Introduction
Rapid sequence intubation (RSI) is a technique used when rapid control of the airway is needed as a precaution for patients who may have risks of pulmonary aspiration. This method is utilized by clinicians across multiple medical specialties, including critical care physicians, anesthesiologists, and emergency medical personnel.
RSI is indicated for a patient in acute respiratory failure due to inadequate oxygenation or ventilation and for airway protection in a patient with an altered mental status. A systematic approach to RSI is important to ensure the procedure's success. The clinician should assess the risk before the intervention and place the patient in an optimal position with an understanding of the anatomy involved. All necessary supplies must be available at the bedside, including alternative options to secure the airway in case of failure.[1]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Assessing Airway Risk
Several parameters need to be evaluated before the start of the procedure. Multiple mnemonics, including L.E.M.O.N., exist to help a clinician determine if an airway will be difficult.[2]
- L: Look externally (facial trauma, beard, loose teeth, dentures, large incisors); these factors can indicate a difficult airway.
- E: Evaluate the 3-3-2 rule
- Can 3 fingers fit between the incisors?
- Can 3 fingers fit between the tip of the chin and the hyoid bone?
- Can 2 fingers fit from the top of the thyroid notch to the hyoid bone?
- A decrease in these distances can be an indication of a difficult airway.
- M: Mallampati score; assess how much of the posterior pharynx and uvula can be seen (a higher Mallampati score indicates a more difficult airway).
