Introduction
Varicose veins are characterized by subcutaneous dilated, tortuous veins greater than or equal to three millimeters, involving the saphenous veins, saphenous tributaries, or non-saphenous superficial leg veins with age and family history considered important risk factors.[1] Varicose veins are considered a common clinical manifestation of chronic venous disease.[2] Notwithstanding the cosmetic challenges with varicose veins, the associated superficial axial venous reflux should be evaluated. Accordingly, great and small saphenous vein reflux exclusion is part of the primary diagnostic management.[3] Varicose vein entity includes a vast majority of clinical and pathological manifestations, from limited leg discomfort to swelling and non-healing ulcers.[4][5][6]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The risk factors for varicose veins include female sex, multiparity, body weight, constipation, and history of venous thrombosis.[3][4][5] Prolonged standing or walking at work has been suggested to be a cause of VVs. Varicose veins are considered C2 in the clinical classification of clinical, etiologic, anatomic, and pathophysiological (CEAP) for chronic venous disorders.[3] Despite the multifactorial pathogenesis of varicose veins, the contributing genetic and environmental factors are understudied.[7]
In one of the recent studies, researchers applied machine learning to probe the potential risk factors of varicose veins in almost 500,000 individuals in the UK Biobank.[7] Consequently, a genome-wide association study of varicose veins and expression quantitative loci and pathway analysis were performed among unrelated individuals of white British descent.[8] Linkage disequilibrium score regression (LDSC), a tool to estimate single nucleotide polymorphisms (SNP) heritability, genetic correlation, and genomic inflation, was applied to a genome-wide association study (GWAS) summary data sets of the UK biobank.[9] Interestingly, height has emerged as a new potential risk factor, and several mendelian randomization analyses examined height's causal role in varicose vein development and severity.[7][10]
Recent mendelian randomization studies unveiled the positive and inverse association of genetically-predicted factors. Accordingly, it has been demonstrated that height, body mass index, smoking, and circulating iron levels were positively associated with the risk of varicose veins. However, circulating minerals, including calcium and zinc levels, showed an inverse association with varicose veins development. Several putative predictors that have been variably reported in the literature, including hypertension, age at menopause, and smoking, were not reported among the top predictors with machine learning approaches.[7] Indeed, the associations were further adjusted, and the results were against the association for genetically predicted systolic blood pressure after adjustment for height.[10] Moreover, the following genetically predicted factors were reported to have a positive association with the development of varicose veins; 1. coffee consumption, 2. circulating vitamin B12, and 3. magnesium levels.[10][11]
Some uncertain risk factors, including oral contraceptive pills use, are less likely to correlate independently.[7] Additionally, height and varicose veins were correlated in almost 16% of the reviewed patients. The correlation was stronger than the estimated correlation between the varicose vein and body mass index. Moreover, the history of DVT had the greatest genetic correlation with varicose vein disease. More than 850 new SNPs associated with varicose veins were evaluated, and 30 independent putative genetic variants were assessed. The strongest association was located on chromosome 1 in the CASZ1 gene, a well-established blood pressure locus.[7][12]
Epidemiology
Varicose veins are reported in up to 30 percent of the general population, with significantly increased rates in the older population.[13] Varicose veins are seen globally and are influenced by activity and lifestyle. Overall, varicose veins are more common in women than in men. The Framingham Study examined the presence of varicose veins every two years for a 16-year duration. Accordingly, twenty-three and thirty percent of the male and female population developed varicose veins during the mentioned follow-up. However, the presence or absence of venous reflux was not evaluated. The two-year incidence of varicose veins was 39.4 to 51.9 per 1000. The incidence was highest in women in their 40s.[12] There is an obvious racial correlation with the prevalence of varicose veins. Accordingly, the prevalence of chronic venous insufficiency and varicose veins in Asians is lower than non-Hispanic whites.[14]
Pathophysiology
A myriad of intrinsic and extrinsic factors contribute to the formation of varicose veins, including age, gender, pregnancy, obesity, height, race, diet, occupation, history of deep vein thrombosis (DVT), and genetics. The primary pathologies related to varicose veins are; 1) elevated venous pressure in the extremities and 2) defective or incompetent valves resulting in reflux and, thus, elevated venous pressure in the extremity. Whether venous hypertension and valvular incompetence occur before the irreversible alterations of venous wall development or the reverse is still inconclusive.[15] Several pathophysiological mechanisms, including hypoxia, cellular hyperplasia, and dysregulated apoptosis, might affect and change the combination of the extracellular matrix in the involved vein at the cellular level.[13]
Incompetent venous valves result in the backward transmission of the pressure gradient. The pressure gradient would be transmitted from the deep to the superficial venous system via the saphenofemoral junction (SFJ) and perforator veins. The most common site for the incompetent venous valve is the below-knee great saphenous vein.[16] Moreover, venous hypertension has been correlated with the severity of the disease.[15] Any conditions with increased intraabdominal pressure, including pregnancy and obesity in individuals with incompetent lower leg valves, might impose a higher risk for varicose veins.
