Introduction
Trauma is the leading cause of death worldwide. In the United States, trauma is the leading cause of death in young adults and accounts for ten percent of death in all men and women. In the U.S., there are approximately 50 million visits to the emergency department annually related to trauma. The most common causes of mortality in trauma victims include hemorrhage, cardiopulmonary arrest, and multiple organ dysfunction syndromes.[1]
The assessment of trauma victims requires an organized and systematic approach. When caring for a trauma victim, physicians, nurses, and support staff must work together and communicate effectively. The goal of assessing trauma victims is identifying immediate life threats and stabilizing the patient.
Technique or Treatment
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Technique or Treatment
Prehospital
The first step in trauma assessment begins prior to the patient's arrival. This includes gathering the care team, equipment, and initial information. Emergency medical services (EMS) should provide information including mechanism of injury, patient vital signs, obvious injury, current interventions, and patient's age and sex if available. After receiving this information, the healthcare team members should begin thinking of possible injuries that may be a threat to the patient's life. The trauma team may vary based on the hospital location and staffing but should, at a minimum, include a physician and nurse. Once the team is present, and ideally before the patient arrives, roles should be assigned. There must be one individual assigned as a team leader, usually the physician. Other roles may include documentation, airway management, IV access, attaching monitoring devices, and medication administration. The team leader should assign the roles and be in charge of the direction and decision making upon patient arrival and throughout the assessment.[2] With the initial information provided by emergency medical services (EMS) and the team assembled, all equipment should be gathered and prepared. It is important to prepare equipment needed for intubation, cardiac monitoring, intravenous access, or intraosseous access, and any other intervention that may be indicated by the initial information received. Additional equipment and interventions might also be required beyond those anticipated by the prearrival report, and having ready access to additional resources is also important.
Primary Survey
Upon patient arrival, the room should be quiet, and EMS should briefly present the patient and their findings. Depending on the patient's condition, the primary survey may have to start during the EMS presentation. If this occurs, every effort should be made to obtain the pertinent information from EMS before their departure. Advanced Trauma Life Support (ATLS), developed by the American College of Surgeons, promotes the primary survey sequence as airway, breathing, circulation, disability, exposure (ABCDE).
Airway
Airway obstruction is a major, preventable cause of death in trauma victims, and therefore it is the initial step of the primary survey.[3] Assessing the conscious patient's airway starts with talking to the patient. Ask the patient their name to see if they respond clearly and appropriately. This will help assess the patency of the airway. Airway evaluation also includes a visual inspection of the patient. Look for signs of respiratory distress, listen for stridor, inspect the face, oral cavity, and neck, as well as palpate the patient's neck and face. When inspecting and palpating the patient, look for oral or dental injury, obstructions to intubation, such as unstable midface fractures, and even location for possible cricothyrotomy. If the patient is unconscious or not protecting their airway, they should be intubated immediately. If unable to intubate, cricothyrotomy should be performed. If intubating cervical spine immobilization must be maintained. If the patient requires intubation, be sure that the endotracheal tube remains secure as accidental extubation is a leading cause of morbidity in trauma patients.[4]
Breathing
Once the airway is secured or maintained by the patient, breathing and ventilation should be assessed. This involves visual inspection of the patient's chest, looking for injury. Look for paradoxical chest movement, which indicates flail chest, penetrating injury, or tracheal deviation. Auscultate the lungs listening for decreased breath sounds. Palpate the chest for signs of crepitus. If the patient has signs of tension pneumothorax, immediate needle decompression or chest thoracostomy should be performed. Evaluate the patient's oxygen saturation. Ultrasound or x-ray imaging of the chest should be considered as an adjunct to the physical exam.
