Introduction
Papillary thyroid carcinoma (PTC) is an epithelial malignancy showing evidence of follicular cell differentiation and distinctive nuclear features. It is the most frequent thyroid neoplasm and carries the best overall prognosis. The tumor usually appears as an irregular solid mass but may have cystic features in rare cases. One key feature of PTC is its ability to invade adjacent structures like lymphatics. About 10% of patients may present with metastatic disease at initial presentation. The overall prognosis is good for most patients, especially the ones younger than 45 years of age.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Known risk factors for PTC include:
Radiation Exposure
The incidence of papillary thyroid cancer is greater in people with a history of exposure to significant ionizing radiation.
Childhood Exposure
External low-dose radiation therapy to the head and neck during childhood, used in the 1940s to 1960s to treat various benign diseases, predisposes to PTC. The average time from irradiation to tumor recognition is approximately 10 years but may be longer than 30 years.[1] Medical Therapy
High radiation doses (> 2000 cGy) used in treating malignant diseases have also been associated with an increased risk of PTC. Environmental Exposure
The Chornobyl nuclear accident, which occurred on April 26, 1986, led to a 3- to 75-fold increase in the incidence of PTC in fallout regions, especially in younger children.
Genetics
A few familial syndromes are associated with PTC, including familial adenomatous polyposis—Gardner syndrome, Werner syndrome, and Carney complex type 1. Familial PTC cases have been reported in 5% of all patients with PTC and may portend a more aggressive disease course.[2]
Other
PTC is higher in regions with high dietary iodine intake and patients with preexisting benign thyroid disease.[3] There is also a trend for an increased incidence of thyroid cancer due to being overweight or obese, as shown in a report studying the changes in the frequency of thyroid cancer between 1995 and 2015.[4]
Epidemiology
PTC is the predominant form of thyroid cancer, accounting for 80 to 85% of all thyroid cancer cases. In a report based on the Surveillance, Epidemiology, and End Results (SEER) database from 1975 to 2012, the incidence of PTC increased from 4.8 to 14.9 per 100,000.[5][6][7] A recent report of autopsy results showed no difference in the prevalence of subclinical thyroid cancer through lifespan and different age groups.[8] One of the latest thoughts in the medical community is that there is an obvious overdiagnosis of thyroid cancer in general that might even result in overtreatment without necessarily changing the ultimate prognosis and mortality from the disease.[9] The overdiagnosis is usually due to frequent incidental finding of microcancers of the thyroid gland in routine imaging studies, and the overtreatment is due to the slow-changing mentality of the medical force that is still using aggressive surgical therapy as definite treatment of thyroid cancer versus the newest more conservative approach of observation or more limited surgical intervention. PTC occurs predominantly in middle-aged adults with a 3 to 1 female-to-male ratio; the median age at presentation is 50 years. Even though rare in children, PTC is still the most common pediatric thyroid malignancy. It affects Whites more commonly than Blacks.[10]
Pathophysiology
Chromosomal rearrangements have been identified in PTC, including the RET protooncogene, NTRK1, and MET gene overexpression.[11] Further, mutations in the BRAF gene have also been identified and correlated with prognosis, particularly BRAFV600E mutation.[12][13][14][15] A clear association between PTC and radiation exposure is now well established.
