Acute and Chronic Thermal Burn Evaluation and Management
Acute and Chronic Thermal Burn Evaluation and Management
Introduction
Thermal burns are a significant cause of worldwide morbidity and mortality. They can lead to debilitating, lifelong injuries and have a serious psychological and economic impact. With proper treatment, successful functional and emotional recovery is possible. After reviewing this article, the reader should be familiar with basic approaches to burn care, the underlying pathophysiology of thermal injuries, and the interprofessional effort required for successful post-operative care.[1][2][3][4][5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Thermal burns result from tissue exposure to an external heat source. Burns that occur at higher temperatures or for extended contact times result in deeper, more severe injuries. There are three main thermal burn mechanisms. Flash and flame burns occur due to direct or indirect exposure of a patient to a flame source. These flames result from a triad of an ignition source, an oxidizing agent, and a fuel source. Inhalation injuries may occur if patients are exposed to open flames in a closed setting. Scald burns result from exposure of the patient to high-temperature liquids. Grease burns and those due to hot oils are often much deeper than the initial examination suggests. Finally, contact burns occur from direct contact with a high-temperature object. Individuals with medical conditions such as epilepsy or habits like alcoholism that predispose them to periods of incapacitation are at higher risk of this mechanism of injury.
Epidemiology
According to the World health organization (WHO), thermal burns account for an estimated 6.6 million injuries and 300 thousand deaths each year worldwide. An estimated 95% of these deaths occur in low-income countries due to lack of education and access to medical care as well as the more common use of open fires for heating, lighting, and cooking. The 2014 World fire statistics showed that fire-related burn injuries have a significant economic impact with an estimated 0.02-0.22% of average gross domestic product (GDP) attributed to direct losses and 0.002-0.95% to indirect losses. Approximately two-thirds of fire-related costs were attributed to males. Deaths per 100 thousand ranged from 0.02 (Singapore) to 2.03 (Finland) with the United States in the middle at 1.11. Flash and flame burns accounted for the majority of adult burn admissions while scald burns accounted for the majority of pediatric burns.
Pathophysiology
The skin is the largest organ in the body and is composed of the superficial epidermis, the underlying dermis (further divided into the upper papillary dermis and lower reticular dermis), and the hypodermis, composed of subcutaneous fat and connective tissue.
Thermal burn pathophysiology can be broken into local and systemic responses. When excessive heat is transferred to the skin, it radiates outward from the point of initial contact and forms a local response with three zones in all directions. The zone of coagulation is the central contact point of maximal damage in which cell death, denaturation of proteins in the extracellular matrix, and damage to the circulation occur. Damaged circulation near the zone of coagulation results in a second surrounding zone of stasis. The third peripheral zone of hyperemia results from increased circulation as the body responds to injury. The zone of stasis can recover with proper resuscitation and adequate wound care. On the contrary, prolonged periods of hypotension and inadequate wound care can convert the zone of stasis and even the zone of hyperemia into wider and deeper tissue damage.
The systemic response following a burn can be massive. In a large burn, two clinically significant processes occur. The release of systemic inflammatory mediators and cytokines results in increased capillary permeability and wide-scale extravasation of fluid and proteins from the intravascular to the extravascular space. This can result in life-threatening hypotension, pulmonary edema, and decreased circulation to end organs and the already stressed integument in a response similar to that of severe sepsis and septic shock. The second process is due to physical skin loss. The skin plays several important roles in homeostasis including temperature control, and fluid regulation, and it serves as a physical barrier to infection as well as a point of contact to mediate interpretation of our environment. Large surface area loss of this vital organ interrupts these important processes.
