Introduction
The term thyroiditis reflects inflammation of the thyroid gland. Thyroiditis can be classified based on the onset of symptoms, underlying etiology, and clinical symptoms. The most common cause of thyroiditis is an autoimmune disease. In the United States, Hashimoto thyroiditis is the most common cause of hypothyroidism.[1] Thyroiditis can cause transient or permanent hypo and hyperthyroidism.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Thyroiditis can occur due to autoimmune disease (Hashimoto thyroiditis, Graves disease, postpartum thyroiditis or painless sporadic thyroiditis), infection (painful subacute thyroiditis or suppurative thyroiditis), drugs (amiodarone, lithium, interferons and interleukin-2; and checkpoint inhibitors) or fibrosis (Riedel thyroiditis)
Painful thyroiditis encompasses infectious, subacute thyroiditis, traumatic or radiation-induced thyroiditis, and painless thyroiditis encompass autoimmune, postpartum, and drug-induced thyroiditis.
It can be classified into acute, subacute, and chronic thyroiditis.
Acute thyroiditis is caused by bacterial infection of the gland.
Subacute, also known as granulomatous thyroiditis, is caused by viruses.
Chronic includes autoimmune thyroiditis, Hashimoto thyroiditis, postpartum thyroiditis, and other painless thyroiditis, including iatrogenic and drug-induced thyroiditis.
Acute Thyroiditis
Infectious thyroiditis: Infection of the thyroid gland is rare as it is encapsulated with rich blood supply and extensive lymphatic drainage. This is usually seen in the elderly, chronically ill and immunocompromised patients.[2] It is most commonly caused by gram-positive bacteria like Staphylococcus or Streptococcus. Sometimes mycobacteria and fungi, including pneumocystis, can be the culprit in immunocompromised patients. Source of infection is usually hematogenous or congenital abnormalities like pyriform sinus usually seen in children.
Radiation-induced thyroiditis: Radiation treatment of neck cancer can cause thyroiditis, followed by hypothyroidism. Patients who receive radioactive iodine for ablation of Graves disease occasionally develop severe thyroid pain 7 to 10 days after therapy. It is rare, and the incidence is about 1%.
Subacute Thyroiditis
It is usually preceded by upper respiratory tract infections and is presumed to be due to a viral illness, though definite evidence is lacking.[3] There is also a strong association with HLA -35.[4]
Chronic Thyroiditis
Autoimmune thyroiditis: It includes Hashimoto thyroiditis and postpartum thyroiditis and its association with HLA-DR3, HLA-DR4, HLA-DR5 has been reported in Whites.[5][6][7] Hashimoto thyroiditis is the most common cause of hypothyroidism in the United States. It is presumed to be due to a viral infection, with the viral structure being similar to thyroid protein leading to the production of antibodies against the thyroid gland. Approximately 10% of the general population in the US has a high concentration of these antibodies, but the majority of them have normal thyroid function tests.[8] However, there is a risk of progression to overt hypothyroidism in such individuals.
Postpartum thyroiditis: It is an autoimmune phenomenon where antibodies formed against fetal thyroid cells accumulate in the mother's thyroid gland.[9] It occurs in postpartum women within one year of childbirth. The maternal presence of positive thyroid peroxidase antibody or other autoimmune diseases is a risk factor.
Drug-induced thyroiditis: The most common drugs causing thyroid dysfunction are amiodarone, lithium, and tyrosine kinase inhibitors.
Amiodarone can cause both hyper and hypothyroidism. In euthyroid individuals, amiodarone can cause transient changes in thyroid function tests (TFT), followed by normalization. In patients who have underlying Hashimoto, or pregnant are at risk of developing worsening hypothyroidism. It is thought to be secondary to the antithyroid effect of the iodine in amiodarone. Amiodarone can induce hyperthyroidism in two ways. In type 1, there is increased synthesis and release of thyroid hormone, whereas, in type 2, there is destructive thyroiditis leading to the release of preformed T4 and T3 from the damaged thyroid gland.
Checkpoint inhibitors are a type of immunotherapy with anti-neoplastic properties and include drugs like nivolumab, ipilimumab, pembrolizumab, and atezolizumab. They are associated with endocrinopathies especially, hypothyroidism secondary to destructive thyroiditis.[10] Patients usually present with vague symptoms of hypothyroidism like fatigue, weight gain. It should be distinguished from secondary hypothyroidism as these drugs also cause hypophysitis. Hyperthyroidism though very rare, is also seen.
