Introduction
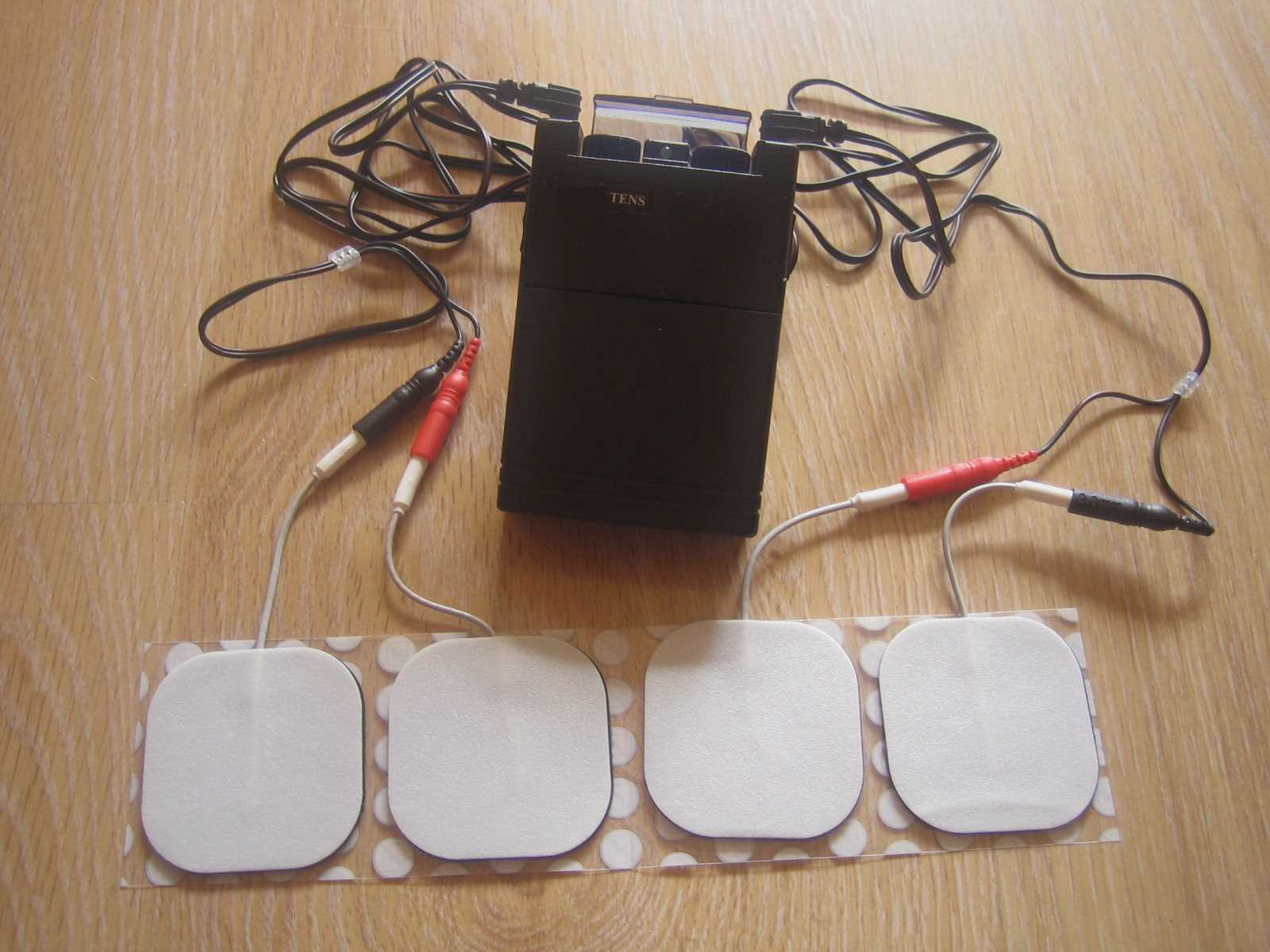
Transcutaneous electrical nerve stimulation, or TENS, is a therapeutic approach employing electric current to activate peripheral nerves for pain relief. The TENS unit, a compact, often battery-powered device, can easily fit into a pocket (see Image. Transcutaneous Electrical Nerve Stimulator). Electrodes are applied to the skin around the targeted region and connected to the TENS unit via wires. Users can then adjust the pulse amplitude, frequency, duration, and pattern of the currents. Thus, high user tolerance is achieved with minimal side effects and no potential for overdose.[1][2] Low frequencies (<10 Hz) and high intensity induce muscle contractions, while high frequencies (>50 Hz) with low intensity produce paresthesia without contractions.[3]
The historical debate over TENS efficacy persists despite proven clinical benefits. Disagreements persist regarding the appropriateness of TENS for specific pain syndromes and conditions. TENS has a rich history dating back to around 60 A.D. when Roman physician Scribonius Largus proposed using an "electric fish" for relief. Electric eels were also historically utilized for pain management benefits. By the 18th century, various devices aimed to treat multiple conditions with electrostatic exposures. A device for clinical therapy using electricity called the "Electreat" was introduced in the 19th century, but its use was discontinued due to limitations.