With a flash and flame burn in an enclosed setting, one can be exposed to high levels of carbon dioxide. Carbon dioxide, which has a 40 times higher affinity for hemoglobin than oxygen, causes intracellular and extracellular hypoxia by displacing oxygen from hemoglobin as well as interrupting oxidative respiration by binding to proteins in the cytochrome oxidase pathway. Inhalation of smoke can also result in facial and supraglottic burns, but true subglottic and lower respiratory tract burns are rare due to the protective mechanism of reflexive vocal chord closure. The products of combustion can travel deep into the respiratory tract and cause mucosal irritation, leading to bronchospasm and local or systemic inflammation, and capillary leak. True inhalation injury causes a significant increase in mortality.
A burn wound is considered fully healed after final epithelialization. Open wounds epithelialize two ways, circumferentially inward from the intact epithelium at the periphery and from basal cells in underlying dermal appendages such as hair follicles and sebaceous/sweat glands. Therefore, the depth of a burn will largely dictate the healing process as deeper burns will no longer have dermal appendages and epithelialization will depend solely on circumferential growth from the wound periphery, a much slower process.
From superficial to deep, the first category of burn injuries includes first-degree or superficial burns. These are confined in the depth of the epidermis, and all dermal appendages and nerve endings are intact. Superficial burns generally heal in three to five days with minimal intervention and do not leave significant scarring. Second-degree burns are broken up into superficial partial-thickness burns, which involve the papillary dermis with intact dermal appendages and partially damaged nerves, and deep partial-thickness burns, which involve the deeper reticular dermis and have significant damage to nerves and dermal appendages. Superficial partial burns are very painful but generally heal in 10 to 15 days with minimal scarring, although pigmentary changes can occur. Deep partial burns can only epithelialize from the periphery of the wound and therefore heal at a much slower average of three to five weeks with significant scarring and scar contracture. Third-degree or full-thickness burns involve the entire epidermis and dermis and will form significant scarring and contractures with prolonged healing times without surgical intervention. Fourth-degree burns involve the skin, underlying subcutaneous fat, and even muscle or bone. These will require more extensive debridements, the use of dermal autografts, and possibly amputations during treatment.
History and Physical
In addition to a standard history of present illness, past medical history, social history, surgical history, family history, review of systems, and current medication lists/allergies, there are several key points to the patient history specific to thermal burn care. Mechanism of injury will give insight into burn depth and concomitant trauma or inhalation injury. Certain patterns such as scald burns with discrete lines of demarcation and discrepancies between the physical exam and history should raise suspicion for abuse, especially in the pediatric and elderly population. One should ask about the volume and type of resuscitation fluid the patient received en route for proper calculation of resuscitation fluid rates. The history should specifically focus on factors that will negatively affect wound healing (smoking, diabetes, chronic steroids) or increase the risk of surgery (chronic obstructive pulmonary disease [COPD], coronary artery disease [CAD], personal/family history of problems with anesthesia, blood clotting, or bleeding disorders) as these can change treatment strategies.