Histopathology
Gross Findings
Grossly, PTC typically presents as an invasive neoplasm with poorly defined margins, a firm consistency, and a granular white-cut surface. Calcifications may be present. The size is widely variable, with a mean diameter of 2-3 cm. PTC has 3 classification categories based on the size and extent of the primary lesion. Minimal carcinoma or occult carcinoma/micro-carcinoma tumors are 1.5 cm or smaller and show no evidence of invasiveness through the thyroid capsule or cervical lymph nodes. These lesions are typically nonpalpable and usually found as incidental findings during operative or autopsy examination. Intra-thyroid tumors are greater than 1.5 cm in diameter but remain confined to the thyroid gland with no evidence of extra-thyroid invasion. Extra-thyroid tumors extend through the thyroid capsule to involve the surrounding viscera.[16]
Microscopic Findings
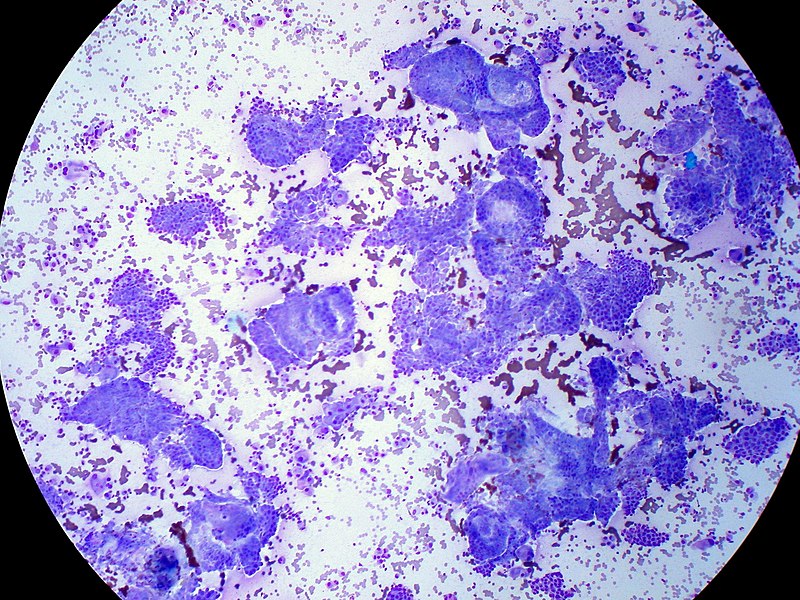
The 2 cardinal morphological features of conventional PTC are the papillae and the nuclear changes. The papillae comprise a central fibrovascular stalk covered by a neoplastic epithelial lining. The papillae may be long, straight, or arborizing, arranged in a parallel, regimented fashion, short and stubby, or tightly packed. The thickness and composition of the papillary stalk are variable. The stalk usually comprises loose connective tissue and variously sized thin-walled vessels.[17] The diagnosis of papillary carcinoma is based on the nuclear morphology of a thyroid neoplasm (see Image. Papillary Thyroid Carcinoma, FNA Giemsa Stain). The existence of multiple architectural variants proves the irrelevance of architecture.[17] The following constellation of features characterizes the diagnostic nuclear morphology:
- Enlarged and elongated nuclei with crowding and overlap
- Irregular nuclear contour
- Chromatin clearing with peripheral margination of chromatin, giving rise to what has been described as Orphan Annie Eye nuclei
- Multiple micro-nucleoli located immediately underneath the nuclear membrane
- Nuclear grooves resulting from an irregularity of nuclear contour seen in 2 dimensions
- Intranuclear cytoplasmic pseudo-inclusions from the accumulation of cytoplasm in prominent nuclear grooves
- Presence of psammoma bodies
Immunohistochemical Findings
Immunohistochemistry is seldom of value in diagnosing PTC, although it may play a role in metastatic disease. The neoplastic cells are strongly and diffusely immunoreactive with keratin, CK7, thyroglobulin, TTF1, and PAX8, while other markers (HBME-1, Galectin-3, S100 protein, CITED1, CK19) yield variable results.[18]
History and Physical
PTC usually presents as an asymptomatic (painless) thyroid mass with or without enlargement of regional (cervical) lymph nodes. Hoarseness and dysphagia occur in approximately 20% of cases, signaling recurrent laryngeal nerve involvement with vocal cord paralysis or tracheal compression. Nodal metastases in the lateral neck are reported in 27% of patients at presentation, most often originating from tumors in the ipsilateral thyroid lobe.[19] In rare cases, there could be lateral lymph node involvement.[20] The examination reveals a painless hard lesion, usually less than 5 cm. The mass is often fixed and has irregular borders.
