Introduction
Tooth eruption is when a developing tooth moves from its initial nonfunctional position within the alveolar bone to its final functional location within the oral cavity.[1] Notably, the term eruption should not be mistaken for emergence, as the latter refers explicitly to the point at which any portion of the tooth's crown becomes visible through the gingiva.[2]
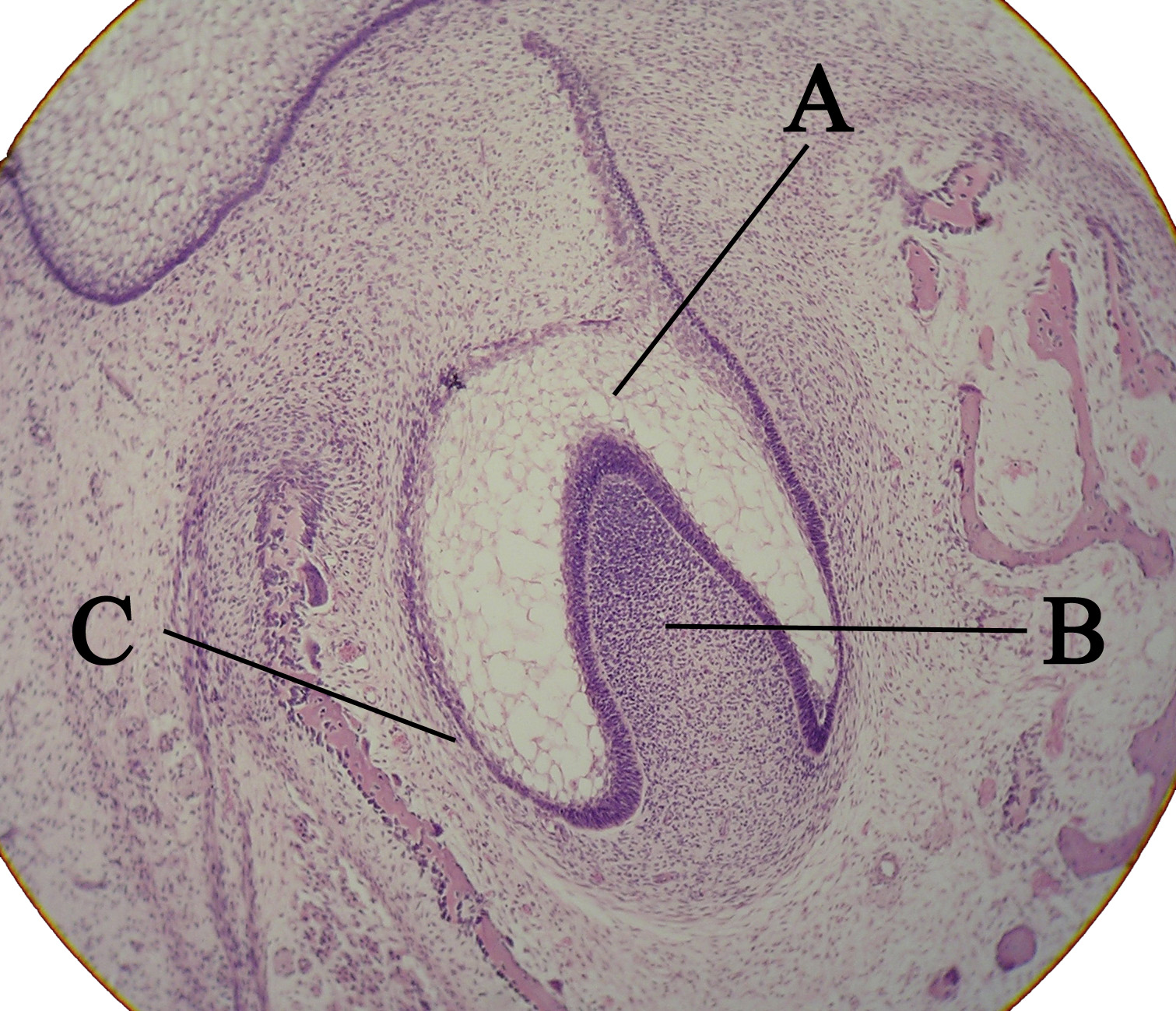
Tooth eruption results from bone remodeling processes involving bone formation and resorption mechanisms.[1] Experimental research has demonstrated that the dental follicle (see Image. Microscopic View of a Tooth Bud) is pivotal in transforming these changes within the alveolar bone. Moreover, the dental follicle gives rise to the periodontal ligament—a structure believed to have a significant role in facilitating tooth eruption during the supraosseous stage.[1]
The phenomenon of bone resorption offers a distinct pathway for the correct emergence and alignment of a developing tooth. The force propelling the tooth toward the occlusal plane along this path is believed to originate from bone apposition occurring apically to the developing tooth.[3] The onset of eruptive movements typically coincides with the initiation of root formation.[3] Root growth is not the primary cause of tooth eruption, although it may have a role in the process. This is evident as teeth can still erupt without fully formed roots.[3]
The periodontal ligament is believed to mediate supraosseous events during tooth eruption.[1] In contrast, intraosseous events, which involve changes within the bone itself, are not directly influenced or regulated by the actions of the periodontal ligament.[1] These events primarily involve bone remodeling mechanisms and the creation of the eruption pathway.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Two crucial factors aid in the process of tooth eruption. First, the permanent teeth require the removal of bone and primary roots. Second, soft tissue alterations are necessary, followed by the application of force that propels the tooth toward the occlusal surface, directing it along an established eruption pathway.[4] Despite significant progress, the exact mechanisms regulating these events are still not fully comprehended. Nonetheless, valuable insights have been gleaned from studies involving various species and clinical experiences.
Tooth eruption is primarily attributed to bone remodeling mechanisms. Within this process, different areas of the dental follicle are believed to mediate bone resorption occlusal to the developing crown and alveolar bone formation apical to the developing root. This coordinated activity facilitates the tooth's movement toward the alveolar crest.[3] The dental follicle is an organized connective tissue that envelops the tooth germ during the early stages of tooth development.[1] In addition, the dental follicle is the source of the periodontal ligament, believed to have a role in tooth eruption during the supraosseous stage.[1]
Resorptive cellular activity within the dental follicle commences once the crown has fully developed, triggered by signals from the enamel epithelium.[3] Potential mediators of this resorption process include interleukin-1, epidermal growth factor-1, matrix metalloproteinases, and various unidentified proteins found within the enamel organ and the dental follicle.[3]