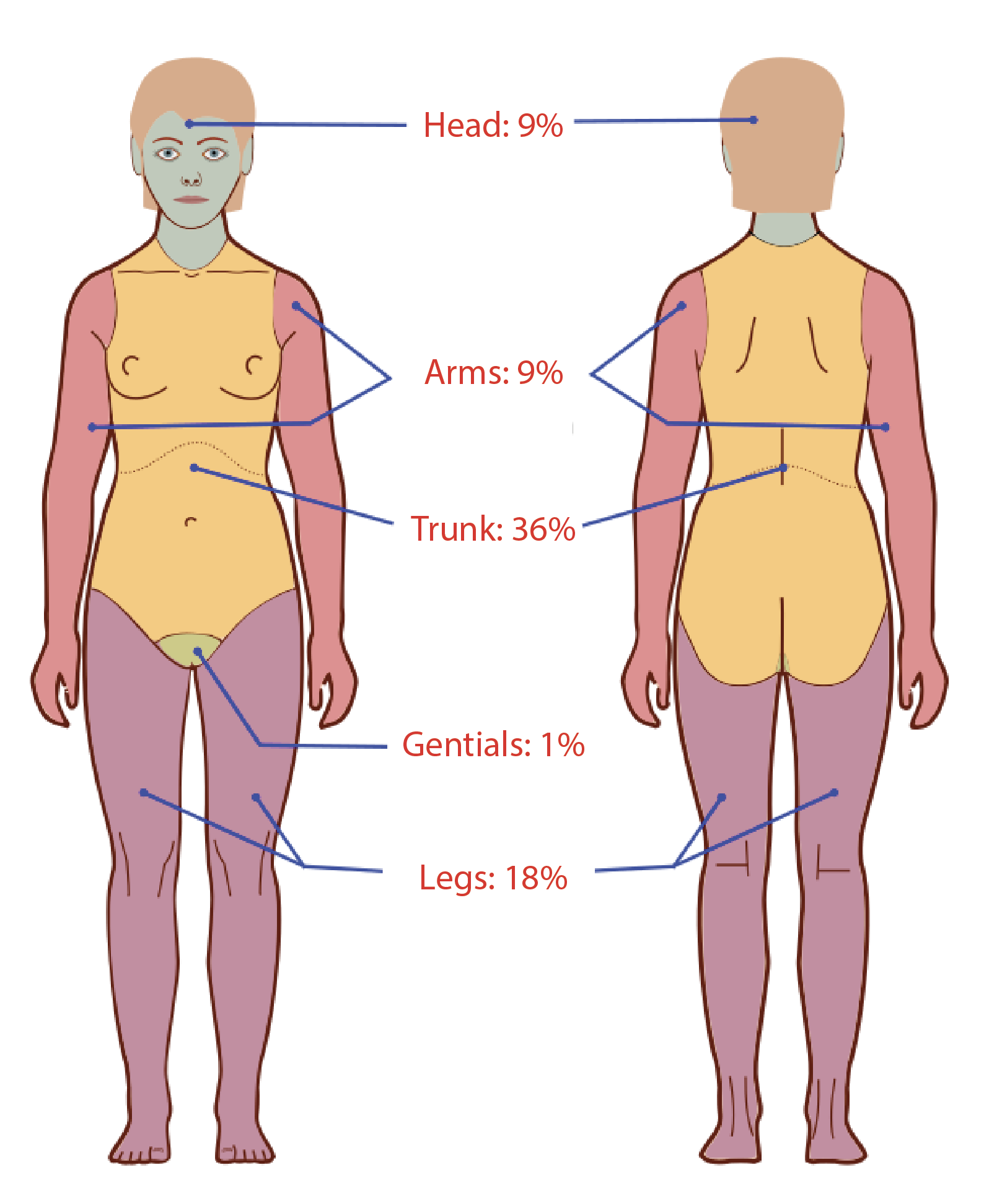
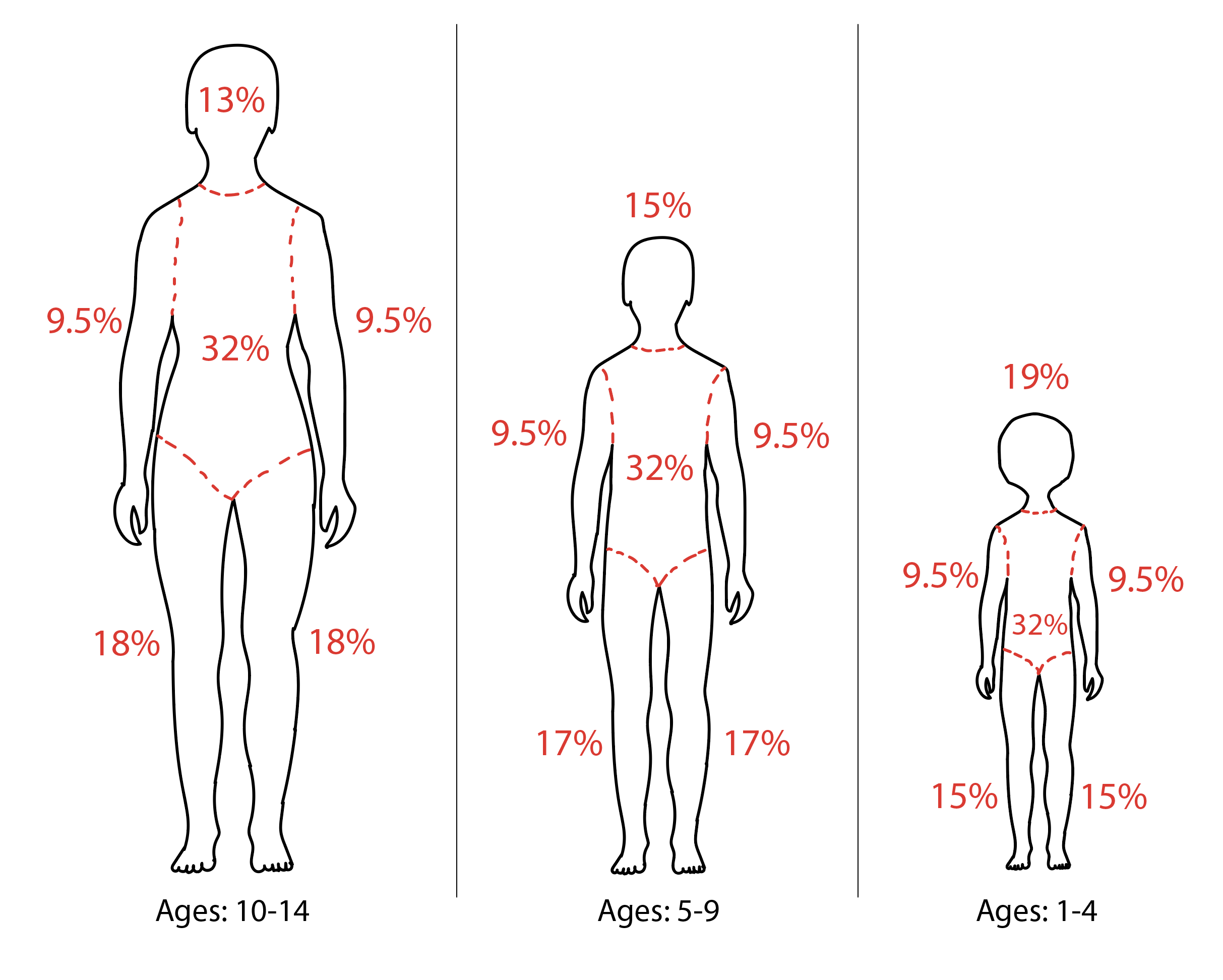
A full head-to-toe physical examination is vital to identify all burn injuries and signs of any concomitant trauma or inhalation injury (singed facial hairs, mucosal irritation, increased work of breathing, poor oxygenation on pulse oximetry). Identification of the depth and extent of the burn injuries will give significant insight into the required treatment. Superficial burns will have erythema and mild-moderate pain, but there will be no blistering. Superficial partial burns will have blisters and vesicles or sheared epidermis with wet, pink dermis that readily blanches with pressure. These burns will be very painful due to intact, irritating nerve endings. Deep partial burns will be less painful as many of the nerve endings are damaged and will have white, waxy, non-blanching dermis with no blisters or vesicles. Full-thickness burns will be painless with leathery, dry skin, thrombosed blood vessels, and possibly black eschar. Total body surface area (TBSA) of second-degree burns or deeper should be estimated using the Wallace rule of nines for adults or a credible pediatric burn assessment chart such as the Lund Browder Assessment scale to assist in burn resuscitation. Finally, any part of the body with circumferential partial to full-thickness burns must be monitored for compartment syndrome as they may need escharotomies or even formal fasciotomies. Signs of compartment syndrome in an extremity include early pain out of proportion to exam, paresthesias, poikilothermia and late paralysis, and lack of pulse.