Evaluation
Fine Needle Aspiration (FNA)
It is frequently the initial diagnostic method used in the detection of PTC. Fine-needle aspiration specimens from conventional PTC are usually cellular. They may show papillary structures, monolayer sheets, and 3D groups in a background of watery or thick so-called ropy colloid, nuclear or calcific debris, macrophages, and stromal fragments. The individual tumor cells with eosinophilic cytoplasm are enlarged, elongated, or oval. The nuclei show elongation, membrane thickening, chromatin clearing, grooves, and pseudo-inclusions. These tumors usually show enlarged follicular cells arranged in monolayer sheets and follicular groups in a thin and thick colloid background.[21][22]
Laboratory Tests
Thyroid function testing has limited utility in diagnosing PTC because most patients have normal thyroid function.[23]
Radiographic Features
On thyroid scans, PTCs typically appear as cold (hypo-functioning) nodules but rarely can appear as hot (hyperfunctioning) nodules. Ultrasound examination is the imaging modality of choice for PTC. Sonographic features include a hypoechoic or isoechoic solid nodule with irregular or poorly defined margins, micro-calcifications, taller-than-wide shape, and disorganized internal vascularity. Ultrasound findings are also invaluable for guiding fine-needle aspiration biopsy of abnormal nodes. Microcalcifications are highly specific for this type of cancer. Other imaging modalities, including CT, MRI, and FDG-PET/CT, may be needed to assess the extent of extra-thyroidal extension, evaluate the presence of substernal masses, detect recurrent tumors, and improve diagnostic accuracy.[24]
Treatment / Management
Surgery
Primary treatment decisions have as their basis a preoperative risk assessment that includes clinical, imaging, and cytological data.[25] Choices depend on the location and extent of identifiable disease and the risk that unidentifiable disease foci are also present. With increasing emphasis on risk-stratified management, the treatment approaches recommended by the 2015 ATA guidelines are more conservative than in the past.[26][27][28] Small-size papillary cancers can be followed conservatively with active surveillance and without any intervention, and surgery can be pursued only if there is a significant change in size or internal features of the tumor.[29][30] A recent study showed that there is still an adjustment period among physicians who are still recommending more aggressive treatment choices despite the current changes.[31][32](A1)
A lobectomy is an option for unifocal tumors smaller than 4 cm with no evidence of extrathyroidal extension or lymph node metastasis. For patients with PTC >4 cm, or with gross extra-thyroidal extension (clinical T4), or clinically apparent metastatic disease to nodes (clinical N1) or distant sites (clinical M1), the initial surgical procedure should include a near-total or total thyroidectomy and gross removal of all primary tumor unless there are contraindications to this procedure. If surgery is chosen for patients with thyroid cancer <1 cm without extra-thyroidal extension and cN0, the initial surgical procedure should be a thyroid lobectomy unless there are clear indications to remove the contralateral lobe. Thyroid lobectomy alone is sufficient treatment for small, unifocal, intrathyroidal carcinomas in the absence of prior head and neck radiation, familial thyroid carcinoma, or clinically detectable cervical nodal metastases.[26][33] Prophylactic central-compartment neck dissection (ipsilateral or bilateral) should be considered in patients with PTC with clinically uninvolved central neck lymph nodes (cN0) who have advanced primary tumors (T3 or T4) or clinically involved lateral neck nodes (cN1b) or if the information be used to plan further steps in therapy.
Adjuvant Radioiodine Therapy
After thyroidectomy, radioiodine is the therapy of choice in patients with PTC to ablate residual normal thyroid tissue.
Radioiodine therapy is indicated in several cases.[34] These include:(B2)
- Patients with a tumor >2 cm and 1 of the following risk factors: gross extra-thyroidal extension, age > 45 years, lymph node and distant metastases
- Patients with a tumor <2 cm and distant metastasis
Radioactive iodine therapy is given 4 to 6 weeks after surgery. Before treatment, a hypothyroid state is induced by stopping thyroid hormone replacement treatment. The therapy is continued until no more radioactive iodine uptake is seen. Potential adverse effects of radioactive iodine include:
- Sialoadenitis
- Transient thyrotoxicosis
- Pulmonary fibrosis
- Emesis
- Brain edema (can be prevented with the use of corticosteroids)
- Infertility
- There is a small risk of leukemia, breast or bladder cancer
Thyroid Hormone Treatment
After thyroidectomy, patients require lifelong thyroid hormone therapy, usually as monotherapy with levothyroxine (LT4). Since TSH can promote the growth of remaining PTC cells, the dosage of LT4 should initially be high enough to achieve suppression of thyrotropin. The thyroid function should be checked after 6 to 8 weeks. Depending on the result, the dosage should be adjusted; the use of TSH suppressive therapy should merit careful consideration since it carries an increased risk of complications.[26]
NCCN Guidelines for Total Thyroidectomy
- Known distant metastases
- History of radiation
- Extrathyroidal extension
- Bilateral nodules
- The tumor measures more than 4 cm
- Poorly differentiate lesion
- Positive cervical lymph nodes
Routine cervical node dissection continues to be debated. Some literature notes fewer recurrences, but other studies have noted a higher incidence of recurrent nerve injury.
New Developments
New techniques have been tried for initially treating smaller-size papillary thyroid cancer with good results, like thermal ablation and ultrasound radiofrequency ablation for treating recurrent disease.[35][36] (A1)
Chemotherapy
This is reserved for patients with recurrent or excessive remnant disease after the initial surgical treatment and radioactive iodine ablation. The most common agents used are the kinase inhibitors that target different pathways, like the anti-angiogenic multi-targeted kinase inhibitors (aaMKI- lenvatinib, sorafenib), BRAF kinase inhibitors (vemurafenib, dabrafenib), MEK inhibitors (trametinib, cobimetinib), NTR kinase inhibitors (larotrectinib), and RET inhibitors (selpercatinib).[37][38][39]
Differential Diagnosis
The primary differential diagnoses of PTC are:
- Reactive changes following fine-needle aspiration.[40] This condition characteristically shows nuclear enlargement, chromatin clearing, and micro-nucleoli similar to the nuclei of PTC.