A limited number of genetic disorders have been correlated with varicose veins disease. Accordingly, the correlation between Klippel-Trenaunay syndrome and varicose vein disease has been well established.[17] Moreover, mutations in FOXC2, thrombomodulin (THBD), and desmuslin (SYNM) may alter vein function and impose the risk of varicose vein development.[18]
Histopathology
In varicose vein pathology, two main index events are involved: venous hypertension and valvular incompetence. The mentioned events induce a cascade of immune cells and pro-inflammatory signaling pathways resulting in the consequent venous wall remodeling. However, the opponent's school of thought argues that the venous wall alteration is the index event. Collectively, venous arterialization, smooth muscle cell hypertrophy, and hyperplasia are the histopathological findings in varicose vein disease. Insulin receptor substrate (IRS)-4 may be involved in the mentioned changes.[19]
The mentioned insulin receptor, similar to other receptor proteins of the IRS substrate family, mediates cell signaling from the insulin receptor (IR) and insulin-like growth factor (IGF)-1 receptor (IGF-1R). Accordingly, insulin and IGF-1 regulate IRS-4 expression. The regulation occurs via the activation of IR/IGF-1R. Consequently, altered IRS-4 expression may be associated with impaired cellular growth and glucose dysmetabolism. Thus, histopathological evaluation of IRS-4 elucidated that IRS-4 overexpression could be served as a prognostic measure and a potential therapeutic target.[20]
History and Physical
The clinical-etiology-anatomy-pathophysiology (CEAP) classification system of venous reflux is used to assess the clinical severity of symptoms:
- C0 no visible or palpable signs of venous disease
- C1 telangiectasies or reticular veins
- C2 varicose veins
- C3 edema
- C4a pigmentation and eczema
- C4b lipodermatosclerosis and atrophie blanche
- C5 healed venous ulcer
- C6 active venous ulcer[3] However, as the evidence related to these aspects of venous disorders, specifically the subject of this topic, varicose veins (C2), continues to develop, the CEAP classification should be periodically analyzed and revised. Accordingly, in May 2017, the American venous forum CEAP task force introduced several changes, including Corona phlebectatica as the C4c clinical subclass and "r" for recurrent varicose veins and venous ulcers.[3] Among the most critical revisions, additional assessments of chronic vascular disease (CVD) regarding the functional status and sub-categorical anatomical involvement significantly improved the comprehensive evaluation of CVD with CEAP.[21]
Initial diagnosis is by clinical evaluation of swelling, discoloration, and skin ulcerations.