Lithium is known to cause hypothyroidism by decreasing the secretion of thyroid hormones. This causes a rise in TSH and eventually enlargement of the thyroid gland and goiter. About 15% of patients on interferon alfa therapy can develop thyroid dysfunction.[11] Thyroid abnormalities, including both hyper and hypothyroidism, can be seen in patients on tyrosine kinase inhibitors, especially sunitinib and lenvatinib.
Riedel thyroiditis: Reidel thyroiditis is a rare condition characterized by progressive fibrosis of the thyroid gland. The exact etiology is unclear, but recent data indicate that it is closely related to IgG-4 related sclerosing disease. The fibrosis of the thyroid gland may or may not be associated with progressive fibrosis of other organs.[12]
Epidemiology
Hashimoto thyroiditis is the most common cause of hypothyroidism, while Graves disease is the most common cause of autoimmune hyperthyroidism in the United States. High intake of iodine can increase the incidence of Graves disease, whereas iodine insufficiency can be protective against autoimmune thyroiditis.[13]
Pathophysiology
Acute Thyroiditis
Infectious thyroiditis is caused by gram-positive bacteria like streptococcus, staphylococcus, or fungi, mycoparasitic infection.[2]
The destruction of thyroid parenchyma causes radiation-induced thyroiditis after exposure to radioactive iodine for treatment of Graves disease or thyroid cancer and high dose radiation to the neck for the lymphoma and other head and neck cancers.
Subacute Thyroiditis
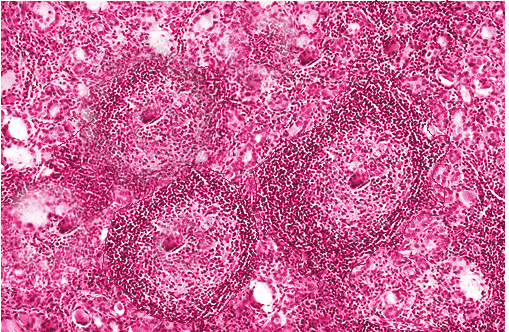
This is caused by viruses like coxsackie A, B, echovirus. Granulomas are formed in the thyroid gland, which becomes fibrotic but can return to normal after treatment.
Chronic Thyroiditis
Hashimoto thyroiditis is an autoimmune phenomenon characterized by lymphocytic infiltration of the gland presumed to be due to similarities between thyroid protein and the viral structure resulting in cross-reacting antibodies. Anti-TPO antibodies that are present in 90% of patients with Hashimoto thyroiditis fix complement and are hence capable of inducing antibody-dependent cell-mediated cytotoxicity, causing the death of thyrocytes.[14]
Postpartum thyroiditis is a destructive thyroiditis characterized by lymphocytic infiltration of the thyroid gland. Fetal cells that migrate to the maternal thyroid gland tend to survive the immunocompromised pregnancy state, and when the maternal immune system rebounds postpartum, it activates the autoimmune phenomenon and causes postpartum thyroiditis.[15][16]
Drug-induced thyroiditis causing hyperthyroidism is usually caused by either an increase in the release and synthesis of thyroid hormone or by destructive thyroiditis caused by the release of preformed hormones. Whereas hypothyroidism is caused by a decrease in the synthesis and release of thyroid hormone or from hypophysitis causing secondary hypothyroidism. The iodine content of the drugs also causes thyroid dysfunction.
Reidel’s thyroiditis: Pathophysiology is not completely understood, but chronic inflammation by the mononuclear cells seems to play a role. It has also been claimed as IgG4 thyroid disease, which includes Reidel thyroiditis, autoimmune pancreatitis, interstitial pneumonia, and orbital pseudotumors.[12]
History and Physical
Acute and Subacute Thyroiditis
Symptoms of upper respiratory tract infection could indicate subacute thyroiditis, and other infective symptoms like fever and neck pain could indicate acute infectious thyroiditis. History of recent radiation to the neck or radioactive iodine treatment could indicate radiation-induced thyroiditis.[17]
On physical exam, most acute thyroiditis patients have a tender and inflamed thyroid gland.