- Severe chronic lymphocytic thyroiditis, where the reactive atypia is attributed to inflammation, results in nuclear morphology similar to that of PTC.[41]
- Adenomatoid nodules
- Diffuse hyperplasia
- Dyshormonogenetic goiter
- Follicular adenoma
- Follicular thyroid carcinoma
- Medullary thyroid carcinoma
- Metastatic tumors
Staging
Several staging systems have been proposed for PTC and continue to evolve.[42][43] The most commonly used are:
For patients less than 45 years:
- Stage l: any Tm, any N, M0 (cancer localized to the thyroid)
- Stage ll: Any T, any N, M1 (cancer spread to cervical nodes or distant organs)
For patients older than 45 years:
- Stage l: T1, N0, M0 (cancer less than 2 cm)
- Stage ll: T2, N0, M0, and T3 (cancer localized to the thyroid that is between 2 to 4 cm)
- Stage lll: T4, N0, M0, and any T, N1, M0 (lesion more than 4 cm and spread limited to the neck)
- Stage lV: Any T, any N, M1 (cancer spread outside the neck and to distant organs)
Prognosis
Although PTC frequently metastasizes to regional lymph nodes, it generally carries an excellent prognosis. There are, however, several clinicopathological and background features that can lead to a poor prognosis.[44][45][46][47]
Poor prognostic factors of PTC include:
- Older age at diagnosis
- Large tumor size
- Extra-thyroidal growth
- Male sex
- Less differentiated or solid areas, vascular invasion, and aneuploid cell population
- Subtypes of PTC that are associated with a more aggressive clinical behavior like the tall cell variant, a diffuse sclerosis variant, the solid variant, and the follicular variant
Complications
Extra-thyroidal Extension
Extra-thyroidal extension occurs in 8% to 32% of the cases.[48]
Local or Regional Recurrences
Local or regional recurrences occur in 5 to 15% of patients with PTC.[49]
Distant Metastases
Distant metastasis occurs in only 1% to 25%, mainly in the lungs and bones. Other less common sites are the brain, liver, and skin.[50]
Postoperative and Rehabilitation Care
Long-term monitoring is necessary every 6 to 12 months for at least 5 years and annually thereafter to look for recurrence. During those visits, TSH, thyroglobulin, and antithyroglobulin antibodies should be measured.
Deterrence and Patient Education
Patients need to know the extent of the thyroid cancer, as well as the appropriate follow-up routine. Reassurance should be offered about the ultimate good prognosis so patients feel less stressed and avoid the stigma of cancer.
Enhancing Healthcare Team Outcomes
Papillary thyroid cancer is ideally managed by an interprofessional team that consists of an endocrinologist, general surgeon, oncologist, radiation oncologist, nuclear medicine clinician, internist, pharmacist (oncology or nuclear medicine specialized), and specialty care nurse. Most patients present to the primary care provider or nurse practitioner with a painless mass in the neck. Once the FNA is performed, the patient should be referred to an endocrinologist and a surgeon. Patients need to know that the sole treatment for PTC is surgery. Patients treated with radioactive iodine need to be educated about this therapy and warned about the potential adverse effects. Following surgery, all patients require long-term monitoring for recurrence. Most patients require long-term thyroid hormone replacement. Specialty care nurses in endocrinology or oncology assist with treatment, monitor and educate patients, and provide updates to the team. Pharmacists assist with nuclear medicine and chemotherapy, as well as hormone replacement therapy following treatment measures. Best practices require open communication among all team members, particularly if they note a change or deterioration in the patient's condition. This includes accurate and updated patient records so everyone involved in care can access the latest patient data. This interprofessional care model yields the best patient results. With early diagnosis and prompt treatment, the prognosis for most patients with PTC is excellent.
