rate.
- Prior trauma, surgery, or manipulation of the superficial temporal vascular system (e.g., STA biopsy for temporal cell arteritis) may have interrupted the flap's vascular supply.
Equipment
Preoperatively
- Surgical marker
- Local anesthesia (per surgeon preference)
- Topical antiseptic
- Based on the clinical scenario, a corneal shield may be considered for eye protection
- Facial nerve monitoring system (not routinely employed)
Intraoperatively
- Head and neck soft tissue surgical tray
- Bipolar cautery
- #15 blade scalpel
- Multiprong retractors
- Closed suction drain with bulb
- Material for closure of scalp skin (suture vs. staple) per surgeon preference
Postoperatively
- Antibiotic ointment
- Wound dressing material (per surgeon preference)
Personnel
- Surgeon
- Surgical assistant
- Surgical scrub technician
- Operating room nurse (circulator)
- Anesthesiologist and/or nurse anesthetist
Preparation
- The patient should be risk-stratified and medically optimized for general anesthesia.
- A thorough preoperative head and neck examination, including an assessment of facial nerve function, should be performed.
- Preoperative photography may be considered to document the defect's shape, size, and location.
- The patient should be appropriately counseled regarding the procedure's risks, benefits, and alternatives. Pertinent to this procedure, it is important to mention flap compromise, alopecia, paresthesias, and facial nerve injury, among the other more common risks associated with surgery (e.g., pain, bleeding, infection, scarring, etc.).
- The surgeon should mark the skin incisions in the temporal scalp to ensure maximal preservation of the hairline. The Y or T-shaped incision is made parallel to the course of the STA. The arterial bifurcation is commonly found 3 centimeters above the helical root.
- Important landmarks are identified, including the STA and trajectory of the frontotemporal branch of the facial nerve.
- General anesthesia is recommended. Long-acting paralytics are usually avoided to permit intraoperative facial nerve monitoring. Similarly, some surgeons will prefer to avoid using local anesthesia, instead substituting plain 1:100,000 epinephrine to avoid interfering with nerve monitoring.
- A single dose of intravenous antibiotics covering skin flora is given preoperatively.
Technique or Treatment
It is not strictly necessary to shave any hair during this procedure, though it may be helpful to shave the hair 1 to 2 cm beyond the anticipated incision line.
- A Y or T-shaped incision is planned in the preauricular crease and extended several centimeters cranially. Some surgeons prefer to zigzag the vertical portion of the incision in order to improve scar camouflage postoperatively.
- The incision is made through the skin, dermis, and subcutaneous fat. The elevation of the scalp flaps is performed in a subcutaneous plane just below the level of the hair follicles. This step is of utmost importance as it assists the surgeon in maintaining the appropriate depth of dissection and preserves robust temporoparietal fascia flap thickness. Sharp dissection with a scalpel is preferred to avoid thermal injury to the hair follicles and decrease the risk of alopecia.
- Care should be taken to avoid injuring the underlying STA, which courses through the substance of the flap itself. Once the required size of the TPFF is exposed, the surgeon can incise the periphery of the temporoparietal fascia sharply, with care taken to preserve the vascular pedicle. At this step, the distal branches of the superficial temporal artery are ligated. The surgeon may now rotate the flap into the defect. If hair-bearing skin is required, this flap may be harvested in continuity with the overlying skin. NOTE: One should be mindful during anterior dissection to avoid injuring the frontotemporal branch of the facial nerve, which lies either within or just beneath the temporoparietal fascia. Dissection performed underneath the hair-bearing scalp is typically not near enough to the frontotemporal branch of the facial nerve for inadvertent injury to be likely.
- The STA may be dissected farther proximally until the middle temporal artery is identified. The surgeon may enter the parotid gland in certain situations to facilitate this step. At this point, the flap may be harvested as a chimeric flap to include the deep temporal fascia and/or temporalis muscle. If desired, the surgeon can extend the dissection beyond the temporal fossa to include the pericranium and/or harvest a vascularized strip of calvarium (outer cortex).
- The surgeon may either rotate or tunnel this flap into the desired defect, or the vascular bundle may be ligated in anticipation of free microvascular reconstruction of distal defects.
- An optional closed suction drain may be placed.
- The skin flaps are then reapproximated with deep absorbable sutures, followed by staples or suture closure of the scalp.
- If the TPFF is used to reconstruct a defect, including skin, but the scalp is not harvested with the flap, a skin graft may be applied on top of the TPFF (e.g., during auricular reconstruction).