- Mallampati 1 score: Indicates that the entirety of the uvula can be visualized
- Mallampati 2 score: Indicates that half of the uvula can be visualized
- Mallampati 3 score: Indicates that only the base of the uvula can be visualized
- Mallampati 4 score: Indicates that the uvula cannot be visualized
- O: Obstruction or obesity
- Obesity (body mass index >30) can predict a difficult airway.
- Obstruction of the airway, including head and neck cancer and epiglottitis, can indicate a difficult airway.
- N: Neck mobility
- Assess the neck's mobility; a neck that cannot be maneuvered into an ideal position due to trauma, a C-collar, or rigidity can lead to a more difficult airway.
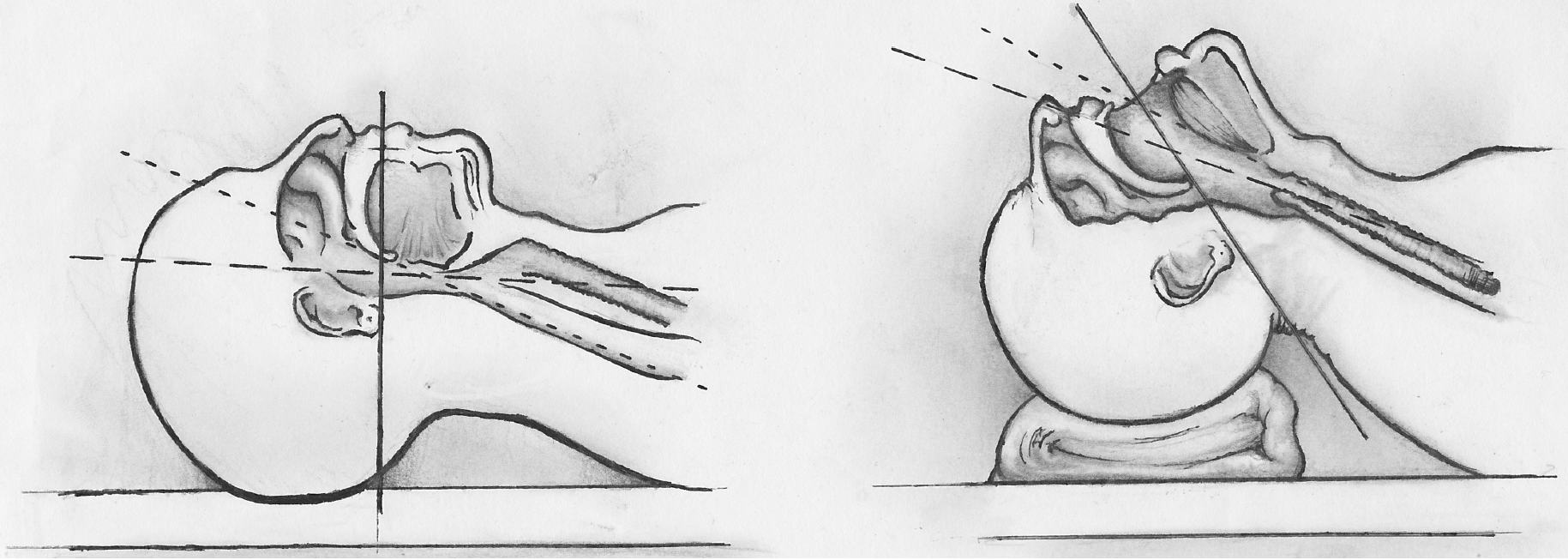
Positioning and Anatomy
Proper patient positioning is vital to the success of the procedure. Ideally, the neck should be flexed at the lower cervical spine (C6-C7) and extended at the upper cervical spine (C1-C2). This position is called the "sniffing position." It allows for the best visualization of the anatomy, including the epiglottis and vocal cords (see Image. Sniffing Position).
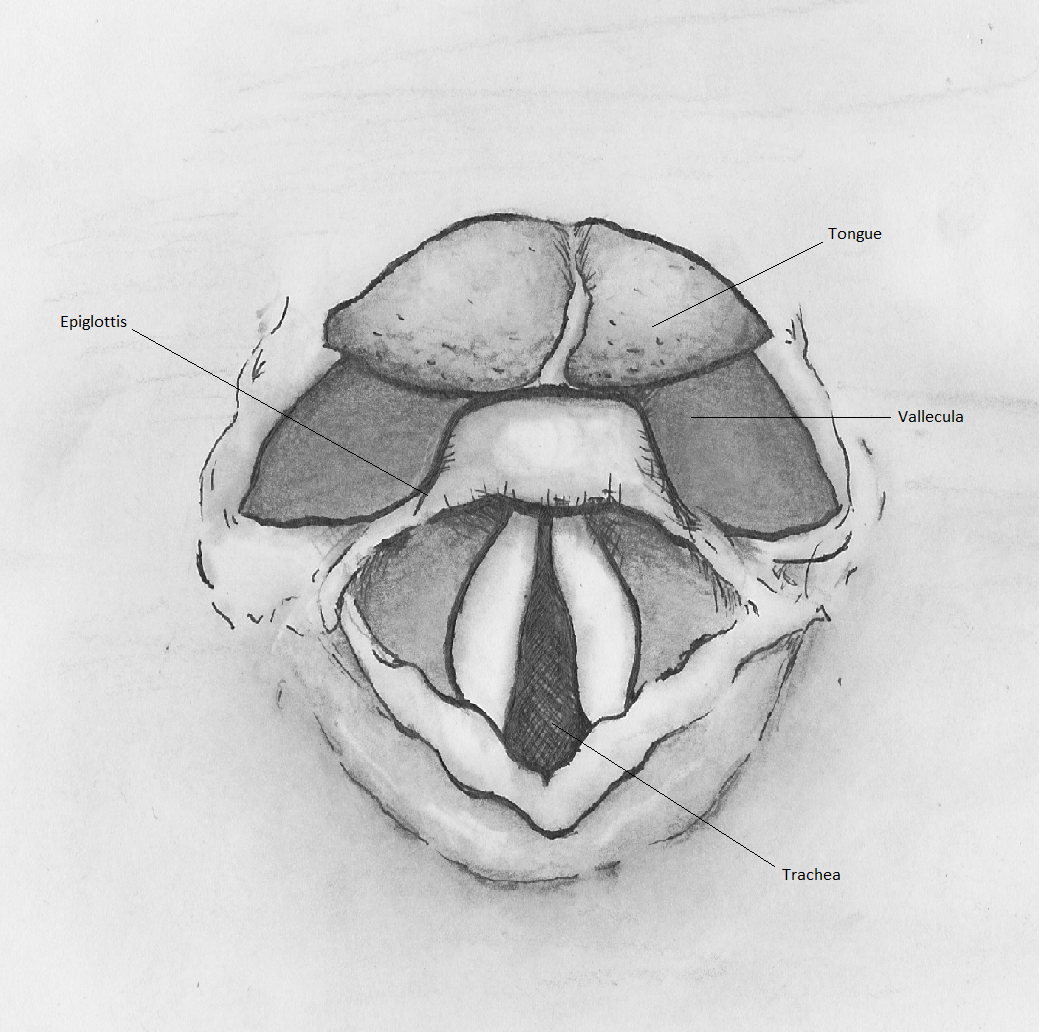
The epiglottis serves as the primary landmark that will direct successful endotracheal intubation. The origin of the epiglottis can be found at the base of the tongue. The valley between the tongue and the epiglottis is called the vallecula. When intubating with a Macintosh blade (discussed later), the tip of the blade should ideally be placed at the base of the tongue in the vallecula, and a ventral and inferior movement of the blade reveals the vocal cords.