The process of tooth eruption can be categorized into 2 distinct stages—intraosseous and supraosseous. During the intraosseous stage, the tooth undergoes bone resorption, which enables its movement within the bone structure. The supraosseous stage commences when a portion of the erupting crown becomes visible above the alveolar crest.[1]
The phases of tooth eruption are divided into 5 stages—pre-eruptive movement, intraosseous eruption, mucosal penetration, pre-occlusal eruption, and post-occlusal eruption—which provides a more comprehensive overview of the process.[3]
Clinical and Experimental Findings on Tooth Eruption
Pre-eruptive movement
Crown development occurs within the alveolar bone, and during this phase, small, random movements occur before the eruption. These movements are localized and do not follow a distinct axial eruption direction.[3] However, it remains uncertain whether these developing crown movements are attributed to the natural growth and maturation of the jaws or if events mediated by the dental follicle influence them.[3]
Intraosseous eruption
The initial phases of tooth eruption commence when the crown fully develops and root formation begins.[4] In this phase, an eruption pathway is created through bone resorption that facilitates the tooth's emergence.[4] Studies on dog premolars have revealed that the role of the dental follicle in tooth eruption is pivotal, as it ensures timely eruption and exfoliation of the tooth, irrespective of the crown's influence. Although earlier it was proposed that pressure from the developing tooth triggers osteoclastic activity and forms the eruption pathway,[4] this study disproves that theory.
The study is outlined as follows:
- Alveolar resorption occlusal to the tooth persisted despite immobilizing the tooth bud by ligating the dog's mandible.[5]
- The unerupted tooth's crown was extracted and substituted with a metallic replica, which was subsequently inserted into the dental follicle, resulting in the normal eruption of the tooth.[5]
- The removal of the dental follicle halted the tooth eruption and localized bone metabolism. Specifically, removing its coronal half hindered the formation of an eruption pathway, whereas removing its basal half obstructed bone apposition.[5]
Furthermore, in a clinical case involving a human patient, unintentional ligation of a tooth bud while managing a jaw fracture led to resorptive activity that spontaneously formed an eruption pathway for the immobilized tooth bud.[4]
These observations underscore the importance of the dental follicle in regulating alveolar bone metabolism, as it is crucial for alveolar bone resorption and apposition processes, which are vital for tooth eruption during the intraosseous stage.[5] Root formation occurs concurrently with the eruption process, potentially influencing the eruption speed.[3] However, it is crucial to underscore that tooth eruption cannot be solely attributed to root formation. This is evident in cases such as dysplasia type I, where teeth with incomplete roots can still erupt,[3] and instances where teeth with closed apices also successfully undergo eruption.