Media
(Click Image to Enlarge)
References
Mao XC, Yu WQ, Shang JB, Wang KJ. Clinical characteristics and treatment of thyroid cancer in children and adolescents: a retrospective analysis of 83 patients. Journal of Zhejiang University. Science. B. 2017 May:18(5):430-436. doi: 10.1631/jzus.B1600308. Epub [PubMed PMID: 28471115]
Level 2 (mid-level) evidenceMileva M, Stoilovska B, Jovanovska A, Ugrinska A, Petrushevska G, Kostadinova-Kunovska S, Miladinova D, Majstorov V. Thyroid cancer detection rate and associated risk factors in patients with thyroid nodules classified as Bethesda category III. Radiology and oncology. 2018 Sep 27:52(4):370-376. doi: 10.2478/raon-2018-0039. Epub 2018 Sep 27 [PubMed PMID: 30265655]
Kim K, Cho SW, Park YJ, Lee KE, Lee DW, Park SK. Association between Iodine Intake, Thyroid Function, and Papillary Thyroid Cancer: A Case-Control Study. Endocrinology and metabolism (Seoul, Korea). 2021 Aug:36(4):790-799. doi: 10.3803/EnM.2021.1034. Epub 2021 Aug 11 [PubMed PMID: 34376043]
Level 2 (mid-level) evidenceKitahara CM, Pfeiffer RM, Sosa JA, Shiels MS. Impact of Overweight and Obesity on US Papillary Thyroid Cancer Incidence Trends (1995-2015). Journal of the National Cancer Institute. 2020 Aug 1:112(8):810-817. doi: 10.1093/jnci/djz202. Epub [PubMed PMID: 31638139]
Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006 May 10:295(18):2164-7 [PubMed PMID: 16684987]
Level 2 (mid-level) evidenceCasella C, Fusco M. Thyroid cancer. Epidemiologia e prevenzione. 2004 Mar-Apr:28(2 Suppl):88-91 [PubMed PMID: 15281612]
Level 2 (mid-level) evidenceKitahara CM, Sosa JA, Shiels MS. Influence of Nomenclature Changes on Trends in Papillary Thyroid Cancer Incidence in the United States, 2000 to 2017. The Journal of clinical endocrinology and metabolism. 2020 Dec 1:105(12):e4823-30. doi: 10.1210/clinem/dgaa690. Epub [PubMed PMID: 32984898]
Arroyo N, Bell KJL, Hsiao V, Fernandes-Taylor S, Alagoz O, Zhang Y, Davies L, Francis DO. Prevalence of Subclinical Papillary Thyroid Cancer by Age: Meta-analysis of Autopsy Studies. The Journal of clinical endocrinology and metabolism. 2022 Sep 28:107(10):2945-2952. doi: 10.1210/clinem/dgac468. Epub [PubMed PMID: 35947867]
Level 1 (high-level) evidenceKrajewska J, Kukulska A, Oczko-Wojciechowska M, Kotecka-Blicharz A, Drosik-Rutowicz K, Haras-Gil M, Jarzab B, Handkiewicz-Junak D. Early Diagnosis of Low-Risk Papillary Thyroid Cancer Results Rather in Overtreatment Than a Better Survival. Frontiers in endocrinology. 2020:11():571421. doi: 10.3389/fendo.2020.571421. Epub 2020 Oct 6 [PubMed PMID: 33123090]
Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in Thyroid Cancer Incidence and Mortality in the United States, 1974-2013. JAMA. 2017 Apr 4:317(13):1338-1348. doi: 10.1001/jama.2017.2719. Epub [PubMed PMID: 28362912]
Rogucki M, Buczyńska A, Krętowski AJ, Popławska-Kita A. The Importance of miRNA in the Diagnosis and Prognosis of Papillary Thyroid Cancer. Journal of clinical medicine. 2021 Oct 15:10(20):. doi: 10.3390/jcm10204738. Epub 2021 Oct 15 [PubMed PMID: 34682861]
Tao Y, Wang F, Shen X, Zhu G, Liu R, Viola D, Elisei R, Puxeddu E, Fugazzola L, Colombo C, Jarzab B, Czarniecka A, Lam AK, Mian C, Vianello F, Yip L, Riesco-Eizaguirre G, Santisteban P, O'Neill CJ, Sywak MS, Clifton-Bligh R, Bendlova B, Sýkorová V, Zhao S, Wang Y, Xing M. BRAF V600E Status Sharply Differentiates Lymph Node Metastasis-associated Mortality Risk in Papillary Thyroid Cancer. The Journal of clinical endocrinology and metabolism. 2021 Oct 21:106(11):3228-3238. doi: 10.1210/clinem/dgab286. Epub [PubMed PMID: 34273152]