Complications
Potential complications for a temporoparietal fascia flap may include[22]:
- Alopecia
- Flap necrosis
- Frontalis and corrugator supercilii muscle weakness following an injury to the frontal branch of the facial nerve
- Venous congestion
- Wound breakdown
- Hematoma formation
- Infection
- Unfavorable scarring
- Paresthesia
Most complications can be avoided with meticulous dissection and careful flap elevation that respects the local scalp anatomy. Rates of flap loss (partial vs. total) are roughly 2.44%.[13] Some degree of alopecia may occur in up to 8% of patients.[20] Injury to the frontotemporal branch of the facial nerve resulting in transient weakness to paralysis may range from 1% to 20%.[23]
Clinical Significance
A temporoparietal fascia flap is a work-horse option in the armamentarium of the reconstructive surgeon. TPFF transfer is a low-risk option for reconstructing local (craniofacial) and distal soft tissue defects. It has found popularity in head and neck reconstruction as a pedicled flap but may be harvested as a free flap for extremity reconstruction. The outcomes can be very satisfactory in the hands of an experienced and knowledgeable surgeon. Additionally, there is very little donor site morbidity, with most patients and surgeons not noticing any decreased soft tissue mass within the temporal fossa.
Enhancing Healthcare Team Outcomes
Identifying risk factors and performing a thorough assessment before transferring a temporoparietal fascial flap is imperative. The patient should be evaluated by a surgeon experienced in reconstructive surgery using the TPFF. If necessary, the patient should see a primary care provider for medical optimization in anticipation of general anesthesia. Lastly, the patient should be monitored by the preoperative, operative, and postoperative specialty nurses to assist with the coordination of care and education.
An interprofessional team consisting of an experienced surgeon, anesthesiologist, surgical assistant, and operative nurse should perform the TPFF transfer to optimize outcomes. Close follow-up should monitor the patient for potential complications: flap necrosis, alopecia, wound breakdown, hematoma, and facial paralysis. Team members should counsel the patient regarding appropriate wound care and postoperative activity level.
Nursing, Allied Health, and Interprofessional Team Interventions
Recovery following a temporoparietal fascia flap transfer depends on the complexity of the original problem for which the reconstruction was performed. Local wound care is critical to ensure a healthy and clean surgical environment. Suction drains (if placed) can be removed when output has appropriately decreased (e.g., less than 30 mL over 24 hours). The patient should avoid rigorous activity for ten days following surgery to allow adequate wound healing and minimize edema, ecchymosis, and bleeding. After discharge, the patient is typically followed regularly for several weeks to months to ensure proper healing.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
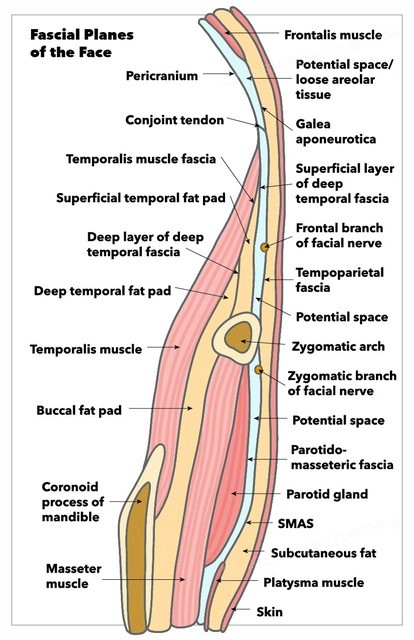
Fascial Planes of the Face. This illustration shows the fascial planes of the face while demonstrating the continuity of the frontalis muscle, galea aponeurotica, temporoparietal fascia, superficial musculoaponeurotic system, platysma, and facial nerve's location.