Mucosal penetration and eruption
Once the tooth's cusps reach the alveolar crest, the eruption pathway is fully established, leading to an increased eruption rate. However, this accelerated rate gradually diminishes as the tooth approaches the occlusal plane.[3] During this phase, significant changes occur within the enamel epithelium. The enamel epithelium undergoes thickening and transformation processes, eventually merging with the oral epithelium, primarily driven by the proliferation of the external enamel epithelium and proteolytic events.[3]
Proteins derived from the enamel matrix are released before and during the penetration of the oral mucosa. These proteins are hypothesized to contribute to inducing a hypersensitivity reaction, thereby triggering the typical symptoms associated with teething, including fever, rhinitis, and localized erythema.[3] Another significant event during mucosal penetration is the formation of the junctional epithelium on the tooth's surface.[3]
The movement responsible for elevating the tooth from the gingival to the occlusal plane is primarily attributed to the collagen fibers within the periodontal ligament. Collagen maturation, characterized by a cross-linking and shortening process, is pivotal in generating the propulsive force that drives the eruptive mechanism.[4] Oral forces can modify the orientation and quantity of these fibers, triggering the activation of this eruptive mechanism.[4] Medications that disrupt collagen maturation also hinder tooth eruption, strongly indicating that the collagen fibers within the periodontal ligament serve as the primary mechanism for post-emergent axial movement of the tooth.[4][6]
The propulsive force responsible for moving the erupting tooth from its gingival emergence to the occlusal plane is contributed to by root growth and bone apposition at the crypt's base and interradicular septa.[3] Studies have indicated that this eruption stage occurs during a limited timeframe in the early evening, coinciding with the peak levels of growth.[4] Furthermore, fluctuations in the blood flow within the periodontal ligament may influence the eruption rate during this period.[4]
Post-occlusal eruption
Once the tooth has reached its functional position within the occlusal plane, a series of processes are initiated to anchor it in its new location firmly. These mechanisms involve bone-related activities, including the formation of circumferential bone, the visible appearance of the lamina dura in x-rays, and the maturation of the periodontal ligament fibers.[3] Furthermore, during the post-occlusal stage, the roots of the tooth undergo their final growth phase (see Image. Post-Occlusal Eruption).[3]
The mechanism underlying horizontal movements remains a subject of investigation. One hypothesis suggests that horizontal displacements, such as buccal movement, occur through a coordinated process involving bone resorption, formation, and cementum apposition.[3] Cementum apposition may also be partly responsible for the compensatory eruption observed in tooth wear.[3] Teeth can continue to undergo eruption even in adulthood as a compensatory response to the loss of an opposing tooth, demonstrating that eruption activity persists throughout an individual's life.[4]
Tooth Eruption Theories
Various mechanisms have been proposed to explain tooth eruption. Marks and Schroeder introduced criteria for a valid tooth eruption theory, emphasizing 3 fundamental eruption facts:[3]
- Teeth move axially and in 3 dimensions.
- Teeth exhibit distinct eruption characteristics and have varying stage-specific needs.
- The functional position of teeth is inheritable.
A concise overview of historical and contemporary tooth eruption theories is as follows:
Cushioned hammock theory
Harry Sicher's theory attributes tooth eruption to a cushioned hammock ligament beneath the tooth.