The modern concept of TENS is credited to American neurosurgeon Dr. C. Norman Shealy. His training at Duke University and additional experience at Barnes-Jewish Hospital and Massachusetts General Hospital led to the development of today's TENS units. Dr. Shealy aimed to create an impactful therapy for migraines, back pain, and gout. As the study of TENS advanced, new techniques emerged, including intense TENS, acupuncture TENS, and conventional TENS.[4]
While the medical community engages in an ongoing debate about the efficacy of TENS, a clearer picture is likely to form as more trials emerge with optimal dosing and specific outcome measures. Despite the controversy and confusion surrounding TENS, numerous studies point towards positive outcomes in pain management. Acknowledging contraindications is crucial, yet the risk of complications or side effects is minimal when TENS is operated within manufacturer parameters. For those willing to explore alternative avenues, the fusion of TENS with pharmacotherapy holds promise.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
TENS works through several peripheral and central mechanisms to reduce hyperalgesia. At the peripheral level, TENS activates either large-diameter, low-threshold, non-noxious afferents (A-β) or small-diameter, high-threshold peripheral afferents (A-δ) to unlock the cascade of postulated mechanisms. This targeted stimulation reduces pain by mitigating nociceptor activity and curtailing unwanted sensations.[5][6] Molecular studies indicate that the activity and expression of key pain-related ion channels, including voltage-gated sodium channels in the peripheral nerves, are modulated by TENS, inhibiting nociceptors' neurotransmission.[7]
Afferent input leads to the activation of descending inhibitory pathways within the periaqueductal gray (PAG) area, rostral ventromedial medulla (RVM), and spinal cord. TENS curbs the activity in the Rexed laminae I to V of the dorsal horn.[7] Communication with these areas occurs with different neurotransmitters and receptors. Concentrations of β-endorphins and methionine-enkephalin, which both interact with opioid receptors, have been shown to increase after high-frequency TENS. Activation of opioid receptors reduces glutamate and substance P release in the spinal cord, thus reducing excitability and potentially decreasing the risk of central sensitization. GABA-A and muscarinic receptors for high-frequency TENS are implicated in mediating CNS effects. Low-frequency TENS utilizes all these receptors in the CNS in addition to serotonin.[8]
Differences in TENS frequency used during treatment are important considerations as they affect which receptor mediates the analgesic effects. Specifically, low-frequency treatment is mediated by the μ-receptor, and the δ-opioid receptor mediates high-frequency treatment. This is relevant for patients using opioid medications for pain relief as the efficacy of low-frequency treatment may be blunted in this population.[9]
Peripheral mechanisms are also crucial to the efficacy of TENS. Interestingly, blockage of peripheral α-2A adrenergic receptors, not central α-receptors, prevents TENS analgesia.[8]
Indications
TENS has been used for the following conditions.
