Anatomy, Bony Pelvis and Lower Limb: Tibialis Posterior Muscle
Anatomy, Bony Pelvis and Lower Limb: Tibialis Posterior Muscle
Introduction
The tibialis posterior muscle (TPM) is the deepest muscle of the deep posterior compartment of the lower leg. Its long muscle belly arises from the posterior aspect of the interosseous membrane and superior two-thirds of the posterior and medial surface of the fibula, and the superior aspect of the proximal tibia. The TPM tendon inserts distally onto many attachment points on the plantar surface of the foot. The muscle is primarily responsible for plantar flexion and inversion of the foot and receives its arterial blood supply and innervation from the posterior tibial artery and tibial nerve, respectively.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Structure
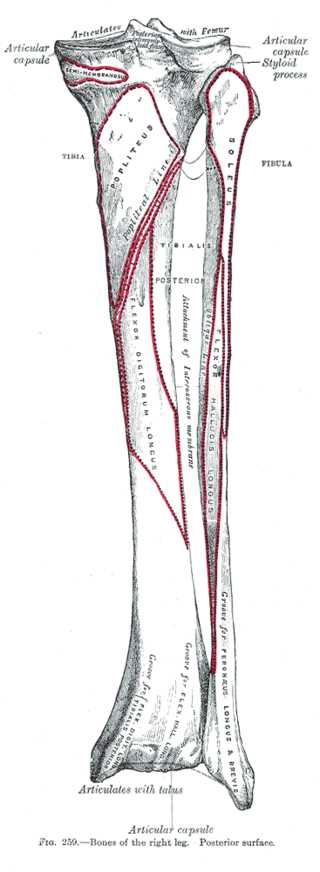
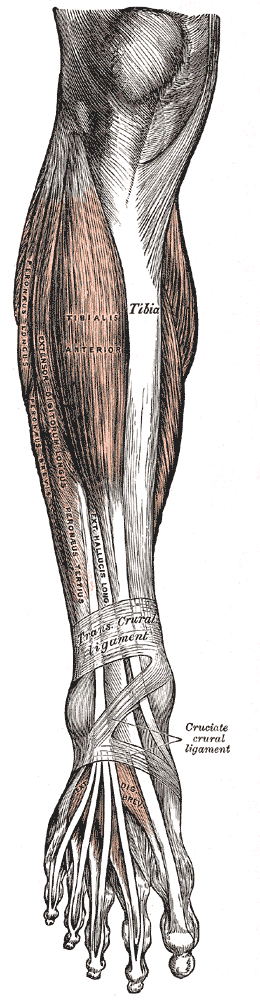
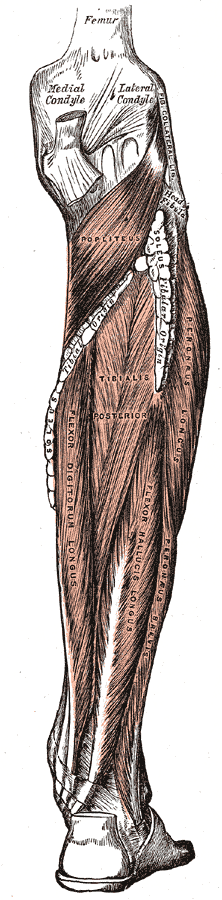
The posterior compartment of the lower leg consists of superficial and deep divisions. The three muscles within the superficial posterior compartment include the gastrocnemius, soleus, and plantaris muscles. The deep posterior compartment muscles include the flexor hallucis longus (FHL), flexor digitorum longus (FDL), TPM, and popliteus muscles.[1][2][3]
The TPM's muscle belly originates from many proximal attachments; these attachments include the posterior surface of the upper half of the posterior tibia, the middle of the posterior fibula, and the posterior interosseous membrane. These deep attachments lie in the center between the FDL and the FHL. The tibialis posterior tendon (TPT) travels distally, then posterior to the medial malleolus along with the FDL tendons, posterior tibial artery, tibial nerve, and FHL.