Root formation theory
According to the root formation theory, the apically directed force generated by the growing root exerts a reactive occlusal force, leading to the coronal movement of the erupting tooth. However, it is essential to acknowledge that this theory encounters challenges in cases where a tooth erupts without fully formed roots or when tooth eruption persists after root formation. Some teeth extend their eruption beyond a distance greater than their total root length. Moreover, the newly formed dentin at the root apex remains unmineralized and susceptible to trauma, which raises doubts regarding the exclusive reliance on root-driven forces for tooth eruption.[7]
Vascular or hydrostatic pressure theory
The pressure theory suggests that a localized rise in tissue fluid pressure within the vessels of the dental pulp and the periapical region generates hydrodynamic and hydrostatic forces, believed to contribute to tooth eruption.[8]
Bone remodeling theory or dental follicle theory
Osteoblasts and osteoclasts, originating from the dental follicle, induce bone remodeling by initiating resorption in the coronal area while concurrently promoting bone apposition in the apical region. This coordinated activity creates a pathway through which the tooth can undergo passive eruption.[5][9]
Periodontal ligament traction theory
According to this theory, the force that causes teeth to erupt is generated by the periodontal ligament-dental follicle complex, which exerts a pulling force through the traction power of fibroblasts when they contract.[10]
Contemporary Theories of Eruption
Bite forces theory
Recent theories suggest that the soft tissues within the dental follicle can detect bite forces, which are believed to have a crucial role in directing bone remodeling processes and influencing tooth eruption.[11]
Innervation-provoked pressure theory
According to this theory, the innervation within the root membrane generates pressure in the apical aspect of the tooth, ultimately resulting in tooth eruption.[12]
The equilibrium theory
Once the tooth reaches its functional plane, an additional eruption is stimulated by the vertical growth of the lower jaw, which moves away from the maxilla. With the expanding available space, the tooth continues to erupt, maintaining appropriate occlusal contact with the corresponding teeth in the opposing arch.
Neuromuscular theory
According to the neuromuscular theory, the active eruption of a tooth is driven by the coordinated and balanced forces exerted by the orofacial muscles, all of which are controlled by the central nervous system. These well-coordinated neuromuscular forces are transformed into various forms of energy, including electrical, electrochemical, and biomechanical energies. The energies are formed to stimulate a cascade of cellular and molecular responses within and around the dental follicle and enamel organ. This action prepares a pathway and initiates other essential cellular functions necessary for the eruption of a developing tooth.
Eruption Patterns
The eruption timing of deciduous and permanent teeth can exhibit significant variation. The eruption sequence holds greater significance than the timing, as it may vary between deciduous and permanent teeth. Usually, a variation of up to 6 months before or after the typical eruption date is considered within the normal range.
The initial teeth to emerge in the oral cavity of a child are the deciduous mandibular central incisors, typically appearing around 5 to 8 months of age (see Image. Penetrating Incisor), followed by the maxillary central incisors, normally erupting 1 to 2 months later. In general, by the age of 19 months, a child should have a total of 12 erupted deciduous teeth. Children should typically have 16 deciduous teeth by 23 months, and all of the deciduous teeth should emerge by 27 months.
The first permanent teeth that emerge in the oral cavity are the maxillary and mandibular first molars (see Image. First Sign of Right Incisor Breakthrough). These teeth typically emerge around age 6 and are called 6-year molars. These molars erupt distal to the deciduous second molars and are accompanied or preceded by the exfoliation of the deciduous mandibular central incisors. The permanent mandibular incisors typically erupt in individuals aged 6 to 7, followed by the permanent maxillary incisors between the ages of 7 and 9. The permanent anterior teeth develop lingual or palatal to the deciduous teeth. In contrast, the permanent premolars grow in the spaces between and beneath the roots of the deciduous molars they replace.
Clinical Significance
Tooth eruption is an intricate and meticulously regulated process that influences the healthy development of the craniofacial region. Factors such as eruption timing, sequence, direction, rate, position, and morphology of teeth significantly contribute to facial aesthetics and phonetics.[13] Predicting the eruption schedule is a valuable tool for strategizing a child's dental care, which includes diagnostic, preventive, and therapeutic measures.[14]
In forensic dentistry, the eruption is critical for diagnosing specific growth disturbances and estimating a child's chronological age when their birth records are unknown.[15] Moreover, comprehending the eruption schedule is crucial for proactively managing occlusion, particularly when deciding the ideal timing for deciduous tooth extractions and initiating orthodontic treatment.[16]
Disruptions in tooth eruption present frequent challenges in dental practice, manifesting as delays, complete impairment, premature eruption, or teeth emerging in ectopic positions. A summary of the prevalent complications associated with tooth eruption is provided below.
Ectopic Eruption
An ectopic eruption is a tooth following a path that deviates from the norm.[17] Timely diagnosis and management of ectopic teeth are essential to prevent future malocclusion. Various factors, including ethnicity, gender, and individual traits, influence the variation in tooth position. A localized traumatic injury can displace 1 or more tooth buds, resulting in an ectopic eruption of the affected teeth. Other local factors contributing to ectopic eruptions include the presence of fibrous tissue, supernumerary teeth, arch length deficiency, and the retention or premature loss of deciduous teeth.