Circulation
The assessment of circulation focuses on hemorrhage control and maintaining adequate perfusion. Hemorrhage has been identified as the most common cause of preventable death in trauma victims.[1] Start by visually evaluating the patient looking for external hemorrhage or signs of shock like pallor. Palpate the patient's carotid and femoral pulses while assessing if the skin is cold and diaphoretic. The patient's mentation can also offer clues to how well they are perfusing their vital organs, but care should be taken to rely on this in patients with a possible head injury. In the presence of external bleeding, control should be attempted by direct pressure. In the case of arterial bleed from an extremity, a tourniquet can be applied. If the patient does not have palpable central pulses, further investigation and intervention are needed. The 5 locations to look for major hemorrhage include the thorax, peritoneal cavity, retroperitoneal cavity, pelvic or long bone fractures, and externally. The focused assessment using sonography in trauma (FAST) exam may be used to assess for intra-abdominal hemorrhage. In patients with shock, isotonic intravenous fluids can be initially administered, but blood products are preferred in a 1 to 1 to 1 ratio of red blood cells to plasma to platelets for patients with ongoing fluid requirements and concerns for hemorrhage.[5][6] Be aware that the trauma victim may be on anticoagulation, and this may need to be reversed.[7] Shock may also be caused by tension pneumothorax, cardiac tamponade, or spinal cord injury. The FAST exam and extended FAST exam (includes pulmonary evaluation) also aid in the diagnosis of cardiac tamponade and pneumothorax. Thoracotomy may be performed if an intrathoracic cause of shock is suspected. Establishing adequate IV access in trauma patients is also of critical importance. Two large-bore peripheral IVs, or functioning intraosseous access, should be established early in the evaluation period. Cardiac monitoring should also be established as soon as feasible.
Disability
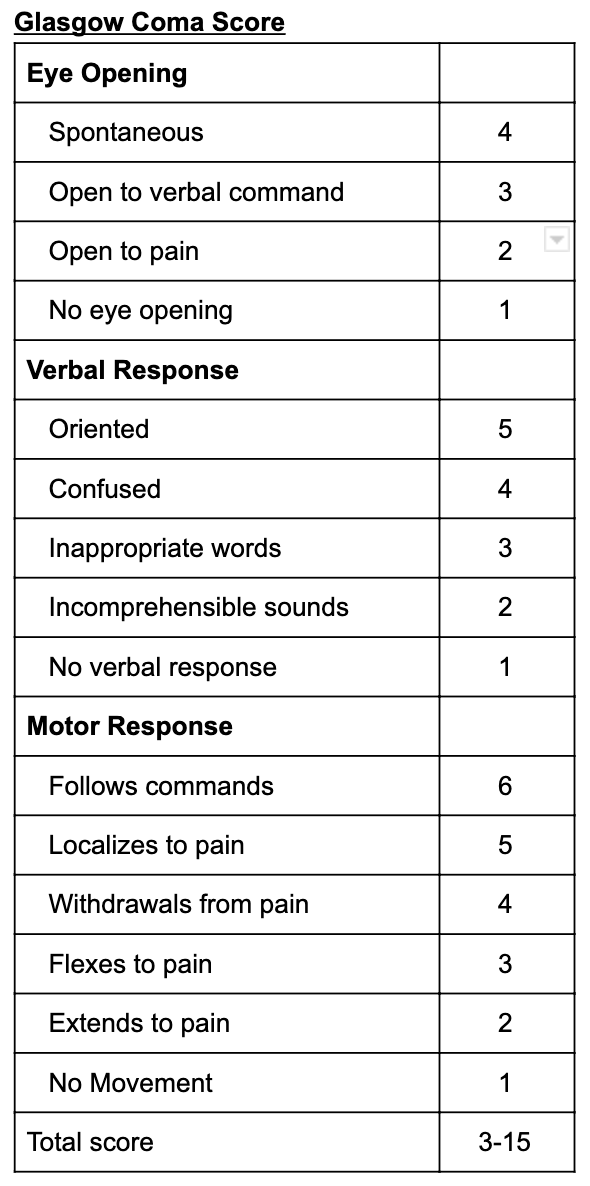
Once airway, breathing, and circulation have been evaluated and stabilized, the patient's neurologic function should be assessed. Measure the patient's consciousness using the Glasgow coma score (GCS) (Table 1, GCS chart). For patients with a GCS of 8 or less, consideration should be given to definitive airway control (if not already achieved). Check pupils for size and reactivity. Assess the patient's motor ability and sensation in all four extremities to look for signs of spinal cord injury. Cervical spine immobilization should be maintained.