- Postoperative pain
- Acute non-postoperative pain
- Low back pain
- Osteoarthritis pain
- Diabetic peripheral neuropathy
- Fibromyalgia
- Neuropathic pain, eg, spinal cord injury [10]
Its versatility makes TENS a formidable ally in pain management, catering to acute and chronic cases. However, a schism within the scientific community persists regarding its efficacy for specific pain types or conditions fueled by methodological concerns.[11] This is due to the lack of high-quality studies or disagreement between existing high-quality studies.[10]
Three distinct kinds of TENS emerge, each with its conceptual indications:
- Intense TENS: Functioning as a "counter-irritant," this type zeroes in on small-diameter, high-threshold cutaneous afferents (A-δ), deploying high frequencies and intensities for brief intervals.[5]
- Acupuncture-like TENS (AL-TENS): Geared for hyperstimulation, AL-TENS steps in for patients unresponsive to conventional TENS. It employs titration to low frequency, higher intensity, and extended pulse width, targeting small-diameter, high-threshold peripheral afferents (A-δ).[12]
- Conventional TENS: This high-frequency, low-intensity, and short pulse duration approach selectively stimulates large-diameter, low-threshold, non-noxious afferents (A-β). This variation finds its niche in treating dermatomal pain distributions.
Literature evaluating the use of these different modalities in various kinds of pain (eg, acute, non-postoperative, chronic, etc) demonstrates that TENS is effective at treating various types of pain. Often, there was no significant difference in the amount of analgesia between modalities, with some exceptions for specific pathologies such as rheumatoid arthritis.[10]
Although high-frequency TENS has shown to be more beneficial than low-frequency TENS, the number of high-quality RCTs are insufficient to recommend the application of TENS for chronic pelvic pain or dysmenorrhea.[13]
Affecting 10% to 24% of the general population, chronic neck pain has not been overtly responsive to TENS therapy.[14]
Contraindications
Correctly administering TENS demands understanding its contraindications. Contraindications include pregnancy, epilepsy, and the presence of a pacemaker.[6] However, TENS use is possible in these patient populations if not applied to the abdomen, head, or chest.[2] Precision in electrode pad placement is paramount, and users must avoid areas prone to skin irritation.[15] Electrodes should not be placed over active, treatable tumors or close to transdermal drug delivery systems.[2]
Equipment
The manufacturer's instruction booklet should be consulted before TENS equipment use. Today's TENS units, compact and lightweight, offer a seamless integration into daily life. However, caution dictates that sessions exclude operating heavy machinery, driving, or aquatic endeavors. Electrode pad placement, adept power management, and precise setting titration are pillars for practical TENS application.[11] Pads are generally placed on relevant dermatomes, but there are a few scenarios where this is contraindicated, including sites over the neck, face, and chest, as these sites contain electrically sensitive structures. It is recommended that most patients increase the intensity to the maximum strength while still being comfortable to derive the most benefit from treatments.[2]
Technique or Treatment
It is imperative to read the manufacturer's instruction booklet, as each unit might have slight variances in recommendations. TENS units are now small and lightweight. Patients can place them in their pocket, on a desk, or hold them. Treatment sessions occur at the patient's convenience except while operating heavy machinery, driving, bathing, showering, or swimming. The unit should be powered off before placing the pads. Electrode pad placement is at least 1 inch apart in the appropriate dermatomal region of the targeted pain. The skin underlying the pad placement must have an intact sensation. After powering the unit, the setting titration follows the manufacturer's recommendations. Red and black lead placement have little impact on clinical outcomes.
Complications
Despite its safety profile, there are cautions associated with TENS use.[16] Due to potential complications, individuals with pacemakers, epilepsy, or those in the throes of pregnancy are universally advised against TENS use. Theoretical risks extend to transdermal drug delivery systems and dermatologic concerns, urging a cautious approach.[15] Steering clear of TENS during activities like driving or operating heavy machinery mitigates potential complications.
Clinical Significance
A consensus on the efficacy of TENS in pain management has not been achieved, but the tapestry of positive outcomes is evident with prudent usage. Short-term triumphs demand strategic breaks and dynamic electrode pad placement. TENS seamlessly integrates into diverse clinical settings, necessitating formal pain assessments and crystal-clear instructions before initiation.
