Introduction
Ulnar nerve entrapment generally occurs in the cubital tunnel at the level of the elbow or in the ulnar tunnel at the level of the wrist. The exact location of the compression will affect the presentation. To understand the symptoms seen in patients with ulnar nerve entrapment, it is necessary to understand the anatomy of the ulnar nerve.
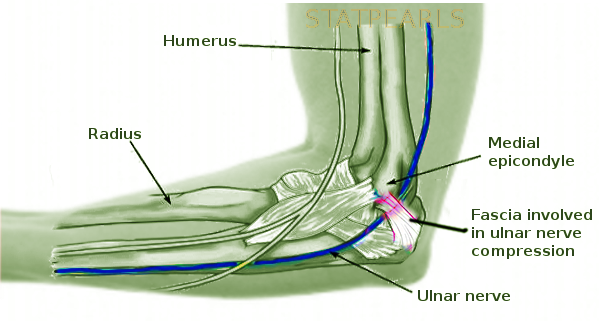
The ulnar nerve is the continuation of the medial cord of the brachial plexus and lies posteromedial to the brachial artery in the anterior compartment of the upper arm. It pierces through the medial intermuscular septum at the arcade of Struthers, which is located approximately 8 cm proximal to the medial epicondyle. Traveling behind the medial epicondyle with the superior ulnar collateral artery, the ulnar nerve enters the forearm through the cubital tunnel, which is defined as the space between the posterior and transverse bands of the medial collateral ligament (deep) and Obsbourne's ligament (superficial), which refers to the extension of the fascia spanning the two heads of the flexor carpi ulnaris (FCU). Compression at the level of the cubital tunnel is most frequently due to compression by Osborne's ligament.
In the forearm, the ulnar nerve travels between the flexor carpi ulnaris (FCU) and the flexor digitorum profundus (FDP). The ulnar nerve provides motor innervation to both the FCU and the FDP controlling flexion of the distal interphalangeal joint (DIP) of the ring and small fingers.
The ulnar nerve and ulnar artery enter Guyon's canal, or the ulnar tunnel at the wrist, which is bordered by the transverse carpal ligament (deep), volar carpal ligament (superficial), pisiform (ulnar), and hook of the hamate (radial). The ulnar nerve lies ulnarly and posteriorly to the ulnar artery within Guyon's canal. Guyon's canal is further subdivided into 3 zones: zone 1 is proximal to the bifurcation of the ulnar nerve into the deep motor branch and the superficial sensory branch. Zone 2 is distal to zone 1, surrounding only the motor branch. Zone 3 is distal to zone 2, and surrounding only the superficial sensory branch of the ulnar nerve.
Therefore, compression or pathology at the cubital tunnel or zone 1 of Guyon's canal results in a motor and sensory deficit of the ulnar nerve. Pathology in zone 2 of Guyon's canal will result in an isolated motor deficit, while dysfunction in zone 3 of Guyon's canal will result in an isolated sensory deficit.[1][2]
The ulnar nerve is crucial for innervating the intrinsic musculature of the hand, which includes the adductor pollicis and the deep head of flexor pollicis brevis in the thenar eminence. Additionally, the ulnar nerve innervates the interossei, the third and fourth lumbricals, the abductor digiti minimi, opponens digiti minimi, and flexor digiti minimi in the hypothenar eminence.