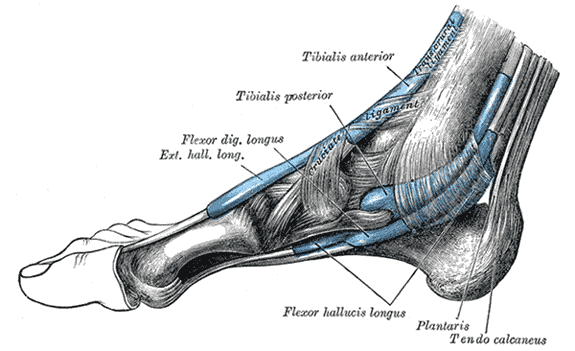
Once the TPT travels distal to the medial malleolus, it courses along the plantar aspect of the foot, where it splits into three components: primary, plantar, and recurrent. This split allows for the broad attachment site of the tibialis posterior tendon (TPT). The main portion inserts primarily onto the navicular bone tubercle as well as the plantar sections of the medial cuneiform. The plantar portion inserts onto the base of the second, third, and fourth metatarsals along with the second and third cuneiform and the cuboid. Finally, the recurrent portion has a small insertion site at the sustentaculum tali of the calcaneus.
The flexor retinaculum (FR), also known as the laciniate ligament and the tarsal tunnel, is a strong fibrous band that covers the medial ankle from the medial malleolus to the calcaneus. The flexor retinaculum forms the canal allowing the passage of the tendons from the posterior compartment of the lower leg. The TPT passes beneath the flexor retinaculum, covered by a synovial lined tunnel acting as a tendon sheath to reduce friction.[4]
Function
The tibialis posterior (TP), along with the tibialis anterior, is a primary inverter of the foot. This inversion happens at two synovial joints of the foot: the midtarsal joint, between the talus and navicular bone, and the subtalar joint, between the talus and calcaneus.
Because the tibialis posterior (TP) originates from the posterior compartment of the lower leg, the tibialis posterior is also a secondary plantar flexor of the foot along with the gastrocnemius, soleus, and plantaris muscles.
The plantar insertions of the tibialis posterior allow for support of the medial arch of the foot. The medial arch in a normal person is higher than the lateral arch and is maintained by the following bones: calcaneus, talus, navicular, three cuneiforms, and the first three metatarsals.[5]
Embryology
The tibialis posterior muscle, a muscle of the posterior compartment of the lower limb, is formed beginning at four weeks of gestation as a primary limb bud. Limb buds begin as undifferentiated mesenchyme (mesoderm) with an epithelial (ectoderm) covering; they are paddle-shaped structures that grow outwards gradually under the influence of local growth factors. By eight weeks of gestation, the skeletal muscle that derives from somites at the level of the limb buds is well-formed.[6]
Blood Supply and Lymphatics
The vascular supply to the tibialis posterior is predominantly via the posterior tibial artery, which arises from the popliteal artery. The popliteal artery courses posterior to the knee and primarily splits into the anterior tibial and posterior tibial arteries.[7] The anterior tibial artery passes through the tibialis posterior muscle and over the interosseous membrane, where it enters the anterior compartment.
The posterior tibial artery courses in the deep posterior compartment of the lower leg, deep to the soleus, and superficial to the deep muscles, including the tibialis posterior. The posterior tibial artery, which gives off the fibular (peroneal) artery, continues inferiorly through the posterior compartment of the lower leg. It supplies muscular branches to all of the muscles in the posterior compartment, including the posterior tibialis muscle. The posterior tibial artery then continues to the foot behind the medial malleolus along with the tibialis posterior tendon, flexor digitorum longus tendons, tibial nerve, and flexor hallucis longus.
The posterior tibial artery gives off the fibular (peroneal) artery, which courses deep to the flexor hallucis longus and gives off muscular branches to supply some of the posterior compartment before entering its primary destination, the lateral compartment of the lower leg.[8][9][10]
Nerves
The tibial nerve innervates the tibialis posterior muscle. The tibial nerve is a component of the sciatic nerve, which comes from the ventral rami of spinal roots L4-S3. The sciatic nerve splits into the tibial nerve, which continues inferiorly, and the common peroneal nerve, which travels laterally around the neck of the fibula.