Chronic Thyroiditis
For chronic thyroiditis, a detailed history is paramount to narrowing the etiology. Medication history is important to diagnose underlying drug-induced thyroiditis. Personal history and family history of autoimmune disease can help discover any increased risk of autoimmune thyroid disease. Symptoms related to local compressive symptoms in the neck, including difficulty swallowing or choking sensation or hoarseness of the voice, could indicate underlying large goiter or large thyroid nodule or Riedel thyroiditis. Patients with Riedel thyroiditis usually present with dysphagia, odynophagia, respiratory distress due to the compression of the trachea, esophagus, and also because of the extension of the fibrosis.[18]
Physical exam should include a detailed thyroid exam to evaluate any enlargement, tenderness on palpation, any abnormality in the texture, or any palpable nodules.
Drug-induced thyroiditis can be clinically benign on the exam. Symptoms of hypothyroidism like weight gain, fatigue, constipation, dry skin in patients on amiodarone should raise the suspicion of drug-induced thyroiditis. Amiodarone can also cause hyperthyroidism, and clinical manifestations may be masked initially because amiodarone has beta-adrenergic blocking activity. Check-point inhibitor immunotherapy: Patients usually present with vague symptoms of hypothyroidism like fatigue, weight gain. It should be distinguished from secondary hypothyroidism as these drugs also cause hypophysitis.[19]
Autoimmune thyroiditis and Hashimoto thyroiditis usually present with a painless goiter.
Postpartum thyroiditis usually presents with symptoms of thyrotoxicosis like tachycardia, nervousness, and diarrhea with a history of recent childbirth.[20]
Patients with Riedel thyroiditis can have a fixed, hard, painless goiter on physical exam. Most of the patients are euthyroid but can develop hypothyroidism.[18]
Evaluation
Thyroid-stimulating hormone (TSH) should be checked to see if the patient has hyperthyroidism or hypothyroidism. Thyroid microsomal antibodies and thyroid receptor antibodies can be checked for confirmation of autoimmune thyroid disease. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are significantly elevated in infectious thyroiditis (bacterial).[2]
Thyroid ultrasound is the most important and most commonly used imaging modality for evaluation of the thyroid gland. Heterogenous thyroid parenchyma indicates inflammation of the thyroid gland, but it does not differentiate between production versus destruction thyroiditis. Thyroid ultrasound can also detect nodules in the thyroid gland. The characteristics of nodules can help to differentiate between benign or malignant nodules.
A thyroid uptake and scan can be done to differentiate production thyroiditis or destruction thyroiditis in patients who present with thyrotoxicosis characterized by low TSH with or without elevated T4 and T3. Low uptake on thyroid scan would indicate destruction thyroiditis (Hashimoto thyroiditis, infectious thyroiditis), while increased or normal uptake indicates production thyroiditis (Graves disease).[14] A thyroid scan can help to further differentiate production thyroiditis into Graves disease, which will show increased uptake throughout the thyroid gland or toxic adenoma, which will show increased uptake in the nodule (hot nodule) with suppression of rest of the thyroid gland.
Fine-needle aspiration is done to evaluate suspicious thyroid nodules to rule out malignancy. In general, any thyroid nodule, which is less than 10 mm, can be monitored without fine-needle aspiration.
Acute Thyroiditis
Thyroid ultrasound, blood cultures, fine needle aspiration with gram stain should be obtained when the clinical presentation is suspicious of infectious thyroiditis. Thyroid function tests are usually normal, but in rare cases, hypo or hyperthyroidism may be present. In cases of radiation thyroiditis, there is a preceding history of radiation exposure or treatment with radioactive iodine for likely Graves disease, which will guide in the diagnosis.