The ulnar nerve relays sensory information back to the central nervous system in the hand from the ulnar border of the ring finger, the small finger, and spanning the dorsal and volar aspect of the hypothenar region of the hand.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Ulnar nerve entrapment occurs most commonly in the cubital tunnel or the ulnar tunnel, i.e., Guyon's canal. At the cubital tunnel, compression between Osborne's ligament, defined as the fascia connecting the two heads of the FCU superficially and the MCL of the elbow deep, can lead to symptoms of compressive neuropathy in the forearm and hand.[3]
In the ulnar tunnel or Guyon's canal, the zone of compression determines the physical presentation. Compression in zone 1 at the proximal end of Guyon's canal will result in a mixed motor and sensory deficit and is most likely caused by ganglia or hook of the hamate fractures. Compression in zone 2 after the bifurcation and surrounding the deep motor branch will cause an isolated motor deficit of the ulnar nerve, and as in the case of zone 1 pathology, is also most likely caused by ganglia or hook of the hamate fractures. Compression in zone 3 surrounding the superficial sensory branch of the ulnar nerve will result in an isolated sensory deficit in the distribution of the ulnar nerve in the hand and is most likely caused by an ulnar artery thrombosis or aneurysm.[4]
Epidemiology
A general population study in Italy revealed that men are affected at twice the rate of women for compressive neuropathies at the elbow.[5]
History and Physical
Symptoms of ulnar nerve compression have an insidious onset that typically begins with numbness and paresthesias over the small finger, ulnar half of the ring finger, and hypothenar eminence. Weakness and atrophy of the hand intrinsics may follow if compression occurs proximal to zone 3 of Guyon's canal. Wasting and atrophy of the hand often follows, and leads to clumsiness and decreased pinch strength exhibited by Froment's test positivity. Froment's test is a component of the physical examination where a patient is asked to hold a piece of paper between the thumb and radial side of the index finger to isolate adductor pollicis, which as noted above is the only muscle of the thenar eminence that is solely innervated by the ulnar nerve. Flexion of the thumb at the IP joint to utilize flexor pollicis longus (FPL) rather than the adductor pollicis indicates dysfunction of the ulnar nerve and constitutes a positive Froment's sign.[6]
Similarly, Tinel's sign at the cubital and ulnar tunnels may reproduce symptoms of paresthesias and numbness, indicating a likely compressive neuropathy at that location.
Wartenberg's sign is a test for ulnar nerve motor weakness where a patient is asked to hold his or her fingers fully adducted with the metacarpophalangeal joint, proximal interphalangeal, and distal interphalangeal joints (i.e., MCP, PIP, and DIPs) in full extension. If in so doing, it is found that the small finger drifts away from the others into abduction, this is known as a positive Wartenberg sign. This finding represents a deficiency of the palmar interossei, which are innervated by the ulnar nerve and function to adduct the fingers. An abducted drift of the little finger is caused by unopposed action from the extensor digit minimi (EDM) and the extensor digitorum communis (EDC) muscles to the small finger, which are innervated by the posterior interosseus nerve (PIN).[7]
As noted above, it is critical to understand the different areas and presentations of ulnar nerve dysfunction, and a good physical exam must differentiate between the various sites of compression. For example, a patient who has an isolated motor deficit with no sensory deficit raises suspicion of compression within zone 2 of Guyon's canal, while an isolated sensory deficit may be indicative of a zone 3 compression, or alternatively an early compressive neuropathy more proximally. Reproduction of symptoms with flexion of the elbow raises a strong suspicion of compression at the level of the elbow in the cubital tunnel. It is important to inquire if the patient notices a "snapping" or "popping" in the elbow, which indicates nerve mobility within the cubital tunnel and indicates ulnar nerve transposition may be appropriate management.
Lastly, the examiner must consider alternative diagnoses, including C8 radiculopathy. The sensory deficits associated with C8 radiculopathy and peripheral nerve compressive neuropathy are similar and must be distinguished. By understanding the anatomy, differentiation of these two mimicking clinical pictures becomes much simpler. The medial forearm receives its sensory innervation from the medial antebrachial cutaneous nerve and rises from the medial cord of the brachial plexus. Therefore, neurological changes in the medial forearm rather than isolation to the hand are consistent with C8 radiculopathy rather than an ulnar nerve compression more distally at the elbow. Muscles of the thenar eminence, including abductor pollicis brevis (APB), flexor pollicis brevis (FPB), and opponens pollicis (OP), as well as the radial two lumbricals, are innervated by the C8 nerve root through the median nerve, and would be weak in C8 radiculopathy but not in a peripheral ulnar nerve compressive neuropathy.[8]
Evaluation
X-rays of the affected extremity at the elbow and wrist should be obtained to rule out any osseous deformity that may cause nerve entrapment, as well as cervical spine radiographs that may reveal sources of radiculopathy or first rib involvement. Finally, a chest x-ray should be obtained to rule out compression of the medial chord by an apical lung or Pancoast tumor, particularly in a patient with a positive history for smoking.