There are also reports of nasal teeth, which emerge as supernumerary structures within the nasal cavity.[18] Nasal teeth can either be asymptomatic or symptomatic, causing symptoms such as facial pain, nasal cavity obstruction, headaches, epistaxis, foul-smelling rhinorrhea, external nasal deformities, and nasolacrimal duct obstruction.[18]
Delayed Eruption
When the timing of tooth emergence significantly deviates from the established norms associated with ethnicity and gender, it is referred to as delayed eruption.[2] Delayed eruption can result from various causes, including local factors such as mucosal barriers, gingival fibromatosis, odontogenic and nonodontogenic tumors, premature loss of a primary tooth, and radiation damage. Moreover, delayed eruption can be associated with systemic conditions and endocrine disorders such as hypothyroidism,[19] hypopituitarism, hypoparathyroidism, and certain medications.[2]
Prolonged chemotherapy or medication usage, including aspirin, acetaminophen, ibuprofen, indomethacin, and bisphosphonates, may inhibit the prostaglandin pathway. This inhibition may decrease osteoclastic activity in periodontal tissues, ultimately slowing down the rate of tooth eruption.
Chronic and prolonged malnutrition, often associated with vitamin deficiencies during childhood, is another factor that also correlates with delayed eruption.[2] Moreover, various syndromes have been identified as causing delayed eruption, including Down syndrome, Gardner syndrome, cleidocranial dysostosis, anhidrotic ectodermal dysplasia, Hutchinson-Gilford syndrome, Bloch–Sulzberger syndrome, Apert syndrome, and Axenfeld–Rieger syndrome.[2]
Impacted Teeth
Impacted teeth cannot erupt due to a physical barrier obstructing their normal eruption path.[2] Among impacted teeth, mandibular third molars are the most frequently affected.
Embedded Teeth
Embedded teeth remain unerupted in cases with no physical obstruction along their path, primarily because of insufficient eruptive force.[2]
Submerged Teeth
Teeth that become ankylosed following initial eruption are called submerged teeth. As a result, they lose the ability to continue erupting as the jaws grow.[2]
Primary Failure of Eruption
Primary failure of eruption refers to the partial or complete failure of a tooth's eruption.[20] In this condition, the tooth's eruption path forms correctly but does not successfully complete the eruption process.[20]
Intraosseous Ectopic Migration of Unerupted Teeth
Primary failure of eruption is a rare phenomenon, affecting less than 1% of the population. This condition is commonly observed in females and occurs within the mandibular arch. This condition typically involves the mandibular second premolar or the mandibular canine.[21][22]
Premature Eruption
The premature eruption of teeth can be attributed to various factors, including genetic abnormalities, disruptions in endocrine function involving the pituitary, thyroid, and gonads, congenital syphilis, local factors such as excessive resorption of the overlying bone, and environmental factors such as exposure to pollutants, including toxic polyhalogenated aromatic hydrocarbons, polychlorinated biphenyls, polychlorinated dibenzodioxins, and dibenzofurans. In addition, poor maternal health and episodes of fever during pregnancy can also contribute to premature tooth eruption.
Natal and Neonatal Teeth
Premature or early tooth eruption refers to the eruption of teeth before their expected schedule. Teeth already present in the oral cavity at birth are termed natal teeth, while those that erupt within the first month of life are called neonatal teeth.[23]
Natal teeth are 3 times more prevalent than neonatal teeth and are most frequently found in the mandibular anterior area, particularly the central incisors. Maxillary incisors, mandibular canines or molars, and maxillary canines may also follow natal teeth in prevalence.
The presence of natal or neonatal teeth can potentially cause ulceration on the ventral surface of the tongue, often due to the sharp incisal edge of the tooth.[24] This condition is referred to as Riga-Fede disease or syndrome. Since the root development of these teeth is incomplete, they are mobile, increasing the risk of swallowing and aspiration teeth. Other potential complications include injury to the mother's breast and difficulties in the infant's ability to suckle.[24] The mobility of these teeth has also been linked to the degeneration of Hertwig epithelial root sheath, which plays a crucial role in root formation. The deterioration of this sheath further contributes to incomplete root development.