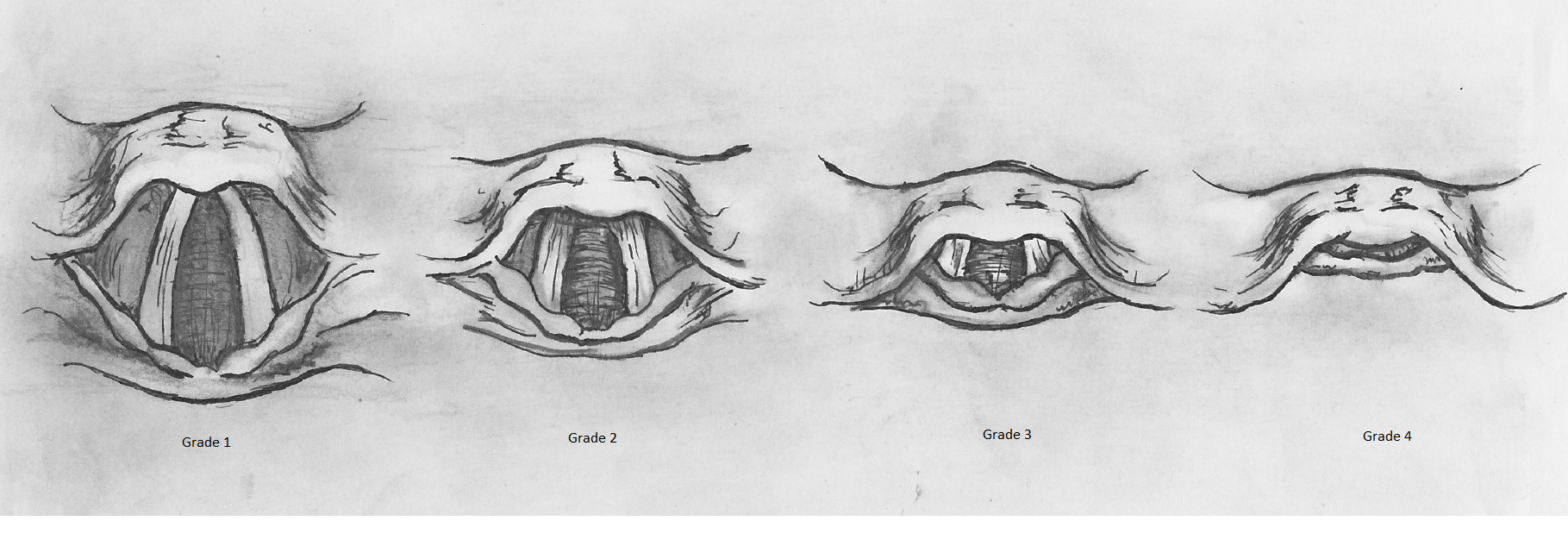
The Cormack and Lehane Grading system allows the provider to evaluate their view of the vocal cord and estimate the chance of successful intubation. A Grade 1 view of the cords using this system indicates a high likelihood of successful intubation. In this grade, the provider can see nearly the entirety of the vocal cord anatomy. Successive grades reveal fewer cords and a decreased rate of successful intubation (see Image. Cormack-Lehane Grading System).