X-rays of the elbow may reveal congenital abnormalities, post-traumatic changes, or valgus alignment of the elbow that can result in neuropraxia at the elbow. X-rays of the wrist should include carpal tunnel and oblique views to assess for hamate fractures, which is a common cause of ulnar nerve compression symptoms in the hand. If there is high clinical suspicion for a hook of the hamate fracture, a CT scan can better assess for pathology, as x-ray has a low sensitivity for detecting such fractures.
MRI is an imaging modality that can be further used to confirm clinical suspicions of cervical radiculopathy in the neck, or of a ganglion or other space-occupying lesions in the wrist.
Ultrasound of the nerve at the elbow and wrist can be used to measure the size of the ulnar nerve compared to controls, as well as to identify a thrombosis of the ulnar artery that can lead to ulnar nerve symptoms originating in Guyon's canal.[9]
Electromyography is also commonly used in the diagnosis of compression neuropathy with muscle denervation. Compressive neuropathies result in increased distal latency and decreased conduction velocity. Thus in patients with cubital tunnel syndrome, one is likely to identify a slowing of conduction in the ulnar nerve segment crossing the elbow.[9][10]
Treatment / Management
Initial treatment for patients with ulnar neuropathies that lack atrophy should include nonsurgical modalities such as anti-inflammatory medications, external padding of the nerve, and night splinting with the elbow in 45 degrees of flexion, or of the wrist in neutral position depending on the etiology of the compression. Additionally, occupational therapy that educates on appropriate positioning of the extremity may help to alleviate symptoms.[9][11]
Cubital Tunnel Syndrome Surgical Management
For patients with significant atrophy and weakness, or those who have failed, conservative nonsurgical treatment should consider surgical management. Surgical release of Osborne's ligament, which spans the heads of FCU, can release pressure on the nerve at the elbow. The release can be extended proximally through the medial intermuscular septum and distally through the flexor-pronator aponeurosis to allow for free movement of the nerve. Ulnar nerve transposition may also serve to relieve the traction and compression of the ulnar nerve when placing the nerve superficial to the flexor-pronator origin, which positions the nerve anterior to the axis of the elbow motion.[12][13]
Alternative treatments of cubital tunnel syndrome may include a medial epicondylectomy, which has a lower incidence of ulnar nerve injury compared to transposition but has the disadvantage of an increased risk of elbow instability and flexor-pronator weakness.[14][15][16]
Ulnar Tunnel Syndrome Surgical Management
Surgical management of compression at Guyon's canal should address the specific pathology causing the nerve compression. Ganglia and other local masses should be excised when possible and results in favorable patient outcomes. Typical release of Guyon's canal should include all four compartments spanning from proximal to the wrist flexion crease and extending to the mid-palmar line. It is important, however, to note that an isolated loss of motor function indicates a zone 2 compression, and therefore should only be managed with release of the pisohamate ligament and exploration for a deep ganglion cyst.[9][17]
Differential Diagnosis
C8-T1 radiculopathies are relatively rare in comparison to peripheral ulnar nerve compression syndromes, and given that it has a similar presentation to peripheral ulnar nerve compression, the condition is frequently overlooked by diagnosticians.[9][18] Ultimately, a thorough understanding of the anatomy of the ulnar nerve is paramount to arriving at an accurate diagnosis. Therefore, a thorough physical examination that includes both a motor and sensory examination, along with appropriate diagnostic studies such as electromyography and MRI imaging, is critical to achieving the proper diagnosis.