Certain syndromes have been reported to be associated with the occurrence of natal and neonatal teeth. These syndromes include chondroectodermal dysplasia, Rubinstein-Taybi syndrome, Pierre Robin syndrome, neonatal progeria, cleft lip or palate, ectodermal dysplasia, craniofacial dysostosis, and Down syndrome.
Eruption Cyst
An eruption hematoma is typically asymptomatic and characterized by a bluish swelling over an erupting tooth. This condition results from the accumulation of blood-tinged fluid within the follicle surrounding the erupting tooth.[25] These hematomas typically rupture spontaneously without the need for treatment. However, in some cases, the cyst's size may cause discomfort and interfere with the ability to eat.
Detrimental Habits That Affect Tooth Eruption
Digit sucking
This habit affects the eruption path of maxillary incisors, causing them to protrude. This occurs because the habit disrupts the balance between the outward force exerted by the tongue musculature against the palate and the inward force of the cheek musculature.[26]
Tongue thrust
Children with a tongue thrust habit exert increased outward force through the tongue musculature, which can alter the eruption pathway of maxillary incisors.[27]
Lip sucking or biting
Lip-sucking or biting habits, especially involving the lower lip, create inward pressure from the lip musculature. This increased pressure, in turn, causes an alteration in the eruption path of the mandibular incisors.[28]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
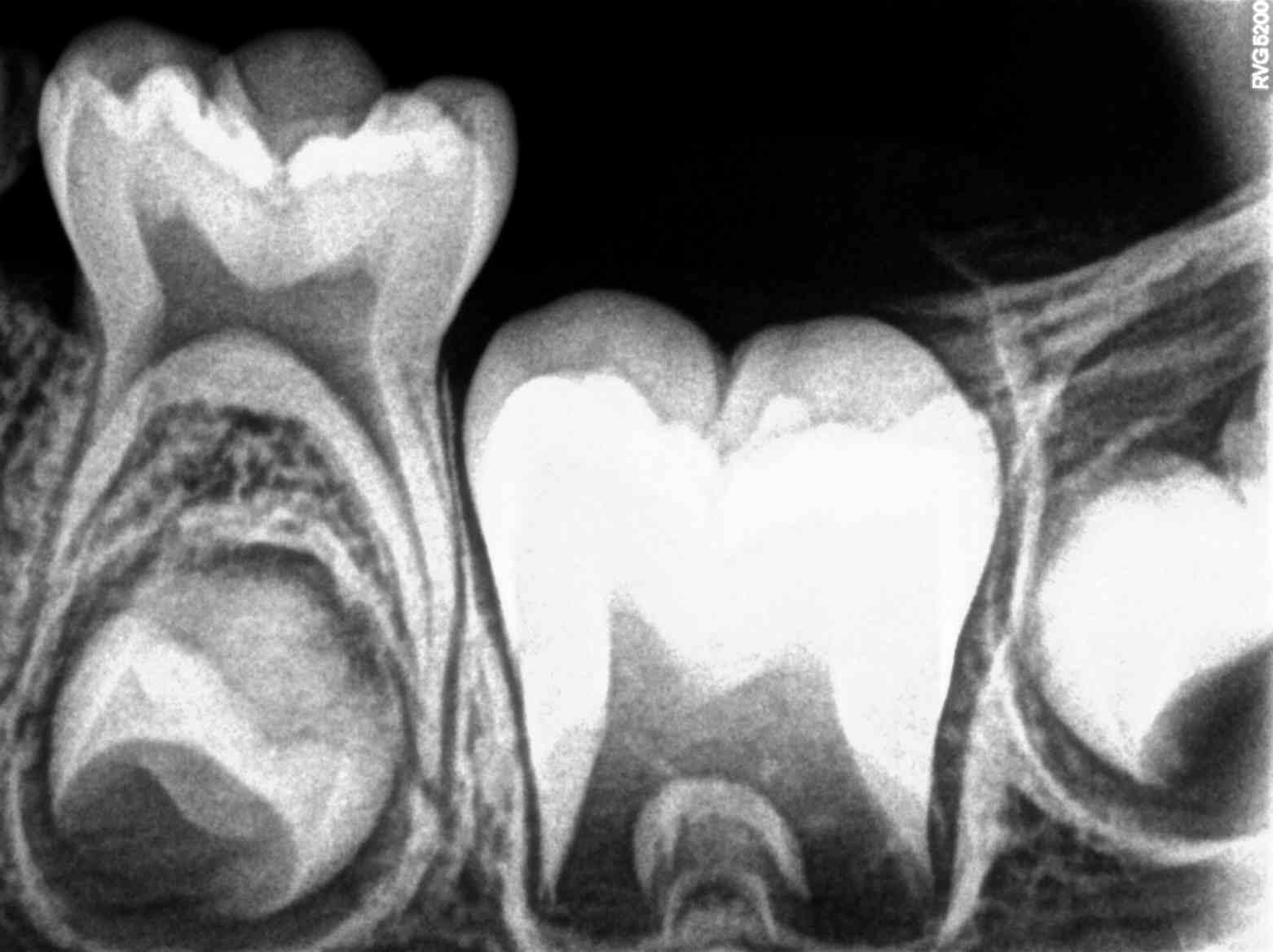
Post-Occlusal Eruption. Intraoral Periapical Radiograph (IOPA) of a boy aged 5 years showing primary tooth #75 and developing crowns of permanent teeth #35, #36, and #37. Note the eruption path for tooth #36 has been completed and is now in a post-emergence eruption stage.