Exposure
The fifth and final step of the primary survey includes removing all clothing to assess for signs of injury such as gunshot wounds, stab wounds, abrasions, lacerations, ecchymosis, or any other traumatic findings. During this stage, it is important to remember to keep the patient warm as hypothermia can lead to multiorgan failure.[8]
Secondary Survey
Once the patient is stabilized, and if they do not need immediate surgical intervention, a secondary assessment is performed. The secondary assessment involves further history from the patient, a thorough head-to-toe exam, and diagnostic testing. The four most commonly missed diagnoses during the survey are blunt abdominal trauma with internal organ injury, penetrating abdominal trauma, penetrating thoracic trauma, and extremity trauma such as fractures and compartment syndrome.[9] Further history should include the patient's past medical and surgical history, medications, and allergies. When possible, ask about the details of the traumatic event and mechanism of injury and allow this to guide the secondary assessment further. If the patient is unable to communicate, it is even more critical to get as much pertinent information as possible from EMS. For blunt trauma, important questions may include speed, seatbelt use, object damage, and/or height of a fall. For penetrating trauma, it is helpful to know what penetrated the patient, the length of the knife or penetrating objects, and potentially the number of gunshots heard. The patient's past medical history, past surgical history, allergies, medications, and social history need to be obtained if possible. It is important to know if the patient is on any anticoagulants or antiplatelet medications, as well as any other medications that might affect the physiologic response to hemorrhage. A full head-to-toe physical exam should be performed, starting with the head and face. Examine the head for lacerations, abrasions, foreign bodies, bony malformations, and unstable midface bones. Examine the ears for hemotympanum, TM rupture, blood within the canal, and external trauma. Examine the eyes for papilledema, globe rupture, unequal pupils, abrasion, and foreign body. Inspect the nose for bleeding or septal hematoma. Inspect the mouth for dental injury, bleeding, and posterior oropharynx obstruction, swelling, or edema. Next, move on to the neck exam by palpating for bony injury, crepitus, midline trachea, lacerations, hematomas, and abrasions. Cervical immobilization should be maintained while performing these exam elements. Following the neck exam, move on to examine the chest. Inspect and palpate the chest, looking for obvious deformity, areas of ecchymosis, penetrating wounds, crepitus, and flail chest. Flail chest is a moving segment of ribs secondary to multiple ribs fractured in more than one place. This is often an indicator of underlying lung injury and may cause difficulty breathing. Take more in-depth auscultation of lung sounds in all fields. Examine the patient's work of breathing by looking at the respiratory rate, accessory muscle use, or inspiratory retractions. After evaluating the patient's chest, inspect the abdomen by looking for distension, tenderness to palpation, penetrating injury, abrasions, seatbelt sign, and/or bruising. Evaluate the patient's flank and back as well, again looking for any signs of injury or bony abnormalities. Bruising along the patient's bilateral flanks or surrounding the patient's umbilicus may represent a retroperitoneal hemorrhage. Evaluate the patient's rectum as well as a genitourinary exam. A digital rectal exam may be performed when fully assessing the patient's disability (neurologic function). Evaluate for the presence of blood or perineal injury. Evaluate the patient's genitals looking for any bleeding, ecchymosis, or lacerations. Foley catheter may be placed as an adjunct but should be avoided without further evaluation if blood is noted at the meatus. The musculoskeletal exam follows and includes a thorough examination of all four extremities. Palpate extremities to assess for pain, decreased temperature, or tension that may indicate compartment syndrome. Evaluate the color of extremities looking for pallor that indicates possible blood loss and cyanosis that may indicate decreased oxygen perfusion. Look for bruising, laceration, abrasion, open fractures, bony abnormalities, and active bleeding. Palpate the pelvis for stability. It is also important to evaluate the patient's back while maintaining spine precautions. Look for penetrating injuries, palpate for step-offs along the spine, evaluate for bruising and bony tenderness. Perform a full neurologic exam, including testing the cranial nerves, strength, sensation, coordination, and reflexes. During the secondary evaluation, X-rays may be performed for evaluation of the lungs and pelvis and any other areas of pain or tenderness that may have been injured. CT scan may be performed to evaluate an internal head injury, cervical spine injury, internal chest or abdomen injury, and pelvic injury. Patients that are not hemodynamically stable should not be taken out of the resuscitation area for imaging studies.