The ulnar nerve provides innervation to much of the hand, including the muscles of the hypothenar eminence, the palmar and dorsal interossei, the third and fourth lumbricals, and a portion of the thenar eminence including adductor pollicis and the deep head of the flexor pollicis brevis (FPB). The median nerve alternatively enters the hand through the carpal tunnel. It innervates the remainder of the thenar eminence, including the abductor pollicis, opponens pollicis, and the remainder of the flexor pollicis brevis (FPB), as well as the first and second lumbricals. In a purely isolated ulnar nerve compressive neuropathy, these five muscles would theoretically remain unaffected, while C8-T1 radiculopathy often does manifest in weakness of these muscles via the median nerve.[8]
In most patients, the ulnar nerve provides sensation to the ulnar half of the fourth finger, the small finger, and the hypothenar region of the hand on both the palmar and dorsal side. However, the ulnar nerve does not provide sensation to the medial forearm. Instead, sensation to the medial forearm is provided by the medial antebrachial cutaneous nerve, which arises from the medial cord of the brachial plexus. Therefore sensory deficits in the medial forearm should prompt evaluation for radiculopathy or Pancoast tumors that may compress the brachial plexus. Intact sensation to the medial forearm should alternatively prompt a search for a more peripheral ulnar nerve compressive syndrome.[8]
Prognosis
A review of 50 published reports of ulnar nerve compression suggests that patients with a minimal degree of compression can have an excellent outcome 50% of the time with non-operative techniques such as anti-inflammatories, external padding, and positional modification. Surgical intervention results in nearly 100% relief of symptoms, provided the location of nerve compression is properly identified and released with anterior transposition of the nerve where appropriate.[19][9]
Complications
Symptom recurrence after surgery is typically the result of either incomplete decompression of the nerve or perineural scarring.[20] The surgical approach to the cubital tunnel also places several structures at risk. Damage to the medial antebrachial cutaneous nerve can result in hyperesthesia and hyperalgesia in the medial forearm. Reports of damage to the medial collateral ligament of the elbow is also a known complication of transposition, which can lead to chronic elbow instability.[9] Surgeons should similarly take great care during surgical release of the ulnar tunnel. It is possible to damage the ulnar artery, which lies anterior and radial to the ulnar nerve, or the carpal ligaments, leading to instability in the wrist.
Postoperative and Rehabilitation Care
Early mobilization is recommended after the release of the ulnar nerve at the elbow to prevent adhesions and stiffness in the elbow.[9]
Deterrence and Patient Education
Recurrent numbness, weakness, and/or pain in the little and ring fingers may have one of many causes, and further workup by a trained orthopedic physician can help to elucidate the source of the symptoms and all available treatment options. As noted, outcomes are generally good in over half of patients undergoing nonsurgical treatment; however, when surgical management becomes an option, the location of the lesion and its decompression by a well-trained surgeon is paramount to an optimal outcome.
Enhancing Healthcare Team Outcomes
The diagnosis and appropriate treatment of ulnar nerve entrapment require that all members of the healthcare team have a basic level of understanding of the pathology of the entrapment, as well as their role in the management of the patient's symptoms. Primary care physicians and mid-level practitioners are often the first steps in the diagnosis of ulnar nerve entrapment syndromes. A basic understanding of the anatomy of the upper extremity is paramount to provide initial counsel to patients with symptoms of nerve entrapment, as well as to direct them to the appropriate provider for further management. Occupational therapists can be utilized to counsel patients on appropriate positional or padding techniques to alleviate symptoms. Neurologists are employed to perform electromyography studies, and can also be invaluable in the diagnostic process of determining the location of nerve compression. If the patient is a surgical candidate, it is paramount that the surgeon has a clear understanding of the patient's anatomy, and that his or her surgical staff is informed and aware of the surgical plan.