TENS is not a cure for pain conditions or syndromes and should only be offered as a tool for symptomatic pain relief.[13]
The positive impact that TENS has on an individual might diminish over time. Habituation might even lead to a worsening of pain. Recommendations are that patients take breaks from treatment, modulate between high frequency and low frequency within treatment sessions, increase the intensity of TENS daily, and vary their placement of electrode pads over time.[10]
Other methods of preventing analgesic tolerance include pharmacologic blockade of NMDA-glutamate receptors (such as ketamine or dextromethorphan) or CCK receptors in the spinal cord.[8]
Regarding acute postoperative pain, efficacy is contingent upon investigators utilizing adequate TENS parameters and specific pain reduction outcomes. Adequate TENS parameters are defined by sufficient frequency and proper intensity. Adequate frequency is defined as 1 to 8 Hz for LF-TENS and 25 to 150 Hz for HF TENS, while adequate intensity is defined as solid sub-noxious, maximum tolerable, or >15 mA. If these parameters are strictly adhered to, then a significant reduction in postoperative opiate use (36%) is observed. Additionally, TENS is more effective in treating the pain associated with postoperative movements, such as walking or incentive spirometer use, but not in reducing pain at rest. Investigators have proposed that future trials should distinctly analyze movement pain from resting to assess the efficacy of TENS in treating acute postoperative pain.[8]
Enhancing Healthcare Team Outcomes
TENS emerges as a linchpin in various clinical domains, from hospice and palliative care to orthopedic surgery. However, before embarking on TENS treatment, a formal pain assessment led by seasoned professionals becomes paramount.[17] Clear and understandable instructions pave the way, with monitored sessions guided by trained providers ensuring optimal understanding and utilization of TENS for pain management.[6] The collaborative synergy of nurses, allied health professionals, and clinicians is pivotal, guaranteeing a comprehensive grasp of TENS's potential in pain management.
Media
(Click Image to Enlarge)
References
DeSantana JM, Walsh DM, Vance C, Rakel BA, Sluka KA. Effectiveness of transcutaneous electrical nerve stimulation for treatment of hyperalgesia and pain. Current rheumatology reports. 2008 Dec:10(6):492-9 [PubMed PMID: 19007541]
Level 3 (low-level) evidenceJohnson M. Transcutaneous Electrical Nerve Stimulation: Mechanisms, Clinical Application and Evidence. Reviews in pain. 2007 Aug:1(1):7-11. doi: 10.1177/204946370700100103. Epub [PubMed PMID: 26526976]
Chao AS, Chao A, Wang TH, Chang YC, Peng HH, Chang SD, Chao A, Chang CJ, Lai CH, Wong AMK. Pain relief by applying transcutaneous electrical nerve stimulation (TENS) on acupuncture points during the first stage of labor: a randomized double-blind placebo-controlled trial. Pain. 2007 Feb:127(3):214-220. doi: 10.1016/j.pain.2006.08.016. Epub 2006 Oct 6 [PubMed PMID: 17030438]
Level 1 (high-level) evidenceAinsworth L, Budelier K, Clinesmith M, Fiedler A, Landstrom R, Leeper BJ, Moeller L, Mutch S, O'Dell K, Ross J, Radhakrishnan R, Sluka KA. Transcutaneous electrical nerve stimulation (TENS) reduces chronic hyperalgesia induced by muscle inflammation. Pain. 2006 Jan:120(1-2):182-187. doi: 10.1016/j.pain.2005.10.030. Epub 2005 Dec 19 [PubMed PMID: 16360266]