Symptoms associated with varicose veins include:
- Leg heaviness
- Itching
- Cramps
- Mild tenderness
- Skin discoloration
- Exercise intolerance
- Leg fatigue[22][14]
The physical exam may reveal visibly distended veins from the thigh to the ankle. The discoloration is usually most prominent around the ankle and calf. The Trendelenburg test is often used to assess the competency of the deep venous valves. The leg is elevated until all the superficial veins have collapsed. With the hand, the groin area is compressed to occlude the saphenofemoral junction, and the patient is asked to stand up. If the deep valves are incompetent, the leg's superficial veins will start filling up. If distal varicosity remains empty, the point of entry is most likely at the saphenofemoral junction. This patient can benefit from ligation of the saphenous vein at this junction.[23]
Evaluation
If venous reflux is suspected based on symptomatology and clinical evaluation, the practitioner should obtain a color duplex venous ultrasound exam. This study is an objective assessment of the anatomy of the veins as well as valvular function. During the ultrasound, evaluation for deep vein thrombosis should also be performed to confirm that DVT/obstruction is not contributing to the clinical scenario.[24][25]
Several Duplex sonography markers have been proposed to identify the preferred index for varicose vein grading study. Accordingly, the peak reflux velocity and reflux time in cases of varicose veins and non-varicose veins were compared. The results demonstrated that quantifying peak reflux velocity is more consistent than reflux time in cases of superficial venous reflux. Moreover, an optimal peak reflux velocity cut-off point of 27.4 cm/sec had the discriminatory power to differentiate the diseased limbs.[26]
Contrast venography is rarely done today. Pulsed-wave Doppler images of varicose veins in axial projection will demonstrate retrograde blood flow after the release of manual calf compression. In the varicose vein with reflux, the reflux can be easily quantified with an ultrasound probe angled steeply upward while imaging in axial projection.[27]
Treatment / Management
Injection Sclerotherapy
Utilizes chemical irritants to obliterate unwanted superficial veins. Sclerotherapy primarily applies to small nonaxial varicose veins with less than 6 mm diameter. For aesthetic reasons, sclerotherapy might be indicated in symptomatic and even asymptomatic varicose veins.[28] Several sclerosing agents have been introduced in the management of varicose veins. Polidocanol is widely used to manage reticular and spider veins with 1 to 3 and equal to or less than 1 mm diameter. The spider veins are treated with higher concentrations. (0.5 % versus 1 %), and the injections should be repeated in 1 to 2 weeks.[29] (B2)
Recently, the cyanoacrylate glue application has been the popular and preferred way to treat chronic venous insufficiency with varicose veins. This technique has several advantages, including the short duration of a minimally-invasive procedure lack of need for anesthesia induction.[28](B2)
Conservative Treatments
Most patients obtain adequate symptom relief using long-term graduated compression stockings, leg elevation, and oral pain medications. For compression rates, the recommended graduation is 20-30 mmHg and, in more severe cases, can be elevated to 30-40 mmHg.[30][31][32] Stockings, when worn daily, are the ideal treatment for patients who do not want surgery. They do work, but the heat and hot weather can reduce compliance.
Surgical Treatment
Traditional surgical treatment consisted of ligation and stripping the greater saphenous vein with the avulsion of tributary veins.
Surgical techniques involve ligation and/or removal of the veins; however, the method selection is based on the location, size, and extent of the venous involvement with or without venous reflux. Unilateral surgery in bilateral limb involvement is recommended to avoid the risk of post-operative limitations and intolerance.