Indications
RSI is indicated for a patient in acute respiratory failure due to poor oxygenation or ventilation and for a patient who cannot protect their airway due to altered mental status. RSI may also be used in a patient with an acute upper gastrointestinal bleed with a high risk of aspiration.[3]
Contraindications
There are few absolute contraindications for rapid sequence intubation. These contraindications include complete upper airway obstruction and the loss of facial or oropharyngeal landmarks, which will require a surgical airway to be placed.
Relative contraindications are related to issues that may lead to procedural failure, which can be due to injuries to the airway, anatomic abnormalities, and the proficiency of the clinician.[4] These relative contraindications can be evaluated using the L.E.M.O.N. mnemonic and Cormack and Lehane Grading system discussed above.[5]
Equipment
There are many supplies necessary in preparation for rapid sequence intubation:
- Endotracheal tube with an inflatable cuff with sterile lubricant
- Laryngoscope handle and blades
- Suction (x2)
- Bag valve mask
- End-tidal carbon dioxide monitor
- Induction agents
- Tracheal tube inducer (bougie)
- Supraglottic airway, such as laryngeal mask airway
- Video-assisted laryngoscopy
- Pulse oximetry
- IV access
- Push dose pressors (see Image. Equipment for Endotracheal Intubation).[6][7]
Before initiating the procedure, the clinician should ensure adequate lighting for the room. The clinician should test the lighting source on the laryngoscope and the inflation of the endotracheal tube. An easily viewed pulse oximeter should also be available.
Endotracheal Tube Size
Generally, a 7.0- to 7.5-mm internal diameter tube should be placed in a female patient, and a 7.5- to 8.0-mm tube should be placed in a male. Smaller tube sizes are not adequate for performing a bronchoscopy if necessary.
Blade Selection
The most commonly used laryngoscope blades are the Macintosh and Miller blades. The Macintosh blade has a curved spatula used to approximate the curvature of the tongue and move the epiglottis, mandible, hyoid bone, and other soft tissues out of the view of the glottis (see Image. Superior View of the Glottis). A Macintosh 3 has a 13-cm blade and fits most average-sized adults. A Macintosh 4 blade is 15.5 cm, allowing the practitioner to utilize a longer blade if necessary. The Macintosh blade should be placed inside the vallecula at the base of the tongue. A flat Miller blade is designed to go over the epiglottis to reveal the vocal cords.
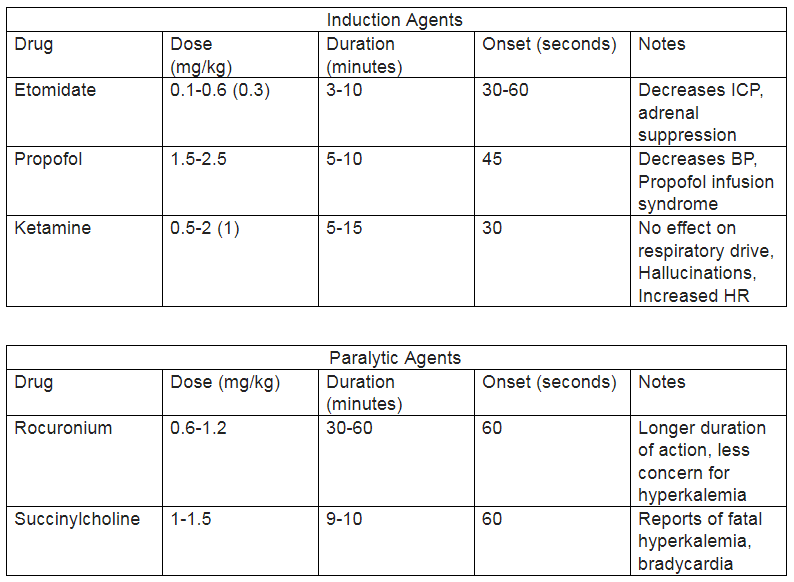
Induction Agents
An in-depth discussion of the agents used to induce and paralyze patients undergoing RSI is outside the scope of this article. However, below are two charts of the frequently used induction and paralytic agents and their differing characteristics (see Image. Induction and Paralytic Medications).