Evaluation
On evaluation, imaging for any suspected trauma according to ATLS protocol as well as labs to assess end-organ health, electrolyte status, and nutritional status including complete blood count, complete metabolic profile, prothrombin time/international normalized ratio, and pre-albumin should be obtained. A urine drug screen in this patient population is important as well as a pregnancy test for women of childbearing age. Elevated carboxyhemoglobin levels can indicate carbon monoxide poisoning and give insight into possible inhalation injury and impending respiratory failure. However, be aware that the half-life of carboxyhemoglobin has been shown to be four hours or shorter in a patient on 100% oxygen, and therefore low levels taken several hours after injury do not necessarily rule out inhalation injury.[6][7][8][9]
Treatment / Management
Assessment and stabilization of the burn patient's airway, breathing, and circulation according to ATLS guidelines should be the first step to treating any burn patient, as they are first and foremost considered trauma patients. Appropriate supportive care including resuscitation with crystalloids, blood products, and possibly endotracheal intubation. After initial stabilization, appropriate assessment for transfer to an accredited burn center must be considered. Indications for transfer include TBSA of partial-thickness or deeper burns of 10% or greater, burns involving the face, hands/feet, genitalia/perineum, or major joints, chemical or electrical burns, large burns with concomitant trauma, inhalation injury, large burns in patients with special social or rehabilitation needs or significant medical problems that affect mortality, and if the evaluating hospital is without qualified personnel/equipment to care for pediatric burns. [10][11][12](B3)
Initial TBSA calculation will guide the need for resuscitation and resuscitation fluid rates. Burn resuscitation may be the most important and also one of the most controversial elements of burn care, with many differing opinions among experts. The 2012 American Burn Association Consensus acknowledges 20% TBSA as criteria for requiring formal resuscitation but also recognizes that pediatric burns may need different criteria, and many institutions have individualized guidelines for this patient population. They also acknowledge that there is insufficient evidence that more expensive colloid resuscitation is advantageous than crystalloid resuscitation. The most popular burn resuscitation formulas are the Parkland formula (4-times %TBSA x weight in kg) and the newer Modified Brooke formula (2-times %TBSA x weight in kg). They both calculate a number with units in milliliters. The first half of this calculated volume is divided evenly over the first 8 hours and the second half is divided evenly over the second 16 hours. Both original formulas advocated the use of colloid but more recently lactated ringers have been the resuscitation fluid of choice. After initial resuscitation rates are calculated, both formulas also advocate titration of rates to markers of physiologic response such as urine output of 0.5-1cc/kg/hr, and one should be aware that over-resuscitation can be as detrimental as under-resuscitation.
There is significant variation in burn wound care regimens, but all follow several basic principles. Adequate wound care serves to prevent infection, allows for slow mechanical removal of devitalized tissue, helps prevent fluid loss, and is cost-effective. Common classic topical antibacterial regimens from least to most tissue penetrance include silver nitrate, silver sulfadiazine, and mafenide acetate. The most commonly used is silver sulfadiazine as it has a good penetrance, good antibiotic spectrum against gram positives and negatives, and is less painful than mafenide acetate. Silver nitrate, with activity against Staph species and Pseudomonas, is generally used for superficial burns in patients with Sulfa allergies. Mafenide acetate, which is highly effective against gram negatives and has deep tissue penetrance, is generally reserved for very deep, heavily contaminated wounds, those with eschar, and auricular burns due to its superior cartilage penetration.