Subacute Thyroiditis
There is a strong association with HLA-35. ESR and CRP are markedly elevated, and so is leucocyte count. T4, T3, and TSH can vary depending on the hyperthyroid or hypothyroid phase. The iodine uptake is low, distinguishing the thyrotoxic phase from Graves disease.[21]
Chronic Thyroiditis
Diagnostic tests for autoimmune/Hashimoto thyroiditis include thyroid peroxidase antibody, which is present in 90% of the patients and thyroglobulin antibody, which is present in 20% to 50%. Thyroid function tests show a hypothyroid picture with high TSH and low T3 and T4. It is associated with HLA-DR3, HLA-DR4, HLA-DR5 in Whites.[14][21]
In patients who are on drugs like amiodarone, lithium, interferon, interleukin 2, and checkpoint inhibitors should have baseline TSH at the commencement of treatment.[19][22] TSH, free T4, free T3 should be obtained in case of the development of symptoms of thyroid dysfunction. Thyroid ultrasound with an iodine uptake scan can be obtained to distinguish drug-induced destructive inflammatory thyroiditis from Graves disease. Uptake is low in drug-induced inflammatory thyroiditis and high in Graves disease.
Postpartum thyroiditis presents with symptoms of hyperthyroidism and history of recent pregnancy and should be evaluated with TSH, free T4, free T3. It can be distinguished from Graves disease by 24-hour iodine uptake scan, and the uptake is low in postpartum thyroiditis.[20]
Riedel thyroiditis: Biopsy is necessary for definitive diagnosis. FNA may not be sufficient for diagnosis and may require an open biopsy for definitive diagnosis of this disease.[23][18]
Treatment / Management
Acute Thyroiditis
Infectious thyroiditis: Patients with suppurative thyroiditis can be managed with nonsurgical management. Antibiotics are used to control infection. NSAIDs are used to control severe neck pain and inflammation. Surgical intervention, like abscess drainage, can be done if clinically indicated.[2](B3)
Radiation-induced thyroiditis: Treatment is symptomatic with NSAIDs or prednisone in severe cases. These patients are increased risk of hypothyroidism and should be followed with a thyroid function test.[24](A1)
Subacute Thyroiditis
It is usually self-limiting, and symptomatic management is all that is needed. NSAIDs are preferred for pain control. In case of severe pain and severe symptoms of thyrotoxicosis, corticosteroids, and beta-blockers can be used for the treatment of inflammation and tachycardia due to thyrotoxicosis. The hypothyroid phase is usually mild and does not require treatment.[25]
Chronic Thyroiditis
Autoimmune thyroiditis: Hashimoto thyroiditis with normal thyroid function can be monitored without treatment with levothyroxine.[14] Hyperthyroidism or Graves disease can be treated with methimazole or propylthiouracil. Methimazole is the drug of choice, but propylthiouracil is preferred during the first trimester of pregnancy and for treatment of the thyroid storm. Permanent treatment of Graves disease included radioactive iodine treatment and thyroidectomy.[26](B3)
Postpartum thyroiditis: It is usually transient, and 80% of patients eventually become euthyroid. Hypothyroid patients can be treated with levothyroxine and monitored with regular thyroid function.[20]
Amiodarone induced thyroiditis: It can cause both hypothyroidism and hyperthyroidism.[27]
Hypothyroidism- Once diagnosed, amiodarone is usually continued along with levothyroxine replacement. If amiodarone is stopped for a different reason, individuals without previous thyroid dysfunction usually progress to euthyroid state with the withdrawal of amiodarone.[27]
Hyperthyroidism - Treatment of type I hyperthyroidism is done with beta-blockers and methimazole. For type 2 thyroiditis, the use of glucocorticoids is recommended to alleviate the hyperthyroid symptoms.
Lithium: Treatment is to continue lithium and start treatment with levothyroxine. It can also cause hyperthyroidism and Graves disease secondary to goiter formation.[11](B2)
Differential Diagnosis
Differential diagnosis of symptomatic thyroiditis includes acute hemorrhage into thyroid cyst, thyroid nodule, thyroid cancer, tonsillitis, and acute pharyngitis.
Prognosis
Thyroiditis with or without thyroid dysfunction has a good prognosis, but long-standing hypothyroidism can predispose to myxedema come, which is more common in the elderly population and has a high mortality rate. Many patients with hypothyroid may have ongoing symptoms even with treatment, which may affect the quality of life.