A review of 50 published reports of more than 2000 patients by Dellon et al. reveals that nonoperative management yields excellent results for half of the patients with mild symptoms, and surgical management with decompression and transposition yields excellent results in almost 100% of cases.[9] [Level 1]
Media
References
Polatsch DB, Melone CP Jr, Beldner S, Incorvaia A. Ulnar nerve anatomy. Hand clinics. 2007 Aug:23(3):283-9, v [PubMed PMID: 17765580]
Maroukis BL, Ogawa T, Rehim SA, Chung KC. Guyon canal: the evolution of clinical anatomy. The Journal of hand surgery. 2015 Mar:40(3):560-5. doi: 10.1016/j.jhsa.2014.09.026. Epub 2014 Oct 29 [PubMed PMID: 25446410]
Spies CK, Löw S, Langer MF, Hohendorff B, Müller LP, Unglaub F. [Cubital tunnel syndrome : Diagnostics and therapy]. Der Orthopade. 2017 Aug:46(8):717-726. doi: 10.1007/s00132-017-3453-z. Epub [PubMed PMID: 28741034]
Depukat P, Mizia E, Kuniewicz M, Bonczar T, Mazur M, Pełka P, Mróz I, Lipski M, Tomaszewski K. Syndrome of canal of Guyon - definition, diagnosis, treatment and complication. Folia medica Cracoviensia. 2015:55(1):17-23 [PubMed PMID: 26774628]
Mondelli M, Giannini F, Ballerini M, Ginanneschi F, Martorelli E. Incidence of ulnar neuropathy at the elbow in the province of Siena (Italy). Journal of the neurological sciences. 2005 Jul 15:234(1-2):5-10 [PubMed PMID: 15993135]
Level 2 (mid-level) evidenceFroment J. Prehension and the sign of the thumb in paralysis of the ulnar nerve. Bulletin of the Hospital for Joint Diseases. 1972 Oct:33(2):193-6 [PubMed PMID: 4648258]
Bertelli JA, Tavares KE. Little finger abduction and adduction testing in ulnar nerve lesions. Hand surgery & rehabilitation. 2018 Dec:37(6):368-371. doi: 10.1016/j.hansur.2018.09.006. Epub 2018 Oct 23 [PubMed PMID: 30361046]
Stoker GE, Kim HJ, Riew KD. Differentiating c8-t1 radiculopathy from ulnar neuropathy: a survey of 24 spine surgeons. Global spine journal. 2014 Feb:4(1):1-6. doi: 10.1055/s-0033-1354254. Epub 2013 Aug 28 [PubMed PMID: 24494175]
Level 3 (low-level) evidenceElhassan B, Steinmann SP. Entrapment neuropathy of the ulnar nerve. The Journal of the American Academy of Orthopaedic Surgeons. 2007 Nov:15(11):672-81 [PubMed PMID: 17989418]
Bradshaw DY, Shefner JM. Ulnar neuropathy at the elbow. Neurologic clinics. 1999 Aug:17(3):447-61, v-vi [PubMed PMID: 10393748]
Spinner M. Management of nerve compression lesions. Instructional course lectures. 1984:33():498-512 [PubMed PMID: 6546125]
Eaton RG, Crowe JF, Parkes JC 3rd. Anterior transposition of the ulnar nerve using a non-compressing fasciodermal sling. The Journal of bone and joint surgery. American volume. 1980 Jul:62(5):820-5 [PubMed PMID: 6248560]
Goldberg J, Burnham JM, Dhawan V. Subcutaneous Ulnar Nerve Transposition Using Osborne's Ligament as a Ligamentodermal or Ligamentofascial Sling. American journal of orthopedics (Belle Mead, N.J.). 2018 Sep:47(9):. doi: 10.12788/ajo.2018.0070. Epub [PubMed PMID: 30296318]
KING T, MORGAN FP. Late results of removing the medial humeral epicondyle for traumatic ulnar neuritis. The Journal of bone and joint surgery. British volume. 1959 Feb:41-B(1):51-5 [PubMed PMID: 13620706]
Craven PR Jr, Green DP. Cubital tunnel syndrome. Treatment by medial epicondylectomy. The Journal of bone and joint surgery. American volume. 1980 Sep:62(6):986-9 [PubMed PMID: 7430188]
Heithoff SJ, Millender LH, Nalebuff EA, Petruska AJ Jr. Medial epicondylectomy for the treatment of ulnar nerve compression at the elbow. The Journal of hand surgery. 1990 Jan:15(1):22-9 [PubMed PMID: 2299163]
Bednar MS. Ulnar tunnel syndrome. Hand clinics. 1996 Nov:12(4):657-64 [PubMed PMID: 8953286]
Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain : a journal of neurology. 1994 Apr:117 ( Pt 2)():325-35 [PubMed PMID: 8186959]
Dellon AL. Diagnosis and treatment of ulnar nerve compression at the elbow. Techniques in hand & upper extremity surgery. 2000 Jun:4(2):127-36 [PubMed PMID: 16609402]
Rogers MR, Bergfield TG, Aulicino PL. The failed ulnar nerve transposition. Etiology and treatment. Clinical orthopaedics and related research. 1991 Aug:(269):193-200 [PubMed PMID: 1864038]