In the case of saphenous vein stripping, complete skin exposure and meticulous hygiene concerns are respected. The lower extremity is prepared and draped circumferentially from the anterior superior iliac spine to the ankle. Since several skin markings are needed, alcohol-containing skin preparation is discouraged. In the presence of venous ulceration, skin preparation for the skin overlying the ulcer should be undertaken in the last step. The ulcers should be excluded from the sterile surgical field with drapes. According to the potential for significant blood loss during the surgery, specifically in the large tortuous veins, tourniquet application has been recommended.[33] The blood loss with a tourniquet application was up to 16 ml compared to almost 133 ml without the tourniquet.[34] Moreover, long-term complications, including nerve injury, were not reported. However, improper tourniquet application might cause further complications with bleeding due to venous hypertension or deep vein thrombosis due to prolonged stasis.[35] (A1)
Saphenous vein inversion and removal A transverse incision of up to 2 cm is made over the saphenofemoral junction, preferably marked with a Duplex scan, 3 cm peripheral to the pubic tubercle.[36] The saphenofemoral junction is identified and isolated. However, only the anteromedial and posterolateral tributaries are ligated; the abdominal wall branches are preserved. The latter is recommended to minimize varicose vein recurrence.[37] The greater end of the greater saphenous vein (GSV) is ligated adjacent to the GSV-CFV (common femoral vein ) confluence.[38] (A1)
Consequently, a retrograde vein stripper is passed caudally. Smooth passage regarding the incompetent venous valve is expected. The distal end of the vein stripper is pulled out adjacent to the patella, while the proximal end is secured in the groin. Mushroom tips are discouraged due to the potential for extensive tissue damage and bleeding. Venous marsupialization and removal would be followed consequently. The procedure is completed with the disruption of the tributary veins followed by precise hemostasis with direct pressure and groin incision closure in multiple layers. Inversion and removal are also indicated in the small saphenous varicose vein. However, potential neurovascular bundle complications during popliteal fossa dissection and sural nerve injury should be considered.
High saphenous ligation Albeit the ligation of the saphenous vein at the saphenofemoral junction is introduced, the technique is less encouraged due to the higher recurrence rate, persistent symptoms, and occurrence of distal superficial thrombophlebitis.[36][39] The High ligation of the saphenous vein is indicated for patients with proximal superficial phlebitis that creeps on the saphenofemoral junction with a contraindication to anticoagulation.(A1)
Ambulatory Phlebectomy
The procedure implies the excision and avulsion of the involved superficial vein with multiple skip incisions. Multiple options exist for managing varicose veins, including a combination of the procedure with saphenous inversion. Punctures are made with an 18 gauge needle or an 11-blade scalpel. Punctures are made adjacent to the target vein. Sequential venous sections are ligated and avulsed. Post-procedural hemorrhage is controlled with direct pressure application and limb elevation.[40]
Transilluminated Powered Phlebectomy
The technique is less commonly used compared to the other minimally-invasive procedures for venous ablation. The procedure is undertaken in three discrete steps under general or regional anesthesia with a mixture of saline, lidocaine, and epinephrine. The procedure starts with hydrodissection of the involved veins, followed by the introduction of the illumination device and vein maceration and aspiration through the second incision. The procedure relies on applying a mechanical aspirator labeled transilluminated powered phlebectomy (TIPP).[41] Transilluminated powered phlebectomy is considered a minimally-invasive procedure with fewer incisions. However, a significantly higher range of post-operative pain and hematoma of a more expensive procedure is inevitable.[42](B2)
Endovascular Management
Catheter-based endovenous ablations have been extensively used for EVTL, either via laser or radiofrequency. The procedure is preferably undertaken with local anesthetics. However, oral anxiolytics might be added for apprehensive patients. A catheter is introduced in an antegrade fashion for a few centimeters away from the saphenofemoral or saphenopopliteal junction. The catheter course within the saphenous vein is completely anesthetized. Next, the saphenous vein would be ablated by either heat energy or radiofrequency during the catheter withdrawal.[43][44](A1)
Differential Diagnosis
- Lymphedema
- Deep vein thrombosis
- Cellulitis
- Stasis dermatitis
Prognosis
There is no cure for varicose veins. Even after surgical removal, recurrences are common. Those who develop venous ulcers have the highest morbidity and a poor quality of life. Unlike the deep venous system, clots in superficial veins rarely embolize, and hence the risk of pulmonary embolism is rare. Untreated varicose veins reflect poor aesthetics, and this is the key reason why most people seek treatment.