Technique or Treatment
Once the patient, supplies, and team have been properly prepared, induction agents can be administered to the patient first, followed by paralytic agents (see Image. Induction and Paralytic Medications). The bag valve mask should be utilized to pre-oxygenate the patient as much as possible. The clinician performing the rapid sequence intubation should ensure a tight seal of the bag valve mask to the patient's face.[8]
After allowing the paralytic agents to take effect after 60 seconds, the patient's mouth should be opened with the scissoring technique. The scissoring technique involves placing the right thumb on the right middle finger and inserting the right hand into the patient's mouth. The clinician then "scissors" the patient's mouth open, crossing the thumb and middle finger. The laryngoscope should then be inserted into the patient's mouth with a sweeping motion from right to left, moving the tongue out of view.
The clinician should locate the epiglottis and place the laryngoscope in the vallecula. A ventral and inferior motion should be performed with a rigid wrist without abduction or "rocking" of the wrist. Suctioning can be performed to obtain a better view and clear debris, and pressure can be applied to the thyroid cartilage to manipulate the glottis into view. Once the clinician has located the glottis, the endotracheal tube can be passed through the vocal cords. Once passed, the stilette can be removed from the endotracheal tube. The tube should be advanced based on the Chula formula: endotracheal tube depth=0.1 (height in cm) + 4. This equation will give the depth at which the endotracheal tube should be advanced when measured at the patient's teeth.
The cuff should be inflated after the tube is advanced to the proper distance. End-tidal capnography, condensation on the endotracheal tube, and bilateral lung sounds should all be used to verify placement initially. A chest X-ray should be performed to assure adequate placement.[9]
Complications
Multiple tools can be used when the clinician cannot place the endotracheal tube with direct laryngoscopy using the standard technique.
- A video-assisted laryngoscope can be used to view the glottis better.
- A grade 4 Cormack and Lehane view of the anatomy may prompt the clinician to utilize the tracheal tube inducer or bougie. A bougie is a long rod-shaped medical device with a curve at the tip. This item is introduced into the patient’s airway, and an attempt is made to place the tube inside the trachea. If the bougie is swept along the trachea's wall, the tracheal rings' signature ridges can be felt. The endotracheal tube can then be introduced over the bougie, and the bougie will guide the endotracheal tube into the trachea.
- A supraglottic airway, such as a laryngeal mask airway, can be placed if endotracheal intubation is not possible.[10][11]
Enhancing Healthcare Team Outcomes
At least 2 to 3 medical professionals must manage the airway for rapid sequence intubation. A clear delineation of roles is necessary for successful endotracheal intubation. The lead clinician is responsible for directing the team, managing the patient's airway, and intubating the patient.
A nursing staff member is responsible for providing induction and paralytic medications at the onset of the procedure. The nurse should wait for the clinician performing the intubation to give their approval before administering medications. An independently trained clinician who can procure equipment, operate the bag valve mask, apply cricoid pressure, and confirm tube placement after the intubation is completed should also be at the bedside. Discussion and preparation for a backup plan in case of procedure failure should be addressed before the start of the procedure.