Liebano RE, Rakel B, Vance CGT, Walsh DM, Sluka KA. An investigation of the development of analgesic tolerance to TENS in humans. Pain. 2011 Feb:152(2):335-342. doi: 10.1016/j.pain.2010.10.040. Epub 2010 Dec 8 [PubMed PMID: 21144659]
Morgan B, Jones AR, Mulcahy KA, Finlay DB, Collett B. Transcutaneous electric nerve stimulation (TENS) during distension shoulder arthrography: a controlled trial. Pain. 1996 Feb:64(2):265-267. doi: 10.1016/0304-3959(95)00107-7. Epub [PubMed PMID: 8740603]
Shi Y, Wu W. Multimodal non-invasive non-pharmacological therapies for chronic pain: mechanisms and progress. BMC medicine. 2023 Sep 29:21(1):372. doi: 10.1186/s12916-023-03076-2. Epub 2023 Sep 29 [PubMed PMID: 37775758]
Vance CGT, Dailey DL, Chimenti RL, Van Gorp BJ, Crofford LJ, Sluka KA. Using TENS for Pain Control: Update on the State of the Evidence. Medicina (Kaunas, Lithuania). 2022 Sep 22:58(10):. doi: 10.3390/medicina58101332. Epub 2022 Sep 22 [PubMed PMID: 36295493]
Gibson W, Wand BM, Meads C, Catley MJ, O'Connell NE. Transcutaneous electrical nerve stimulation (TENS) for chronic pain - an overview of Cochrane Reviews. The Cochrane database of systematic reviews. 2019 Feb 19:2(2):CD011890. doi: 10.1002/14651858.CD011890.pub2. Epub 2019 Feb 19 [PubMed PMID: 30776855]
Level 1 (high-level) evidenceVance CG, Dailey DL, Rakel BA, Sluka KA. Using TENS for pain control: the state of the evidence. Pain management. 2014 May:4(3):197-209. doi: 10.2217/pmt.14.13. Epub [PubMed PMID: 24953072]
Sluka KA, Bjordal JM, Marchand S, Rakel BA. What makes transcutaneous electrical nerve stimulation work? Making sense of the mixed results in the clinical literature. Physical therapy. 2013 Oct:93(10):1397-402. doi: 10.2522/ptj.20120281. Epub 2013 May 2 [PubMed PMID: 23641031]
Radhakrishnan R, King EW, Dickman JK, Herold CA, Johnston NF, Spurgin ML, Sluka KA. Spinal 5-HT(2) and 5-HT(3) receptors mediate low, but not high, frequency TENS-induced antihyperalgesia in rats. Pain. 2003 Sep:105(1-2):205-13 [PubMed PMID: 14499437]
Paley CA, Wittkopf PG, Jones G, Johnson MI. Does TENS Reduce the Intensity of Acute and Chronic Pain? A Comprehensive Appraisal of the Characteristics and Outcomes of 169 Reviews and 49 Meta-Analyses. Medicina (Kaunas, Lithuania). 2021 Oct 4:57(10):. doi: 10.3390/medicina57101060. Epub 2021 Oct 4 [PubMed PMID: 34684097]
Martimbianco ALC, Porfírio GJ, Pacheco RL, Torloni MR, Riera R. Transcutaneous electrical nerve stimulation (TENS) for chronic neck pain. The Cochrane database of systematic reviews. 2019 Dec 12:12(12):CD011927. doi: 10.1002/14651858.CD011927.pub2. Epub 2019 Dec 12 [PubMed PMID: 31830313]
Level 1 (high-level) evidenceSluka KA, Vance CG, Lisi TL. High-frequency, but not low-frequency, transcutaneous electrical nerve stimulation reduces aspartate and glutamate release in the spinal cord dorsal horn. Journal of neurochemistry. 2005 Dec:95(6):1794-801 [PubMed PMID: 16236028]
Radhakrishnan R, Sluka KA. Spinal muscarinic receptors are activated during low or high frequency TENS-induced antihyperalgesia in rats. Neuropharmacology. 2003 Dec:45(8):1111-9 [PubMed PMID: 14614954]
Reeves JL 2nd,Graff-Radford SB,Shipman D, The effects of transcutaneous electrical nerve stimulation on experimental pain and sympathetic nervous system response. Pain medicine (Malden, Mass.). 2004 Jun; [PubMed PMID: 15209969]