Complications
There are several pitfalls in the evaluation of trauma patients that should be avoided if at all possible. If a patient has a clinical deterioration during the trauma evaluation, do not continue with the next step in the evaluation. Immediately go back to the ABCDE evaluation of the patient as this is most likely to identify a life-threatening condition. Similarly, do not be distracted by obvious injuries such as burns, open extremity fractures, or penetrating injuries and, therefore, not follow the sequence of ABCDE evaluation. Another pitfall to avoid is not to send the hemodynamically unstable patient away from the resuscitation area to obtain testing, such as X-rays or CT scans. Further, do not delay transfer to definitive care, if not at the highest level of care, to obtain tests or perform unnecessary procedures. Once the identification of the need to transfer to a higher level of care is identified, the transfer process should be initiated.
Clinical Significance
Traumatic injuries are seen daily in the emergency department. It is important to be familiar with the process of trauma assessment in each health care provider's place of work. An efficient and thorough trauma assessment leads to decreased morbidity and mortality.
Enhancing Healthcare Team Outcomes
Assessing and caring for a trauma victim is a team effort and requires proper organization and effective communication. Poor patient outcomes can occur from missed diagnosis, communication errors, and lack of situational awareness. To avoid missing a diagnosis, there are several things to remember. Assume the worst-case scenario, listen carefully to EMS but remember that the information may be inaccurate, repeatedly reassess the patient, cooperate and be professional with other members of the trauma team, and never get stuck on your initial diagnosis. To avoid communication errors, it is crucial to have one team leader. The team leader is responsible for assigning roles and specific tasks. The team leader should continuously update the entire team of new findings and changes in the patient’s stability and change in the overall plan. Closed-loop communication should be used at all times. To maintain situational awareness, the team leader should encourage all members of the team to announce any concerns or abnormal findings. Proper patient monitoring and constant reevaluation of the patient will help maintain situational awareness.[10]
Summary
The trauma assessment begins prior to the patient’s arrival with information gathering, the formation of the trauma team, and equipment preparation. On patient arrival, the team begins with the primary survey, which includes an assessment of the patient’s airway, breathing, circulation, disability, and exposure. Once the patient has been stabilized, and if they don’t require surgical intervention, the secondary survey begins. This involves a thorough history and physical exam to avoid missing an injury. Patient outcomes can be improved with efficient teamwork and effective communication. One team leader should lead the trauma assessment, and closed-loop communication should be used at all times.