The tibial nerve courses inferiorly with the posterior tibial artery deep to the soleus muscle in the posterior compartment on the posterior surface of the tibialis posterior muscle belly. The tibial nerve gives off motor branches to all of the muscles of the posterior compartment, including the tibialis posterior. The tibial nerve continues inferiorly and passes posterior to the medial malleolus with the tibialis posterior tendon, flexor digitorum longus tendons, posterior tibial artery, and flexor hallucis longus within the tarsal tunnel. The tibial nerve exits the tarsal tunnel onto the plantar surface of the foot, where it divides into both the medial and lateral plantar nerves.[11][12]
Muscles
The tibialis posterior is in the posterior compartment of the lower leg. The posterior compartment contains seven muscles: the gastrocnemius, soleus, plantaris, popliteus, flexor digitorum longus, flexor hallucis longus, and the tibialis posterior. The muscles contained in the posterior compartment receive innervation by the tibial nerve and are primarily supplied by the posterior tibial artery. The gastrocnemius and the soleus are referred to as the triceps surae and are the primary plantar flexors. The plantaris is a secondary plantar flexor of the foot, while the flexor digitorum longus and the flexor hallucis longus are primary flexors of the lateral four toes and the great toe, respectively, with some plantar flexion.
The tibialis posterior acts to plantarflex the foot and invert the foot and support the medial arch.
The muscles of the anterior compartment primarily antagonize the posterior compartment muscles. Collectively, the anterior muscles dorsiflex the foot at the ankle joint. The lateral compartment muscles assist in the eversion of the foot and plantar flexion.
Physiologic Variants
The tibialis posterior tendon (TPT) can have variable insertion patterns. It can have three separate tendons known as the main, plantar, and recurrent tendons, or it can have one wide tendon that inserts onto the same bones on the plantar surface of the foot.
Surgical Considerations
Rupture of the tibialis posterior tendon (TPT) would require surgical assistance. With a rupture of the tibialis posterior, there would be a decrease in the ability to plantarflex and invert the foot. The muscles of the posterior compartment would be able to plantarflex the foot, and some inversion of the foot would be possible due to the actions of the tibialis anterior, but the loss of the tibialis posterior tendon would lead to an everted flat foot due to the inability to maintain the medial arch. This loss would also lead to a valgus deformity, and a gait disorder, where the treatment required is surgical reattachment and repair of the tibialis posterior tendon.
Clinical Significance
Posterior Tibial Tendon Insufficiency (PTTI)
The tibialis posterior tendon (TPT) can become inflamed and irritated due to an acute injury, such as a fall, or overuse during high-impact sports such as basketball, tennis, or soccer. Acute on chronic bouts of recurrent tendinitis propagate the tendinopathic cascade, potentially leading to posterior tibial tendon insufficiency (PTTI).
The pathophysiology underlying PTTI entails the progressive loss of the medial longitudinal arch, compromising its ability for dynamic stabilization of the foot. Later stages of PTTI and arch collapse eventually lead to attritional failure of static hindfoot stabilizers, including compromise to the spring ligament complex (superomedial calcaneonavicular ligament), the plantar fascia, and plantar ligamentous support structures.[13] PTTI is the most common cause of adult-acquired flatfoot deformity (AFFD).