Contributed By Nizil Shah - Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=75101299
References
Marks SC Jr. The basic and applied biology of tooth eruption. Connective tissue research. 1995:32(1-4):149-57 [PubMed PMID: 7554911]
Level 3 (low-level) evidenceSuri L, Gagari E, Vastardis H. Delayed tooth eruption: pathogenesis, diagnosis, and treatment. A literature review. American journal of orthodontics and dentofacial orthopedics : official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 2004 Oct:126(4):432-45 [PubMed PMID: 15470346]
Marks SC Jr, Schroeder HE. Tooth eruption: theories and facts. The Anatomical record. 1996 Jun:245(2):374-93 [PubMed PMID: 8769674]
Level 3 (low-level) evidenceProffit WR, Frazier-Bowers SA. Mechanism and control of tooth eruption: overview and clinical implications. Orthodontics & craniofacial research. 2009 May:12(2):59-66. doi: 10.1111/j.1601-6343.2009.01438.x. Epub [PubMed PMID: 19419448]
Level 3 (low-level) evidenceCahill DR, Marks SC Jr. Tooth eruption: evidence for the central role of the dental follicle. Journal of oral pathology. 1980 Jul:9(4):189-200 [PubMed PMID: 6777476]
Level 3 (low-level) evidenceMoxham BJ, Berkovitz BK. The mobility of the lathyritic rabbit mandibular incisor in response to axially-directed extrusive loads. Archives of oral biology. 1984:29(10):773-8 [PubMed PMID: 6594088]
Level 3 (low-level) evidenceTopouzelis N, Tsaousoglou P, Pisoka V, Zouloumis L. Dilaceration of maxillary central incisor: a literature review. Dental traumatology : official publication of International Association for Dental Traumatology. 2010 Oct:26(5):427-33. doi: 10.1111/j.1600-9657.2010.00915.x. Epub [PubMed PMID: 20831640]
Sutton PR, Graze HR. The blood-vessel thrust theory of tooth eruption and migration. Medical hypotheses. 1985 Nov:18(3):289-95 [PubMed PMID: 3853083]
Marks SC Jr, Cahill DR. Experimental study in the dog of the non-active role of the tooth in the eruptive process. Archives of oral biology. 1984:29(4):311-22 [PubMed PMID: 6586126]
Level 3 (low-level) evidenceKasugai S, Suzuki S, Shibata S, Yasui S, Amano H, Ogura H. Measurements of the isometric contractile forces generated by dog periodontal ligament fibroblasts in vitro. Archives of oral biology. 1990:35(8):597-601 [PubMed PMID: 2256814]
Level 3 (low-level) evidenceSarrafpour B, Swain M, Li Q, Zoellner H. Tooth eruption results from bone remodelling driven by bite forces sensed by soft tissue dental follicles: a finite element analysis. PloS one. 2013:8(3):e58803. doi: 10.1371/journal.pone.0058803. Epub 2013 Mar 15 [PubMed PMID: 23554928]
Kjær I. Mechanism of human tooth eruption: review article including a new theory for future studies on the eruption process. Scientifica. 2014:2014():341905. doi: 10.1155/2014/341905. Epub 2014 Feb 12 [PubMed PMID: 24688798]
Gorski JP, Marks SC Jr. Current concepts of the biology of tooth eruption. Critical reviews in oral biology and medicine : an official publication of the American Association of Oral Biologists. 1992:3(3):185-206 [PubMed PMID: 1571471]
Level 3 (low-level) evidenceSoliman NL, El-Zainy MA, Hassan RM, Aly RM. Timing of deciduous teeth emergence in Egyptian children. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit. 2011 Nov:17(11):875-81 [PubMed PMID: 22276498]