Nursing, Allied Health, and Interprofessional Team Interventions
The nursing team carries out actions during the assessment of trauma victims. Prior to patient arrival, the nursing staff is assigned roles. It is essential to know your role and prepare to perform the actions necessary for that role. Common roles include documentation, placing the patient on cardiac monitoring, obtaining vital signs, placing an intravenous catheter, obtaining a glucose level, drawing labs, obtaining an electrocardiogram, administering medications, and participating in CPR. If a nurse is assigned a role that they are unable to perform, it is important to inform the physician of this so the role may be reassigned. On patient arrival, the nursing staff should perform their assigned roles. When administering any medication, the name of the medication, dose, and route of administration should be repeated prior to giving the drug and once it has been given. The documenting nurse keeps a log of exam findings and actions performed as well as the time that the actions occurred. The nursing team can help improve patient outcomes by repeating back what they are asked to do before the action is completed. This improves communication and accuracy of treatment. Nursing should also voice any concerns and provide any suggestions that they feel may help the patient.
Media
References
Teixeira PG, Inaba K, Hadjizacharia P, Brown C, Salim A, Rhee P, Browder T, Noguchi TT, Demetriades D. Preventable or potentially preventable mortality at a mature trauma center. The Journal of trauma. 2007 Dec:63(6):1338-46; discussion 1346-7. doi: 10.1097/TA.0b013e31815078ae. Epub [PubMed PMID: 18212658]
Kaufman EJ, Richmond TS, Wiebe DJ, Jacoby SF, Holena DN. Patient Experiences of Trauma Resuscitation. JAMA surgery. 2017 Sep 1:152(9):843-850. doi: 10.1001/jamasurg.2017.1088. Epub [PubMed PMID: 28564706]
Hussain LM, Redmond AD. Are pre-hospital deaths from accidental injury preventable? BMJ (Clinical research ed.). 1994 Apr 23:308(6936):1077-80 [PubMed PMID: 8173428]
Level 2 (mid-level) evidenceKovacs G, Sowers N. Airway Management in Trauma. Emergency medicine clinics of North America. 2018 Feb:36(1):61-84. doi: 10.1016/j.emc.2017.08.006. Epub [PubMed PMID: 29132582]
Ley EJ, Clond MA, Srour MK, Barnajian M, Mirocha J, Margulies DR, Salim A. Emergency department crystalloid resuscitation of 1.5 L or more is associated with increased mortality in elderly and nonelderly trauma patients. The Journal of trauma. 2011 Feb:70(2):398-400. doi: 10.1097/TA.0b013e318208f99b. Epub [PubMed PMID: 21307740]
Level 2 (mid-level) evidenceCannon JW, Khan MA, Raja AS, Cohen MJ, Como JJ, Cotton BA, Dubose JJ, Fox EE, Inaba K, Rodriguez CJ, Holcomb JB, Duchesne JC. Damage control resuscitation in patients with severe traumatic hemorrhage: A practice management guideline from the Eastern Association for the Surgery of Trauma. The journal of trauma and acute care surgery. 2017 Mar:82(3):605-617. doi: 10.1097/TA.0000000000001333. Epub [PubMed PMID: 28225743]
Ferraris VA, Bernard AC, Hyde B. The impact of antiplatelet drugs on trauma outcomes. The journal of trauma and acute care surgery. 2012 Aug:73(2):492-7 [PubMed PMID: 23019676]
Level 2 (mid-level) evidenceHess JR, Brohi K, Dutton RP, Hauser CJ, Holcomb JB, Kluger Y, Mackway-Jones K, Parr MJ, Rizoli SB, Yukioka T, Hoyt DB, Bouillon B. The coagulopathy of trauma: a review of mechanisms. The Journal of trauma. 2008 Oct:65(4):748-54. doi: 10.1097/TA.0b013e3181877a9c. Epub [PubMed PMID: 18849786]
Brooks A, Holroyd B, Riley B. Missed injury in major trauma patients. Injury. 2004 Apr:35(4):407-10 [PubMed PMID: 15037376]
Level 2 (mid-level) evidenceMackersie RC. Pitfalls in the evaluation and resuscitation of the trauma patient. Emergency medicine clinics of North America. 2010 Feb:28(1):1-27, vii. doi: 10.1016/j.emc.2009.10.001. Epub [PubMed PMID: 19945596]