Patients often present secondary to pain and progressive dysfunction. Observation of the foot highlights a spectrum from flexible (early) to rigid (end-stage, degenerative) deformities. The patient should be observed clinically during normal gait posturing as well as statically and dynamically. The patient is asked to stand during the examination, and when viewed from the back, the examiner may be able to appreciate the "too many toes sign," referring to the lateral deviation of the toes relative to the hindfoot. The spectrum of PTTI foot deformity and characteristic posturing categorizes into the following descriptions:
- Pes planus
- Hindfoot valgus
- Forefoot varus
- Forefoot abduction
Compartment Syndrome
Acute Compartment Syndrome (ACS)
Acute compartment syndrome (ACS) occurs secondary to traumatic (e.g., fractures), iatrogenic (e.g., external sources of cast/dressing compression), or comorbid medical conditions (e.g., bleeding disorders). Regardless of the underlying etiology, ACS develops when the osseous-fascial compartment pressure increases to a level that results in decreased perfusion of the muscle(s) within the specific compartment, potentially leading to irreversible muscle and nerve damage.[14] ACS can occur in any region where fascia surrounds the skeletal muscle.[15] Patients presenting with ACS most commonly demonstrate pain out of proportion on the exam. Exceptions to this common presentation include:
- Polytrauma patients
- Intubated/sedated patients
- Pediatric patients
These exceptions require heightened clinical suspicion, and immediate clinical attention is warranted to delineate a diagnosis to expedite the decision to proceed with surgical intervention. Classic examination findings include:
- Pain with passive stretch
- The most sensitive finding before the onset of ischemia.
- Paresthesia
- Motor weakness
- It can be subtle and difficult to appreciate, especially in the setting of trauma.
- Palpable swelling
- Diminished to absent peripheral pulses
- Absent pulses are often a late finding and often result in inevitable amputation.
Lower leg ACS, specifically isolated to the posterior compartment, will lead to the aforementioned clinical findings, including motor weakness/inability to plantarflex the foot and weakness of toe flexion and foot inversion. There will be a sensory loss over the lateral part of the leg and foot due to compression of the sural nerve, as well as sensory loss along the plantar surface of the foot and toes due to tibial nerve ischemia.
Diagnosis of compartment syndrome before severe ischemia and necrosis occur is necessary for preventing poor outcomes. The clinical diagnosis in a patient with an intact mental status is often by physical examination alone. Treatment is emergent fasciotomies of the involved compartments.[16]
Chronic Exertional Compartment Syndrome (CECS)
CECS is clinically differentiated from ACS and is a diagnostic consideration in athletes presenting with lower leg pain often attributable to endurance exercises, including sport-specific activities and training programs. CECS is thought to occur secondary to increased intramuscular pressures within a specific compartment(s) attributable to exercise and activity. Unlike ACS, however, CECS occurs across a spectrum of transient ischemia with or without progressive neurovascular dysfunction.[17] CECS in the lower leg most commonly affects the anterior and lateral compartments, followed by the posterior compartments (superficial in approximately 1 to 3%, and deep posterior in 3 to 10%).[18]
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome results from tibial nerve compression within the tarsal tunnel. The tibial nerve travels inferiorly through the posterior compartment of the lower leg on the posterior surface of the tibialis posterior. It follows the tibialis posterior tendon posterior to the medial malleolus through the tarsal tunnel. This compartment is narrow, and increased compression will affect the tendons and the tibial nerve. Compression of the nerve could come from fibrosis, ganglion cysts, osteochondromas, trauma, ankle sprains, obesity, tight shoes, or other causes.
The symptoms are similar to the symptoms of carpal tunnel in the wrist with the median nerve. Symptoms include burning, numbness, tingling, and weakness of the plantar muscle of the foot and toes. The pain worsens with prolonged use, such as standing, activity, and motion through the carpal tunnel. Tinel's sign can be elicited with percussion on the tibial nerve, and a positive sign is pain, numbness, or tingling along the nerve distribution.