Complications
- Venous ulcers
- Pain
- Poor cosmesis
- Deep vein thrombosis (DVT) and pulmonary embolism (PE), a Taiwanese database study, mentioned that the propensity for DVT in individuals with varicose veins compared to matched control patients without varicose veins was (6.6 versus 1.2 per 1000 person-years; hazard ratio, 5.30) and (0.48 versus 0.28 per 1000 person-years; hazard ratio, 1.73).[45] Still, further complementary studies are mandatory to confirm this claimed association and to enclose that it is not affected by confounding variables, including smoking and obesity.[8]
- Superficial thrombophlebitis might be complicated with prolonged bleeding and pain.[14]
- Superficial vein thrombosis[46]
Postoperative and Rehabilitation Care
One of the important aspects of care in varicose vein surgical management is the compression dressing application following the surgery. Notwithstanding the significance of compression therapy in the management of varicose veins, still, the recommendation is equivocal. Accordingly, in venous ulceration treatment, 40 and less than 20 mmHg pressure in peri-malleolar and below the knee are recommended.[47]
The prescription of compression stockings after surgical or laser ablation interventions for varicose vein disease is standard practice; however, the consensus regarding the necessity and preferred duration of compression therapy is lacking. [48][49]
The optimal duration of compression therapy after endo-venous laser ablation (EVLA) with a 1470-nm diode dual-ring radial fiber laser was evaluated.[50] The authors concluded that long-term compression stocking for more than two days following EVLA would not significantly change the outcomes.[50] The results were against the traditional recommendation for equal to or longer than 1-week compression therapy. However, it should be highlighted that the mentioned prospective studies reviewed the less-applicable low wavelength of 810 nm.[51]
Deterrence and Patient Education
- Graduated compression hose
- Healthy weight
- Exercise
Pearls and Other Issues
Venous reflux disease is a common condition that results in a considerable lifestyle impact due to the symptoms of leg pain and swelling, and that has the potential to cause more significant morbidity by eventual venous ulcer formation. Treatment with endovenous ablation with a period of compression therapy is usually effective in reducing the associated symptoms.
Enhancing Healthcare Team Outcomes
Varicose veins are very common and often lead to poor cosmesis and fatigue. However, most patients seek medical assistance because of poor cosmesis. Today, general and vascular surgeons perform several different types of procedures to treat varicose veins, but recurrence is a problem. More important, varicose vein surgery is considered cosmetic and not covered by most health plans, so the patient is left to pay for the entire cost. Each year, consumers spend millions of dollars on the care of varicose veins. In view of the fact that recurrences are common and that surgical procedures also have complications, prevention is critical. The primary care provider, pharmacist, and nurse are in a primary position to educate the patient on preventing varicose veins.