Ge J, Wang J, Wang H, Jiang X, Liao Q, Gong Q, Mo Y, Li X, Li G, Xiong W, Zhao J, Zeng Z. The BRAF V600E mutation is a predictor of the effect of radioiodine therapy in papillary thyroid cancer. Journal of Cancer. 2020:11(4):932-939. doi: 10.7150/jca.33105. Epub 2020 Jan 1 [PubMed PMID: 31949496]
Celik M, Bulbul BY, Ayturk S, Durmus Y, Gurkan H, Can N, Tastekin E, Ustun F, Sezer A, Guldiken S. The relation between BRAFV600E mutation and clinicopathological characteristics of papillary thyroid cancer. Medicinski glasnik : official publication of the Medical Association of Zenica-Doboj Canton, Bosnia and Herzegovina. 2020 Feb 1:17(1):30-34. doi: 10.17392/1086-20. Epub [PubMed PMID: 31994851]
Jensen K, Thakur S, Patel A, Mendonca-Torres MC, Costello J, Gomes-Lima CJ, Walter M, Wartofsky L, Burman KD, Bikas A, Ylli D, Vasko VV, Klubo-Gwiezdzinska J. Detection of BRAFV600E in Liquid Biopsy from Patients with Papillary Thyroid Cancer Is Associated with Tumor Aggressiveness and Response to Therapy. Journal of clinical medicine. 2020 Aug 2:9(8):. doi: 10.3390/jcm9082481. Epub 2020 Aug 2 [PubMed PMID: 32748840]
Choi JB, Lee SG, Kim MJ, Kim TH, Ban EJ, Lee CR, Lee J, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS. Oncologic outcomes in patients with 1-cm to 4-cm differentiated thyroid carcinoma according to extent of thyroidectomy. Head & neck. 2019 Jan:41(1):56-63. doi: 10.1002/hed.25356. Epub 2018 Dec 10 [PubMed PMID: 30536465]
Al-Brahim N, Asa SL. Papillary thyroid carcinoma: an overview. Archives of pathology & laboratory medicine. 2006 Jul:130(7):1057-62 [PubMed PMID: 16831036]
Level 3 (low-level) evidenceCho H, Kim JY, Oh YL. Diagnostic value of HBME-1, CK19, Galectin 3, and CD56 in the subtypes of follicular variant of papillary thyroid carcinoma. Pathology international. 2018 Nov:68(11):605-613. doi: 10.1111/pin.12729. Epub 2018 Oct 23 [PubMed PMID: 30350394]
Rahmat F, Kumar Marutha Muthu A, S Raja Gopal N, Jo Han S, Yahaya AS. Papillary Thyroid Carcinoma as a Lateral Neck Cyst: A Cystic Metastatic Node versus an Ectopic Thyroid Tissue. Case reports in endocrinology. 2018:2018():5198297. doi: 10.1155/2018/5198297. Epub 2018 Oct 18 [PubMed PMID: 30420925]
Level 3 (low-level) evidenceZhao H, Huang T, Li H. Risk factors for skip metastasis and lateral lymph node metastasis of papillary thyroid cancer. Surgery. 2019 Jul:166(1):55-60. doi: 10.1016/j.surg.2019.01.025. Epub 2019 Mar 12 [PubMed PMID: 30876667]
Nasser SM, Pitman MB, Pilch BZ, Faquin WC. Fine-needle aspiration biopsy of papillary thyroid carcinoma: diagnostic utility of cytokeratin 19 immunostaining. Cancer. 2000 Oct 25:90(5):307-11 [PubMed PMID: 11038428]
Nishino M, Krane JF. Updates in Thyroid Cytology. Surgical pathology clinics. 2018 Sep:11(3):467-487. doi: 10.1016/j.path.2018.05.002. Epub [PubMed PMID: 30190135]
Suzuki S, Bogdanova TI, Saenko VA, Hashimoto Y, Ito M, Iwadate M, Rogounovitch TI, Tronko MD, Yamashita S. Histopathological analysis of papillary thyroid carcinoma detected during ultrasound screening examinations in Fukushima. Cancer science. 2019 Feb:110(2):817-827. doi: 10.1111/cas.13912. Epub 2019 Jan 20 [PubMed PMID: 30548366]
Gilmartin A, Ryan M. Incidence of Thyroid Cancer among Patients with Thyroid Nodules. Irish medical journal. 2018 Sep 10:111(8):802 [PubMed PMID: 30547520]
McLeod DSA, Zhang L, Durante C, Cooper DS. Contemporary Debates in Adult Papillary Thyroid Cancer Management. Endocrine reviews. 2019 Dec 1:40(6):1481-1499. doi: 10.1210/er.2019-00085. Epub [PubMed PMID: 31322698]
Haugen BR. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: What is new and what has changed? Cancer. 2017 Feb 1:123(3):372-381. doi: 10.1002/cncr.30360. Epub 2016 Oct 14 [PubMed PMID: 27741354]