Complications
Myxedema coma: It is a medical emergency and is characterized by severe hypothyroidism with clinical features of hypothermia, hyponatremia, bradycardia. It is mostly seen in older patients. Treatment should be initiated on clinical suspicion without awaiting lab results. Steroids are given first followed by thyroxine replacement to prevent an adrenal crisis in the scenario of underlying adrenal insufficiency.[28][29]
Thyroid storm is a life-threatening endocrine emergency often triggered by a metabolically stressful event in a patient with long-standing hyperthyroidism like Graves disease. It can present with hyperpyrexia, tachycardia, agitation, and psychosis with laboratory evidence of low TSH, high free T4, and T3. Prompt recognition and treatment of the condition are necessary as this condition is associated with high mortality. The Burch-Wartofsky diagnostic criteria can help with the timely detection of thyroid storm.[30] The standard of care is immediate initiation of beta-blockers, thionamides, and glucocorticoids. Additionally, iodine and cholestyramine can also be used.[31]
Infectious thyroiditis can lead to an abscess and septicemia if not treated promptly.[2]
Patients with Hashimoto thyroiditis are at risk of developing thyroid lymphoma and carcinoma; thus, a rapidly progressing thyroid nodule enlargement or development of new nodules should raise the suspicion.
Deterrence and Patient Education
Thyroiditis is a condition that occurs when the thyroid gland gets inflamed. The thyroid gland is responsible for making a hormone called thyroxine, which controls the human body's metabolism and energy utilization. When the gland is inflamed, due to any cause, it could make insufficient or excessive hormone, which causes symptoms like fatigue, weight gain, depression or palpitations, weight loss, and anxiety, to name a few.
Consult with your doctor to discuss the right treatment as the management varies depending on the type of thyroiditis, and the physician needs to investigate and follow up with laboratory tests to ensure continued management of the thyroiditis.
Enhancing Healthcare Team Outcomes
Thyroiditis comprises of a group of diseases that can present with strikingly similar symptoms. This frequently poses a diagnostic dilemma to uncover the exact etiology. These patients may present with hyper or hypothyroid symptoms with subtle differences depending on the etiology. A thorough history and physical examination is the key to uncover these subtle differences. It is also important to consult with an endocrinologist to investigate the exact etiology of thyroiditis as well as to help institute the correct treatment and reduce patient morbidity.
The current guidelines for management have been developed with expert recommendations and literature from peer-reviewed journals to determine the appropriateness of laboratory testing and imaging, as well as the formulation of and treatment strategies.
Media
References
Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, Braverman LE. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). The Journal of clinical endocrinology and metabolism. 2002 Feb:87(2):489-99 [PubMed PMID: 11836274]
Level 3 (low-level) evidencePaes JE, Burman KD, Cohen J, Franklyn J, McHenry CR, Shoham S, Kloos RT. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid : official journal of the American Thyroid Association. 2010 Mar:20(3):247-55. doi: 10.1089/thy.2008.0146. Epub [PubMed PMID: 20144025]
Level 3 (low-level) evidenceVolpé R, Row VV, Ezrin C. Circulating viral and thyroid antibodies in subacute thyroiditis. The Journal of clinical endocrinology and metabolism. 1967 Sep:27(9):1275-84 [PubMed PMID: 4292248]