Level 2 (mid-level) evidenceAlmonaitiene R, Balciuniene I, Tutkuviene J. Factors influencing permanent teeth eruption. Part one--general factors. Stomatologija. 2010:12(3):67-72 [PubMed PMID: 21063135]
Hughes TE, Bockmann MR, Seow K, Gotjamanos T, Gully N, Richards LC, Townsend GC. Strong genetic control of emergence of human primary incisors. Journal of dental research. 2007 Dec:86(12):1160-5 [PubMed PMID: 18037648]
Yaseen SM, Naik S, Uloopi KS. Ectopic eruption - A review and case report. Contemporary clinical dentistry. 2011 Jan:2(1):3-7. doi: 10.4103/0976-237X.79289. Epub [PubMed PMID: 22114445]
Level 3 (low-level) evidenceThawley SE, LaFerriere KA. Supernumerary nasal tooth. The Laryngoscope. 1977 Oct:87(10 Pt 1):1770-3 [PubMed PMID: 904416]
Level 3 (low-level) evidenceVucic S, Korevaar TIM, Dhamo B, Jaddoe VWV, Peeters RP, Wolvius EB, Ongkosuwito EM. Thyroid Function during Early Life and Dental Development. Journal of dental research. 2017 Aug:96(9):1020-1026. doi: 10.1177/0022034517708551. Epub 2017 May 10 [PubMed PMID: 28489513]
Hanisch M, Hanisch L, Kleinheinz J, Jung S. Primary failure of eruption (PFE): a systematic review. Head & face medicine. 2018 Mar 15:14(1):5. doi: 10.1186/s13005-018-0163-7. Epub 2018 Mar 15 [PubMed PMID: 29544499]
Level 1 (high-level) evidenceSutton PR. Migrating nonerupted mandibular premolars: a case of migration into the coronoid process. Oral surgery, oral medicine, and oral pathology. 1968 Jan:25(1):87-98 [PubMed PMID: 5235661]
Level 3 (low-level) evidenceShapira Y, Kuftinec MM. Intrabony migration of impacted teeth. The Angle orthodontist. 2003 Dec:73(6):738-43; discussion 744 [PubMed PMID: 14719741]
Mhaske S, Yuwanati MB, Mhaske A, Ragavendra R, Kamath K, Saawarn S. Natal and neonatal teeth: an overview of the literature. ISRN pediatrics. 2013 Aug 18:2013():956269. doi: 10.1155/2013/956269. Epub 2013 Aug 18 [PubMed PMID: 24024038]
Level 3 (low-level) evidenceAdekoya-Sofowora CA. Natal and neonatal teeth: a review. The Nigerian postgraduate medical journal. 2008 Mar:15(1):38-41 [PubMed PMID: 18408782]
Bodner L, Goldstein J, Sarnat H. Eruption cysts: a clinical report of 24 new cases. The Journal of clinical pediatric dentistry. 2004 Winter:28(2):183-6 [PubMed PMID: 14969381]
Level 3 (low-level) evidenceKumar V, Shivanna V, Kopuri RC. Knowledge and attitude of pediatricians toward digit sucking habit in children. Journal of the Indian Society of Pedodontics and Preventive Dentistry. 2019 Jan-Mar:37(1):18-24. doi: 10.4103/JISPPD.JISPPD_136_18. Epub [PubMed PMID: 30804303]
Kurihara K, Fukui T, Sakaue K, Hori K, Ono T, Saito I. The effect of tongue thrusting on tongue pressure production during swallowing in adult anterior open bite cases. Journal of oral rehabilitation. 2019 Oct:46(10):895-902. doi: 10.1111/joor.12820. Epub 2019 May 25 [PubMed PMID: 31081951]
Level 3 (low-level) evidenceAgrawal S, Koirala B, Dali M, Shrestha S, Bhagat T, Niraula SR. Prevalence of Oral Habits of Schoolchildren in the Mixed Dentition in Dharan, Nepal. Journal of dentistry for children (Chicago, Ill.). 2019 May 15:86(2):88-92 [PubMed PMID: 31395113]