Most people can prevent varicose veins by wearing compression stockings, maintaining a healthy weight, and exercising. In addition, the patient should be educated that if the varicose vein is untreated, it can lead to a venous ulcer that is very difficult to cure and costs the healthcare system millions of dollars annually. Finally, when evaluating a patient with a varicose vein, suspicion of a DVT should be high, and the patient should be referred for a duplex ultrasound. Before referring any patient for surgery, the primary care provider, nurse, and pharmacist should advise the patient to change lifestyle, stop smoking, elevate the legs at bedtime and wear stockings- for those who comply; there is no need for surgery.[52][53][54] [Level 5]
Evidence-based Outcomes
Every surgical procedure has good to excellent outcomes for varicose veins, but each is associated with recurrence. For those who develop a venous ulcer, the morbidity is very high as there is no cure. It is also important to note that patients with varicose veins are also at high risk for deep vein thrombosis, which requires prolonged treatment with an anticoagulant which carries further morbidity from the side effects like bleeding. [Level 5] Hence, an interprofessional team approach to varicose veins is recommended to achieve good outcomes.[31][6][55] [Level 5]
Media
(Click Image to Enlarge)
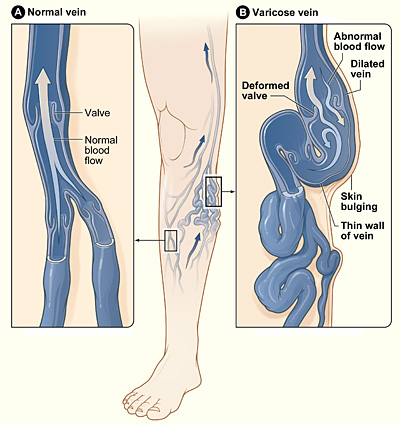
The illustration shows how a varicose vein forms in a leg. Figure A shows a normal vein with a working valve and normal blood flow. Figure B shows a varicose vein with a deformed valve, abnormal blood flow, and thin, stretched walls. The middle image shows where varicose veins might appear in a leg. Contributed by National Heart Lung and Blood Institute
References
Abou-ElWafa HS, El-Metwaly AAM, El-Gilany AH. Lower Limb Varicose Veins among Nurses: A Single Center Cross-Sectional Study in Mansoura, Egypt. Indian journal of occupational and environmental medicine. 2020 Sep-Dec:24(3):172-177. doi: 10.4103/ijoem.IJOEM_264_19. Epub 2020 Dec 14 [PubMed PMID: 33746431]
Level 2 (mid-level) evidenceHamdan A. Management of varicose veins and venous insufficiency. JAMA. 2012 Dec 26:308(24):2612-21. doi: 10.1001/jama.2012.111352. Epub [PubMed PMID: 23268520]
Lurie F, Passman M, Meisner M, Dalsing M, Masuda E, Welch H, Bush RL, Blebea J, Carpentier PH, De Maeseneer M, Gasparis A, Labropoulos N, Marston WA, Rafetto J, Santiago F, Shortell C, Uhl JF, Urbanek T, van Rij A, Eklof B, Gloviczki P, Kistner R, Lawrence P, Moneta G, Padberg F, Perrin M, Wakefield T. The 2020 update of the CEAP classification system and reporting standards. Journal of vascular surgery. Venous and lymphatic disorders. 2020 May:8(3):342-352. doi: 10.1016/j.jvsv.2019.12.075. Epub 2020 Feb 27 [PubMed PMID: 32113854]
Yang GK, Parapini M, Gagnon J, Chen JC. Comparison of cyanoacrylate embolization and radiofrequency ablation for the treatment of varicose veins. Phlebology. 2019 May:34(4):278-283. doi: 10.1177/0268355518794105. Epub 2018 Aug 16 [PubMed PMID: 30114987]
Epstein D, Onida S, Bootun R, Ortega-Ortega M, Davies AH. Cost-Effectiveness of Current and Emerging Treatments of Varicose Veins. Value in health : the journal of the International Society for Pharmacoeconomics and Outcomes Research. 2018 Aug:21(8):911-920. doi: 10.1016/j.jval.2018.01.012. Epub 2018 Mar 15 [PubMed PMID: 30098668]
Oliveira RÁ, Mazzucca ACP, Pachito DV, Riera R, Baptista-Silva JCDC. Evidence for varicose vein treatment: an overview of systematic reviews. Sao Paulo medical journal = Revista paulista de medicina. 2018 Jul-Aug:136(4):324-332. doi: 10.1590/1516-3180.2018.0003240418. Epub 2018 Jul 16 [PubMed PMID: 30020324]
Level 3 (low-level) evidenceFukaya E, Flores AM, Lindholm D, Gustafsson S, Zanetti D, Ingelsson E, Leeper NJ. Clinical and Genetic Determinants of Varicose Veins. Circulation. 2018 Dec 18:138(25):2869-2880. doi: 10.1161/CIRCULATIONAHA.118.035584. Epub [PubMed PMID: 30566020]