Ohsako N, Tamai H, Sudo T, Mukuta T, Tanaka H, Kuma K, Kimura A, Sasazuki T. Clinical characteristics of subacute thyroiditis classified according to human leukocyte antigen typing. The Journal of clinical endocrinology and metabolism. 1995 Dec:80(12):3653-6 [PubMed PMID: 8530615]
Tandon N, Zhang L, Weetman AP. HLA associations with Hashimoto's thyroiditis. Clinical endocrinology. 1991 May:34(5):383-6 [PubMed PMID: 1676351]
Jenkins D, Penny MA, Fletcher JA, Jacobs KH, Mijovic CH, Franklyn JA, Sheppard MC. HLA class II gene polymorphism contributes little to Hashimoto's thyroiditis. Clinical endocrinology. 1992 Aug:37(2):141-5 [PubMed PMID: 1356664]
Level 1 (high-level) evidenceVargas MT,Briones-Urbina R,Gladman D,Papsin FR,Walfish PG, Antithyroid microsomal autoantibodies and HLA-DR5 are associated with postpartum thyroid dysfunction: evidence supporting an autoimmune pathogenesis. The Journal of clinical endocrinology and metabolism. 1988 Aug [PubMed PMID: 3260599]
Pearce EN, Farwell AP, Braverman LE. Thyroiditis. The New England journal of medicine. 2003 Jun 26:348(26):2646-55 [PubMed PMID: 12826640]
Imaizumi M, Pritsker A, Unger P, Davies TF. Intrathyroidal fetal microchimerism in pregnancy and postpartum. Endocrinology. 2002 Jan:143(1):247-53 [PubMed PMID: 11751616]
Level 3 (low-level) evidenceGaron-Czmil J, Petitpain N, Rouby F, Sassier M, Babai S, Yelehe-Okouma M, Weryha G, Klein M, Gillet P. Thyroiditis and immune check point inhibitors: the post-marketing experience using the French National Pharmacovigilance database. Fundamental & clinical pharmacology. 2019 Apr:33(2):241-249. doi: 10.1111/fcp.12423. Epub 2018 Nov 14 [PubMed PMID: 30308083]
Miller KK,Daniels GH, Association between lithium use and thyrotoxicosis caused by silent thyroiditis. Clinical endocrinology. 2001 Oct [PubMed PMID: 11678833]
Level 2 (mid-level) evidenceUmehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, Matsui S, Yoshino T, Nakamura S, Kawa S, Hamano H, Kamisawa T, Shimosegawa T, Shimatsu A, Nakamura S, Ito T, Notohara K, Sumida T, Tanaka Y, Mimori T, Chiba T, Mishima M, Hibi T, Tsubouchi H, Inui K, Ohara H. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Modern rheumatology. 2012 Feb:22(1):21-30. doi: 10.1007/s10165-011-0571-z. Epub 2012 Jan 5 [PubMed PMID: 22218969]
Burikhanov RB, Matsuzaki S. Excess iodine induces apoptosis in the thyroid of goitrogen-pretreated rats in vivo. Thyroid : official journal of the American Thyroid Association. 2000 Feb:10(2):123-9 [PubMed PMID: 10718548]
Level 3 (low-level) evidencePeng CC, Huai-En Chang R, Pennant M, Huang HK, Munir KM. A Literature Review of Painful Hashimoto Thyroiditis: 70 Published Cases in the Past 70 Years. Journal of the Endocrine Society. 2020 Feb 1:4(2):bvz008. doi: 10.1210/jendso/bvz008. Epub 2019 Nov 16 [PubMed PMID: 32047869]
Level 3 (low-level) evidenceKeely EJ. Postpartum thyroiditis: an autoimmune thyroid disorder which predicts future thyroid health. Obstetric medicine. 2011 Mar:4(1):7-11. doi: 10.1258/om.2010.100041. Epub 2011 Mar 1 [PubMed PMID: 27579088]
De Groot L, Abalovich M, Alexander EK, Amino N, Barbour L, Cobin RH, Eastman CJ, Lazarus JH, Luton D, Mandel SJ, Mestman J, Rovet J, Sullivan S. Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society clinical practice guideline. The Journal of clinical endocrinology and metabolism. 2012 Aug:97(8):2543-65. doi: 10.1210/jc.2011-2803. Epub [PubMed PMID: 22869843]
Level 1 (high-level) evidenceGiuffrida G, Bagnato G, Campennì A, Giovinazzo S, Keller KP, Alibrandi A, Roberts WN, Trimarchi F, Ruggeri RM. Non-specific rheumatic manifestations in patients with Hashimoto's thyroiditis: a pilot cross-sectional study. Journal of endocrinological investigation. 2020 Jan:43(1):87-94. doi: 10.1007/s40618-019-01083-w. Epub 2019 Jul 12 [PubMed PMID: 31301020]
Level 2 (mid-level) evidenceFatourechi MM, Hay ID, McIver B, Sebo TJ, Fatourechi V. Invasive fibrous thyroiditis (Riedel thyroiditis): the Mayo Clinic experience, 1976-2008. Thyroid : official journal of the American Thyroid Association. 2011 Jul:21(7):765-72. doi: 10.1089/thy.2010.0453. Epub 2011 May 13 [PubMed PMID: 21568724]