Cho SJ, Suh CH, Baek JH, Chung SR, Choi YJ, Chung KW, Shong YK, Lee JH. Active Surveillance for Small Papillary Thyroid Cancer: A Systematic Review and Meta-Analysis. Thyroid : official journal of the American Thyroid Association. 2019 Oct:29(10):1399-1408. doi: 10.1089/thy.2019.0159. Epub 2019 Sep 27 [PubMed PMID: 31368412]
Level 1 (high-level) evidenceCoca-Pelaz A, Shah JP, Hernandez-Prera JC, Ghossein RA, Rodrigo JP, Hartl DM, Olsen KD, Shaha AR, Zafereo M, Suarez C, Nixon IJ, Randolph GW, Mäkitie AA, Kowalski LP, Vander Poorten V, Sanabria A, Guntinas-Lichius O, Simo R, Zbären P, Angelos P, Khafif A, Rinaldo A, Ferlito A. Papillary Thyroid Cancer-Aggressive Variants and Impact on Management: A Narrative Review. Advances in therapy. 2020 Jul:37(7):3112-3128. doi: 10.1007/s12325-020-01391-1. Epub 2020 Jun 1 [PubMed PMID: 32488657]
Level 3 (low-level) evidenceIñiguez-Ariza NM, Brito JP. Management of Low-Risk Papillary Thyroid Cancer. Endocrinology and metabolism (Seoul, Korea). 2018 Jun:33(2):185-194. doi: 10.3803/EnM.2018.33.2.185. Epub [PubMed PMID: 29947175]
Sawka AM, Ghai S, Yoannidis T, Rotstein L, Gullane PJ, Gilbert RW, Pasternak JD, Brown DH, Eskander A, Almeida JR, Irish JC, Higgins K, Enepekides DJ, Monteiro E, Banerjee A, Shah M, Gooden E, Zahedi A, Korman M, Ezzat S, Jones JM, Rac VE, Tomlinson G, Stanimirovic A, Gafni A, Baxter NN, Goldstein DP. A Prospective Mixed-Methods Study of Decision-Making on Surgery or Active Surveillance for Low-Risk Papillary Thyroid Cancer. Thyroid : official journal of the American Thyroid Association. 2020 Jul:30(7):999-1007. doi: 10.1089/thy.2019.0592. Epub 2020 Apr 8 [PubMed PMID: 32126932]
James BC, Timsina L, Graham R, Angelos P, Haggstrom DA. Changes in total thyroidectomy versus thyroid lobectomy for papillary thyroid cancer during the past 15 years. Surgery. 2019 Jul:166(1):41-47. doi: 10.1016/j.surg.2019.01.007. Epub 2019 Mar 21 [PubMed PMID: 30904172]
Vargas-Pinto S, Romero Arenas MA. Lobectomy Compared to Total Thyroidectomy for Low-Risk Papillary Thyroid Cancer: A Systematic Review. The Journal of surgical research. 2019 Oct:242():244-251. doi: 10.1016/j.jss.2019.04.036. Epub 2019 May 16 [PubMed PMID: 31103828]
Level 1 (high-level) evidenceGartland RM, Lubitz CC. Impact of Extent of Surgery on Tumor Recurrence and Survival for Papillary Thyroid Cancer Patients. Annals of surgical oncology. 2018 Sep:25(9):2520-2525. doi: 10.1245/s10434-018-6550-2. Epub 2018 May 31 [PubMed PMID: 29855833]
Tang J, Kong D, Cui Q, Wang K, Zhang D, Liao X, Gong Y, Wu G. The role of radioactive iodine therapy in papillary thyroid cancer: an observational study based on SEER. OncoTargets and therapy. 2018:11():3551-3560. doi: 10.2147/OTT.S160752. Epub 2018 Jun 19 [PubMed PMID: 29950860]
Level 2 (mid-level) evidenceCho SJ, Baek JH, Chung SR, Choi YJ, Lee JH. Thermal Ablation for Small Papillary Thyroid Cancer: A Systematic Review. Thyroid : official journal of the American Thyroid Association. 2019 Dec:29(12):1774-1783. doi: 10.1089/thy.2019.0377. Epub 2019 Dec 6 [PubMed PMID: 31739738]
Level 1 (high-level) evidenceChung SR, Baek JH, Choi YJ, Lee JH. Longer-term outcomes of radiofrequency ablation for locally recurrent papillary thyroid cancer. European radiology. 2019 Sep:29(9):4897-4903. doi: 10.1007/s00330-019-06063-5. Epub 2019 Feb 25 [PubMed PMID: 30805701]
Fallahi P, Ferrari SM, Galdiero MR, Varricchi G, Elia G, Ragusa F, Paparo SR, Benvenga S, Antonelli A. Molecular targets of tyrosine kinase inhibitors in thyroid cancer. Seminars in cancer biology. 2022 Feb:79():180-196. doi: 10.1016/j.semcancer.2020.11.013. Epub 2020 Nov 26 [PubMed PMID: 33249201]