For deep partial or full thickness burns, surgical excision of damaged tissue and split-thickness skin grafting for wound closure are indicated. While it is possible for a deep partial or full-thickness burn to heal without surgery, these wounds generally take 3 weeks or longer to heal. This prolonged wound healing process predisposes the patient to wound infection, hypertrophic scarring, and the formation of scar contractures. With excision and grafting by ten days following the burn injury, a patient can heal the wound within 7 to 10 days postoperatively and decrease the risk of infection or scar significantly. For larger % TBSA burns, early removal of the burn injury, and closure of the wounds with a skin graft or skin substitute allow for a significant decrease in systemic inflammation and assist in temperature regulation and fluid management. Of note, deeper wounds may require surgical excision and placement of a dermal substitute before a skin grafting procedure.[13][14][15](B3)
Differential Diagnosis
There are two main differential diagnoses of thermal burn injuries and these should always be ruled out. These are:
- Cellulitis
- Toxic Epidermal Necrolysis (TEN)
Prognosis
Thermal burn injuries are a significant problem with high associated morbidity and mortality. Those associated with inhalational trauma (IHT) may be associated with higher mortality, but studies on prognosis are small and underpowered. It seems that %TBSA, presence of IHT, and age are the best predictors of mortality among the current published literature on burn prognosis.
Complications
Thermal burn wounds are prone to becoming infected and these infections are often the source of bacteria responsible for other systemic infections, including bloodstream infections and pneumonia. This can lead to sepsis, multisystem organ failure, and death.[16] Anxiety and depression also result from the disfigurement due to burns.
Deterrence and Patient Education
The best thing to minimize the damage caused by the burn is to properly manage the burn wound while at the incident site and on the way to the hospital. The following measures should be taken to lessen the damage:
- Stop the burning process.
- Remove all burned clothes. Hot clothing may cause a deeper injury. If clothing sticks to the skin, cut or tear around it.
- Pour cool water over burned areas. Do this for 3 to 5 minutes (30 to 40 minutes for a chemical burn).
- Do not pack the burned areas in ice. This may cause more damage and hypothermia.
- Remove all jewelry, belts, and tight clothing. Burned areas will swell immediately. If the victim’s neck is burned, make sure nothing is around it.
- Do not apply ointments or other home remedies to bad burns. These may cause serious infections.
- Cover burns with a clean, dry bandage or sheet.
- Keep the victim warm.
- Seek medical attention immediately.
Enhancing Healthcare Team Outcomes
An interprofessional approach is necessary for successful thermal burn care. Patients can require several surgeries over their lifetime for improvement of scar contractures and aesthetic outcomes, and plastic and general surgeons that take an interest in burn care will often keep relationships with patients throughout their careers. Postoperative physical and occupational therapy is often required to prevent contracture formation. A dietary consult is required as many patients may require high calories. The wound care nurse is essential for routine wound care and dressing changes. Case managers must assist in socioeconomic needs, and psychiatrists or psychologists who specialize in burn care can offer great comfort in this time of physical, emotional, and economic hardship. Success in burn care requires more than a thorough knowledge of treatment guidelines but also the dedication to bring all of these specialties together for a common goal.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Jayawardena A, Lowery AS, Wootten C, Dion GR, Summitt JB, McGrane S, Gelbard A. Early Surgical Management of Thermal Airway Injury: A Case Series. Journal of burn care & research : official publication of the American Burn Association. 2019 Feb 20:40(2):189-195. doi: 10.1093/jbcr/iry059. Epub [PubMed PMID: 30445620]