Treatment can include noninvasive modifications such as weight loss, changing daily habits, changing shoes to orthotics, NSAIDs, and osteopathic manipulative medicine. Surgery is possible management for decompression of the tibial nerve, which involves manipulating the flexor retinaculum covering the tarsal tunnel.[19]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Mostafa E, Graefe SB, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Leg Posterior Compartment. StatPearls. 2023 Jan:(): [PubMed PMID: 30726025]
Binstead JT, Munjal A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Calf. StatPearls. 2023 Jan:(): [PubMed PMID: 29083629]
Cantrell AJ, Imonugo O, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Leg Bones. StatPearls. 2023 Jan:(): [PubMed PMID: 30725709]
Juneja P, Hubbard JB. Anatomy, Bony Pelvis and Lower Limb: Tibialis Anterior Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 30020676]
Bourne M, Sinkler MA, Murphy PB. Anatomy, Bony Pelvis and Lower Limb: Tibia. StatPearls. 2023 Jan:(): [PubMed PMID: 30252309]
Galli A, Robay D, Osterwalder M, Bao X, Bénazet JD, Tariq M, Paro R, Mackem S, Zeller R. Distinct roles of Hand2 in initiating polarity and posterior Shh expression during the onset of mouse limb bud development. PLoS genetics. 2010 Apr 8:6(4):e1000901. doi: 10.1371/journal.pgen.1000901. Epub 2010 Apr 8 [PubMed PMID: 20386744]
Level 3 (low-level) evidenceHyland S, Sinkler MA, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Popliteal Region. StatPearls. 2023 Jan:(): [PubMed PMID: 30422486]
Azam M, Wehrle CJ, Shaw PM. Anatomy, Bony Pelvis and Lower Limb: Tibial Artery. StatPearls. 2023 Jan:(): [PubMed PMID: 30422466]
Day CP, Orme R. Popliteal artery branching patterns -- an angiographic study. Clinical radiology. 2006 Aug:61(8):696-9 [PubMed PMID: 16843754]
Level 2 (mid-level) evidenceKhan IA, Mahabadi N, D’Abarno A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Leg Lateral Compartment. StatPearls. 2023 Jan:(): [PubMed PMID: 30137811]
Hardin JM, Devendra S. Anatomy, Bony Pelvis and Lower Limb: Calf Common Peroneal Nerve (Common Fibular Nerve). StatPearls. 2023 Jan:(): [PubMed PMID: 30422563]
Desai SS, Cohen-Levy WB. Anatomy, Bony Pelvis and Lower Limb: Tibial Nerve. StatPearls. 2023 Jan:(): [PubMed PMID: 30725713]
Bourne M, Talkad A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb, Foot Fascia. StatPearls. 2023 Jan:(): [PubMed PMID: 30252299]
Varacallo M, Shirey L, Kavuri V, Harding S. Acute compartment syndrome of the hand secondary to propofol extravasation. Journal of clinical anesthesia. 2018 Jun:47():1-2. doi: 10.1016/j.jclinane.2018.01.020. Epub 2018 Feb 21 [PubMed PMID: 29476968]
Dave HD, Shook M, Varacallo M. Anatomy, Skeletal Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30725921]
Stella M, Santolini E, Sanguineti F, Felli L, Vicenti G, Bizzoca D, Santolini F. Aetiology of trauma-related acute compartment syndrome of the leg: A systematic review. Injury. 2019 Jul:50 Suppl 2():S57-S64. doi: 10.1016/j.injury.2019.01.047. Epub 2019 Feb 2 [PubMed PMID: 30772051]
Level 1 (high-level) evidenceRaikin SM, Rapuri VR, Vitanzo P. Bilateral simultaneous fasciotomy for chronic exertional compartment syndrome. Foot & ankle international. 2005 Dec:26(12):1007-11 [PubMed PMID: 16390630]
Level 2 (mid-level) evidenceCampano D, Robaina JA, Kusnezov N, Dunn JC, Waterman BR. Surgical Management for Chronic Exertional Compartment Syndrome of the Leg: A Systematic Review of the Literature. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2016 Jul:32(7):1478-86. doi: 10.1016/j.arthro.2016.01.069. Epub 2016 Mar 24 [PubMed PMID: 27020462]
Level 1 (high-level) evidenceBowley MP, Doughty CT. Entrapment Neuropathies of the Lower Extremity. The Medical clinics of North America. 2019 Mar:103(2):371-382. doi: 10.1016/j.mcna.2018.10.013. Epub 2018 Dec 3 [PubMed PMID: 30704688]