Koehler VF, Berg E, Adam P, Weber GL, Pfestroff A, Luster M, Kutsch JM, Lapa C, Sandner B, Rayes N, Fuss CT, Kreissl MC, Hoster E, Allelein S, Schott M, Todica A, Fassnacht M, Kroiss M, Spitzweg C. Real-World Efficacy and Safety of Multi-Tyrosine Kinase Inhibitors in Radioiodine Refractory Thyroid Cancer. Thyroid : official journal of the American Thyroid Association. 2021 Oct:31(10):1531-1541. doi: 10.1089/thy.2021.0091. Epub [PubMed PMID: 34405734]
Wagner M, Wuest M, Lopez-Campistrous A, Glubrecht D, Dufour J, Jans HS, Wuest F, McMullen TPW. Tyrosine kinase inhibitor therapy and metabolic remodelling in papillary thyroid cancer. Endocrine-related cancer. 2020 Sep:27(9):495-507. doi: 10.1530/ERC-20-0135. Epub [PubMed PMID: 32590338]
LiVolsi VA, Merino MJ. Worrisome histologic alterations following fine-needle aspiration of the thyroid (WHAFFT). Pathology annual. 1994:29 ( Pt 2)():99-120 [PubMed PMID: 7936753]
Baloch ZW, LiVolsi VA. Fine-needle aspiration of thyroid nodules: past, present, and future. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2004 May-Jun:10(3):234-41 [PubMed PMID: 15310542]
Wong RM, Bresee C, Braunstein GD. Comparison with published systems of a new staging system for papillary and follicular thyroid carcinoma. Thyroid : official journal of the American Thyroid Association. 2013 May:23(5):566-74. doi: 10.1089/thy.2012.0181. Epub [PubMed PMID: 23106409]
Level 2 (mid-level) evidenceLoh KC, Greenspan FS, Gee L, Miller TR, Yeo PP. Pathological tumor-node-metastasis (pTNM) staging for papillary and follicular thyroid carcinomas: a retrospective analysis of 700 patients. The Journal of clinical endocrinology and metabolism. 1997 Nov:82(11):3553-62 [PubMed PMID: 9360506]
Level 2 (mid-level) evidenceIto Y, Miyauchi A, Kihara M, Fukushima M, Higashiyama T, Miya A. Overall Survival of Papillary Thyroid Carcinoma Patients: A Single-Institution Long-Term Follow-Up of 5897 Patients. World journal of surgery. 2018 Mar:42(3):615-622. doi: 10.1007/s00268-018-4479-z. Epub [PubMed PMID: 29349484]
Ulisse S, Baldini E, Lauro A, Pironi D, Tripodi D, Lori E, Ferent IC, Amabile MI, Catania A, Di Matteo FM, Forte F, Santoro A, Palumbo P, D'Andrea V, Sorrenti S. Papillary Thyroid Cancer Prognosis: An Evolving Field. Cancers. 2021 Nov 7:13(21):. doi: 10.3390/cancers13215567. Epub 2021 Nov 7 [PubMed PMID: 34771729]
Vuong HG, Le HT, Le TTB, Le T, Hassell L, Kakudo K. Clinicopathological significance of major fusion oncogenes in papillary thyroid carcinoma: An individual patient data meta-analysis. Pathology, research and practice. 2022 Dec:240():154180. doi: 10.1016/j.prp.2022.154180. Epub 2022 Oct 21 [PubMed PMID: 36306725]
Level 1 (high-level) evidenceLin P, Guo YN, Shi L, Li XJ, Yang H, He Y, Li Q, Dang YW, Wei KL, Chen G. Development of a prognostic index based on an immunogenomic landscape analysis of papillary thyroid cancer. Aging. 2019 Jan 20:11(2):480-500. doi: 10.18632/aging.101754. Epub [PubMed PMID: 30661062]
Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. The American journal of medicine. 1994 Nov:97(5):418-28 [PubMed PMID: 7977430]
DeGroot LJ, Kaplan EL, McCormick M, Straus FH. Natural history, treatment, and course of papillary thyroid carcinoma. The Journal of clinical endocrinology and metabolism. 1990 Aug:71(2):414-24 [PubMed PMID: 2380337]
Sebastian SO, Gonzalez JM, Paricio PP, Perez JS, Flores DP, Madrona AP, Romero PR, Tebar FJ. Papillary thyroid carcinoma: prognostic index for survival including the histological variety. Archives of surgery (Chicago, Ill. : 1960). 2000 Mar:135(3):272-7 [PubMed PMID: 10722027]