Level 2 (mid-level) evidenceMoore EC, Pilcher DV, Bailey MJ, Stephens H, Cleland H. The Burns Evaluation and Mortality Study (BEAMS): predicting deaths in Australian and New Zealand burn patients admitted to intensive care with burns. The journal of trauma and acute care surgery. 2013 Aug:75(2):298-303. doi: 10.1097/TA.0b013e318295409d. Epub [PubMed PMID: 23887563]
Level 2 (mid-level) evidenceMoore EC, Pilcher DV, Bailey MJ, Cleland H, McNamee J. A simple tool for mortality prediction in burns patients: APACHE III score and FTSA. Burns : journal of the International Society for Burn Injuries. 2010 Nov:36(7):1086-91. doi: 10.1016/j.burns.2010.03.013. Epub 2010 May 21 [PubMed PMID: 20494521]
Level 2 (mid-level) evidenceSaffle JR, Sullivan JJ, Tuohig GM, Larson CM. Multiple organ failure in patients with thermal injury. Critical care medicine. 1993 Nov:21(11):1673-83 [PubMed PMID: 8222683]
Level 2 (mid-level) evidenceGlik J, Cholewka A, Stanek A, Englisz B, Sieroń K, Mikuś-Zagórska K, Knefel G, Nowak M, Kawecki M. Thermal imaging and planimetry evaluation of the results of chronic wounds treatment with hyperbaric oxygen therapy. Advances in clinical and experimental medicine : official organ Wroclaw Medical University. 2019 Feb:28(2):229-236. doi: 10.17219/acem/92304. Epub [PubMed PMID: 30238703]
Level 3 (low-level) evidenceSchaefer TJ, Nunez Lopez O. Burn Resuscitation and Management. StatPearls. 2024 Jan:(): [PubMed PMID: 28613546]
Schaefer TJ, Szymanski KD. Burn Evaluation and Management. StatPearls. 2024 Jan:(): [PubMed PMID: 28613492]
Zuo KJ, Medina A, Tredget EE. Important Developments in Burn Care. Plastic and reconstructive surgery. 2017 Jan:139(1):120e-138e. doi: 10.1097/PRS.0000000000002908. Epub [PubMed PMID: 28027250]
Vivó C, Galeiras R, del Caz MD. Initial evaluation and management of the critical burn patient. Medicina intensiva. 2016 Jan-Feb:40(1):49-59. doi: 10.1016/j.medin.2015.11.010. Epub 2015 Dec 24 [PubMed PMID: 26724246]
Ramachandra T, Ries WR. Management of Nasal and Perinasal Soft Tissue Injuries. Facial plastic surgery : FPS. 2015 Jun:31(3):194-200. doi: 10.1055/s-0035-1555619. Epub 2015 Jun 30 [PubMed PMID: 26126216]
Wu C, Calvert CT, Cairns BA, Hultman CS. Lower extremity nerve decompression in burn patients. Annals of plastic surgery. 2013 May:70(5):563-7. doi: 10.1097/SAP.0b013e31827aef9c. Epub [PubMed PMID: 23542842]
Level 3 (low-level) evidenceToussaint J, Singer AJ. The evaluation and management of thermal injuries: 2014 update. Clinical and experimental emergency medicine. 2014 Sep:1(1):8-18 [PubMed PMID: 27752547]
Fish R, Davidson RS. Management of ocular thermal and chemical injuries, including amniotic membrane therapy. Current opinion in ophthalmology. 2010 Jul:21(4):317-21. doi: 10.1097/ICU.0b013e32833a8da2. Epub [PubMed PMID: 20467317]
Level 3 (low-level) evidenceBayat A, Ramaiah R, Bhananker SM. Analgesia and sedation for children undergoing burn wound care. Expert review of neurotherapeutics. 2010 Nov:10(11):1747-59. doi: 10.1586/ern.10.158. Epub [PubMed PMID: 20977331]
Trupkovic T, Giessler G. [Burn trauma. Part 1: pathophysiology, preclinical care and emergency room management]. Der Anaesthesist. 2008 Sep:57(9):898-907. doi: 10.1007/s00101-008-1428-5. Epub [PubMed PMID: 18716752]
Shankar R, Melstrom KA Jr, Gamelli RL. Inflammation and sepsis: past, present, and the future. Journal of burn care & research : official publication of the American Burn Association. 2007 Jul-Aug:28(4):566-71. doi: 10.1097/BCR.0B013E318093DF16. Epub [PubMed PMID: 17665516]