Contributed by K Humphreys and MH Hohman, MD, FACS
(Click Image to Enlarge)
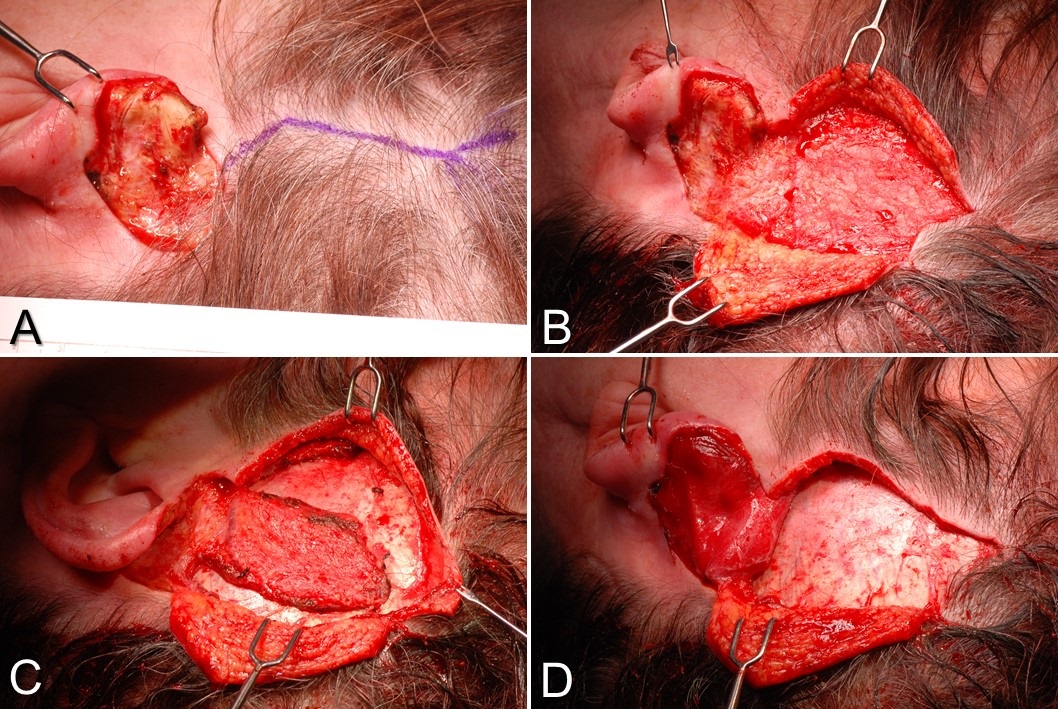
Temporoparietal Fascia Flap. A) This is a postauricular defect from Mohs surgery with too much bare cartilage for a skin graft alone to survive. A Y-shaped incision is planned, paralleling the course of the superficial temporal artery. B) The scalp flaps are elevated in a subdermal plane, exposing the temporoparietal fascia. C) The temporoparietal fascia flap is incised on 3 sides, with the pedicle intact inferiorly. D) The temporoparietal fascia flap is transferred into the defect, after which the scalp will be closed in layers, and a skin graft will be applied to the flap.
Contributed by MH Hohman, MD, FACS
References
Garfein E, Doscher M, Tepper O, Gill J, Gorlick R, Smith RV. Reconstruction of the pediatric midface following oncologic resection. Journal of reconstructive microsurgery. 2015 Jun:31(5):336-42. doi: 10.1055/s-0035-1544181. Epub 2015 Mar 24 [PubMed PMID: 25803408]
Li D, Xu F, Zhang R, Zhang Q, Xu Z, Li Y, Wang C, Li T. Surgical Reconstruction of Traumatic Partial Ear Defects Based on a Novel Classification of Defect Sizes and Surrounding Skin Conditions. Plastic and reconstructive surgery. 2016 Aug:138(2):307e-316e. doi: 10.1097/PRS.0000000000002408. Epub [PubMed PMID: 27465192]
Marks MW, Friedman RJ, Thornton JW, Argenta LC. The temporal island scalp flap for management of facial burn scars. Plastic and reconstructive surgery. 1988 Aug:82(2):257-61 [PubMed PMID: 3399556]
Level 3 (low-level) evidenceJose A,Nagori SA,Arya S,Roy ID, Chimeric temporopareital osteofascial and temporalis muscle flap; a novel method for the reconstruction of composite orbito-maxillary defects. Journal of stomatology, oral and maxillofacial surgery. 2019 Jun; [PubMed PMID: 30763779]
Denadai R, Raposo-Amaral CE, Marques FF, Raposo-Amaral CA. Posttraumatic eyebrow reconstruction with hair-bearing temporoparietal fascia flap. Einstein (Sao Paulo, Brazil). 2015 Jan-Mar:13(1):106-9. doi: 10.1590/S1679-45082015RC2834. Epub 2015 Mar 3 [PubMed PMID: 25993077]
Schreiber M, Dragu A. Free temporal fascia flap to cover soft tissue defects of the foot: a case report. GMS Interdisciplinary plastic and reconstructive surgery DGPW. 2015:4():Doc01. doi: 10.3205/iprs000060. Epub 2015 Jan 13 [PubMed PMID: 26504730]
Level 3 (low-level) evidenceOlcott CM, Simon PE, Romo T 3rd, Louie W. Anatomy of the superficial temporal artery in patients with unilateral microtia. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2019 Jan:72(1):114-118. doi: 10.1016/j.bjps.2018.09.001. Epub 2018 Sep 28 [PubMed PMID: 30528867]
Mitz V,Peyronie M, The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plastic and reconstructive surgery. 1976 Jul; [PubMed PMID: 935283]
Pitanguy I, Ramos AS. The frontal branch of the facial nerve: the importance of its variations in face lifting. Plastic and reconstructive surgery. 1966 Oct:38(4):352-6 [PubMed PMID: 5926990]
Schmidt BL, Pogrel MA, Hakim-Faal Z. The course of the temporal branch of the facial nerve in the periorbital region. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2001 Feb:59(2):178-84 [PubMed PMID: 11213986]