Muller I, Moran C, Lecumberri B, Decallonne B, Robertson N, Jones J, Dayan CM. 2019 European Thyroid Association Guidelines on the Management of Thyroid Dysfunction following Immune Reconstitution Therapy. European thyroid journal. 2019 Jul:8(4):173-185. doi: 10.1159/000500881. Epub 2019 Jul 4 [PubMed PMID: 31602359]
Ide A, Amino N, Kang S, Yoshioka W, Kudo T, Nishihara E, Ito M, Nakamura H, Miyauchi A. Differentiation of postpartum Graves' thyrotoxicosis from postpartum destructive thyrotoxicosis using antithyrotropin receptor antibodies and thyroid blood flow. Thyroid : official journal of the American Thyroid Association. 2014 Jun:24(6):1027-31. doi: 10.1089/thy.2013.0585. Epub 2014 Mar 6 [PubMed PMID: 24400892]
Ruchala M, Szczepanek E, Sowinski J. Sonoelastography in de Quervain thyroiditis. The Journal of clinical endocrinology and metabolism. 2011 Feb:96(2):289-90. doi: 10.1210/jc.2010-1595. Epub [PubMed PMID: 21296992]
Level 3 (low-level) evidenceIyer PC, Cabanillas ME, Waguespack SG, Hu MI, Thosani S, Lavis VR, Busaidy NL, Subudhi SK, Diab A, Dadu R. Immune-Related Thyroiditis with Immune Checkpoint Inhibitors. Thyroid : official journal of the American Thyroid Association. 2018 Oct:28(10):1243-1251. doi: 10.1089/thy.2018.0116. Epub [PubMed PMID: 30132401]
Harigopal M, Sahoo S, Recant WM, DeMay RM. Fine-needle aspiration of Riedel's disease: report of a case and review of the literature. Diagnostic cytopathology. 2004 Mar:30(3):193-7 [PubMed PMID: 14986301]
Level 3 (low-level) evidenceMa C, Xie J, Wang H, Li J, Chen S. Radioiodine therapy versus antithyroid medications for Graves' disease. The Cochrane database of systematic reviews. 2016 Feb 18:2():CD010094. doi: 10.1002/14651858.CD010094.pub2. Epub 2016 Feb 18 [PubMed PMID: 26891370]
Level 1 (high-level) evidenceSamuels MH. Subacute, silent, and postpartum thyroiditis. The Medical clinics of North America. 2012 Mar:96(2):223-33. doi: 10.1016/j.mcna.2012.01.003. Epub 2012 Feb 4 [PubMed PMID: 22443972]
Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, Rivkees SA, Samuels M, Sosa JA, Stan MN, Walter MA. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid : official journal of the American Thyroid Association. 2016 Oct:26(10):1343-1421 [PubMed PMID: 27521067]
Benjamens S, Dullaart RPF, Sluiter WJ, Rienstra M, van Gelder IC, Links TP. The clinical value of regular thyroid function tests during amiodarone treatment. European journal of endocrinology. 2017 Jul:177(1):9-14. doi: 10.1530/EJE-17-0018. Epub 2017 Apr 19 [PubMed PMID: 28424174]
Ono Y, Ono S, Yasunaga H, Matsui H, Fushimi K, Tanaka Y. Clinical characteristics and outcomes of myxedema coma: Analysis of a national inpatient database in Japan. Journal of epidemiology. 2017 Mar:27(3):117-122. doi: 10.1016/j.je.2016.04.002. Epub 2017 Jan 5 [PubMed PMID: 28142035]
Popoveniuc G, Chandra T, Sud A, Sharma M, Blackman MR, Burman KD, Mete M, Desale S, Wartofsky L. A diagnostic scoring system for myxedema coma. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2014 Aug:20(8):808-17. doi: 10.4158/EP13460.OR. Epub [PubMed PMID: 24518183]
Idrose AM. Acute and emergency care for thyrotoxicosis and thyroid storm. Acute medicine & surgery. 2015 Jul:2(3):147-157. doi: 10.1002/ams2.104. Epub 2015 May 12 [PubMed PMID: 29123713]
Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, Tsuboi K, Monden T, Kouki T, Otani H, Teramukai S, Uehara R, Nakamura Y, Nagai M, Mori M, Japan Thyroid Association. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid : official journal of the American Thyroid Association. 2012 Jul:22(7):661-79. doi: 10.1089/thy.2011.0334. Epub 2012 Jun 12 [PubMed PMID: 22690898]
Level 2 (mid-level) evidence