Media
(Click Image to Enlarge)
References
Mosier JM, Sakles JC, Law JA, Brown CA 3rd, Brindley PG. Tracheal Intubation in the Critically Ill. Where We Came from and Where We Should Go. American journal of respiratory and critical care medicine. 2020 Apr 1:201(7):775-788. doi: 10.1164/rccm.201908-1636CI. Epub [PubMed PMID: 31895986]
Saoraya J, Vongkulbhisal K, Kijpaisalratana N, Lumlertgul S, Musikatavorn K, Komindr A. Difficult airway predictors were associated with decreased use of neuromuscular blocking agents in emergency airway management: a retrospective cohort study in Thailand. BMC emergency medicine. 2021 Mar 25:21(1):37. doi: 10.1186/s12873-021-00434-2. Epub 2021 Mar 25 [PubMed PMID: 33765918]
Level 2 (mid-level) evidenceGopinath B, Sachdeva S, Kumar A, Kumar G. Advancing emergency airway management by reducing intubation time at a high-volume academic emergency department. BMJ open quality. 2021 Jul:10(Suppl 1):. doi: 10.1136/bmjoq-2021-001448. Epub [PubMed PMID: 34344738]
Level 2 (mid-level) evidenceFouche PF, Meadley B, StClair T, Winnall A, Stein C, Jennings PA, Bernard S, Smith K. Temporal changes in blood pressure following prehospital rapid sequence intubation. Emergency medicine journal : EMJ. 2022 Jun:39(6):451-456. doi: 10.1136/emermed-2020-210887. Epub 2021 Jul 16 [PubMed PMID: 34272210]
Cadamy AJ, Booth MG. Rapid sequence induction. Anaesthesia. 1999 Aug:54(8):817 [PubMed PMID: 10460710]
Level 3 (low-level) evidenceBotha JC, Lourens A, Stassen W. Rapid sequence intubation: a survey of current practice in the South African pre-hospital setting. International journal of emergency medicine. 2021 Aug 17:14(1):45. doi: 10.1186/s12245-021-00368-3. Epub 2021 Aug 17 [PubMed PMID: 34404352]
Level 3 (low-level) evidenceAvery P, Morton S, Raitt J, Lossius HM, Lockey D. Rapid sequence induction: where did the consensus go? Scandinavian journal of trauma, resuscitation and emergency medicine. 2021 May 13:29(1):64. doi: 10.1186/s13049-021-00883-5. Epub 2021 May 13 [PubMed PMID: 33985541]
Level 3 (low-level) evidenceFakhry SM, Scanlon JM, Robinson L, Askari R, Watenpaugh RL, Fata P, Hauda WE, Trask A. Prehospital rapid sequence intubation for head trauma: conditions for a successful program. The Journal of trauma. 2006 May:60(5):997-1001 [PubMed PMID: 16688061]
Level 2 (mid-level) evidenceKriege M, Lang P, Lang C, Pirlich N, Griemert EV, Heid F, Wittenmeier E, Schmidtmann I, Schmidbauer W, Jänig C, Jungbecker J, Kunitz O, Strate M, Schmutz A. Anaesthesia protocol evaluation of the videolaryngoscopy with the McGrath MAC and direct laryngoscopy for tracheal intubation in 1000 patients undergoing rapid sequence induction: the randomised multicentre LARA trial study protocol. BMJ open. 2021 Oct 6:11(10):e052977. doi: 10.1136/bmjopen-2021-052977. Epub 2021 Oct 6 [PubMed PMID: 34615684]
Level 1 (high-level) evidenceGrant S, Pellatt RA, Shirran M, Sweeny AL, Perez SR, Khan F, Keijzers G. Safety of rapid sequence intubation in an emergency training network. Emergency medicine Australasia : EMA. 2021 Oct:33(5):857-867. doi: 10.1111/1742-6723.13742. Epub 2021 Feb 9 [PubMed PMID: 33565240]
Roshan R, Dhanapal SG, Joshua V, Madhiyazhagan M, Amirtharaj J, Priya G, Abhilash KP. Aspiration during Rapid Sequence Induction: Prevalence and Risk Factors. Indian journal of critical care medicine : peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2021 Feb:25(2):140-145. doi: 10.5005/jp-journals-10071-23714. Epub [PubMed PMID: 33707890]