Trinei FA, Januszkiewicz J, Nahai F. The sentinel vein: an important reference point for surgery in the temporal region. Plastic and reconstructive surgery. 1998 Jan:101(1):27-32 [PubMed PMID: 9427913]
Safavi-Abbasi S, Komune N, Archer JB, Sun H, Theodore N, James J, Little AS, Nakaji P, Sughrue ME, Rhoton AL, Spetzler RF. Surgical anatomy and utility of pedicled vascularized tissue flaps for multilayered repair of skull base defects. Journal of neurosurgery. 2016 Aug:125(2):419-30. doi: 10.3171/2015.5.JNS15529. Epub 2015 Nov 27 [PubMed PMID: 26613175]
Mokal NJ, Ghalme AN, Kothari DS, Desai M. The use of the temporoparietal fascia flap in various clinical scenarios: A review of 71 cases. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India. 2013 Sep:46(3):493-501. doi: 10.4103/0970-0358.121988. Epub [PubMed PMID: 24459337]
Level 3 (low-level) evidenceJaquet Y, Higgins KM, Enepekides DJ. The temporoparietal fascia flap: a versatile tool in head and neck reconstruction. Current opinion in otolaryngology & head and neck surgery. 2011 Aug:19(4):235-41. doi: 10.1097/MOO.0b013e328347f87a. Epub [PubMed PMID: 21593668]
Level 3 (low-level) evidenceCollar RM, Zopf D, Brown D, Fung K, Kim J. The versatility of the temporoparietal fascia flap in head and neck reconstruction. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2012 Feb:65(2):141-8. doi: 10.1016/j.bjps.2011.05.003. Epub 2011 Jun 22 [PubMed PMID: 21700520]
Tahiri Y,Reinisch J, Porous Polyethylene Ear Reconstruction. Clinics in plastic surgery. 2019 Apr [PubMed PMID: 30851753]
Andrews J, Kopacz AA, Hohman MH. Ear Microtia. StatPearls. 2024 Jan:(): [PubMed PMID: 33085390]
Rubinstein RY, Rosen A, Leeman D. Frey syndrome: treatment with temporoparietal fascia flap interposition. Archives of otolaryngology--head & neck surgery. 1999 Jul:125(7):808-11 [PubMed PMID: 10406323]
Level 3 (low-level) evidenceMovassaghi K, Lewis M, Shahzad F, May JW Jr. Optimizing the Aesthetic Result of Parotidectomy with a Facelift Incision and Temporoparietal Fascia Flap. Plastic and reconstructive surgery. Global open. 2019 Feb:7(2):e2067. doi: 10.1097/GOX.0000000000002067. Epub 2019 Feb 8 [PubMed PMID: 30881826]
Hing DN, Buncke HJ, Alpert BS. Use of the temporoparietal free fascial flap in the upper extremity. Plastic and reconstructive surgery. 1988 Apr:81(4):534-44 [PubMed PMID: 3347663]
Level 3 (low-level) evidenceUpton J, Rogers C, Durham-Smith G, Swartz WM. Clinical applications of free temporoparietal flaps in hand reconstruction. The Journal of hand surgery. 1986 Jul:11(4):475-83 [PubMed PMID: 3722753]
Level 3 (low-level) evidenceMavropoulos JC, Bordeaux JS. The temporoparietal fascia flap: a versatile tool for the dermatologic surgeon. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2014 Sep:40 Suppl 9():S113-9. doi: 10.1097/dss.0000000000000114. Epub [PubMed PMID: 25158871]
Level 3 (low-level) evidenceYano H, Fukui M, Yamada K, Nishimura G. Endoscopic harvest of free temporoparietal fascial flap to improve donor-site morbidity. Plastic and reconstructive surgery. 2001 Apr 1:107(4):1003-9 [PubMed PMID: 11252096]