Li R, Chen Z, Gui L, Wu Z, Miao Y, Gao Q, Diao Y, Li Y. Varicose Veins and Risk of Venous Thromboembolic Diseases: A Two-Sample-Based Mendelian Randomization Study. Frontiers in cardiovascular medicine. 2022:9():849027. doi: 10.3389/fcvm.2022.849027. Epub 2022 Apr 14 [PubMed PMID: 35498031]
Bulik-Sullivan BK, Loh PR, Finucane HK, Ripke S, Yang J, Schizophrenia Working Group of the Psychiatric Genomics Consortium, Patterson N, Daly MJ, Price AL, Neale BM. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nature genetics. 2015 Mar:47(3):291-5. doi: 10.1038/ng.3211. Epub 2015 Feb 2 [PubMed PMID: 25642630]
Yuan S, Bruzelius M, Damrauer SM, Larsson SC. Cardiometabolic, Lifestyle, and Nutritional Factors in Relation to Varicose Veins: A Mendelian Randomization Study. Journal of the American Heart Association. 2021 Nov 2:10(21):e022286. doi: 10.1161/JAHA.121.022286. Epub 2021 Oct 20 [PubMed PMID: 34666504]
Larsson SC, Burgess S. Appraising the causal role of smoking in multiple diseases: A systematic review and meta-analysis of Mendelian randomization studies. EBioMedicine. 2022 Aug:82():104154. doi: 10.1016/j.ebiom.2022.104154. Epub 2022 Jul 8 [PubMed PMID: 35816897]
Level 1 (high-level) evidenceAhmed WU, Kleeman S, Ng M, Wang W, Auton A, 23andMe Research Team, Lee R, Handa A, Zondervan KT, Wiberg A, Furniss D. Genome-wide association analysis and replication in 810,625 individuals with varicose veins. Nature communications. 2022 Jun 2:13(1):3065. doi: 10.1038/s41467-022-30765-y. Epub 2022 Jun 2 [PubMed PMID: 35654884]
Shadrina AS, Elgaeva EE, Stanaway IB, Jarvik GP, Namjou B, Wei WQ, Glessner J, Hakonarson H, Suri P, Tsepilov YA. Mendelian randomization analysis of plasma levels of CD209 and MICB proteins and the risk of varicose veins of lower extremities. PloS one. 2022:17(5):e0268725. doi: 10.1371/journal.pone.0268725. Epub 2022 May 20 [PubMed PMID: 35594287]
Youn YJ, Lee J. Chronic venous insufficiency and varicose veins of the lower extremities. The Korean journal of internal medicine. 2019 Mar:34(2):269-283. doi: 10.3904/kjim.2018.230. Epub 2018 Oct 26 [PubMed PMID: 30360023]
Jacobs BN, Andraska EA, Obi AT, Wakefield TW. Pathophysiology of varicose veins. Journal of vascular surgery. Venous and lymphatic disorders. 2017 May:5(3):460-467. doi: 10.1016/j.jvsv.2016.12.014. Epub [PubMed PMID: 28411716]
Pagano M, Bissacco D, Flore R, Tondi P. Great saphenous vein reflux treatment in patients with femoral valve incompetence, the Excluded Saphenous Vein Technique (ESVT): a pilot study. European review for medical and pharmacological sciences. 2018 Nov:22(21):7453-7457. doi: 10.26355/eurrev_201811_16286. Epub [PubMed PMID: 30468494]
Level 3 (low-level) evidenceAnwar MA, Georgiadis KA, Shalhoub J, Lim CS, Gohel MS, Davies AH. A review of familial, genetic, and congenital aspects of primary varicose vein disease. Circulation. Cardiovascular genetics. 2012 Aug 1:5(4):460-6. doi: 10.1161/CIRCGENETICS.112.963439. Epub [PubMed PMID: 22896013]
Level 1 (high-level) evidenceJones GT, Marsman J, Pardo LM, Nijsten T, De Maeseneer M, Phillips V, Lynch-Sutherland C, Horsfield J, Krysa J, van Rij AM. A variant of the castor zinc finger 1 (CASZ1) gene is differentially associated with the clinical classification of chronic venous disease. Scientific reports. 2019 Sep 30:9(1):14011. doi: 10.1038/s41598-019-50586-2. Epub 2019 Sep 30 [PubMed PMID: 31570750]
Horecka A, Hordyjewska A, Biernacka J, Dąbrowski W, Zubilewicz T, Malec A, Musik I, Kurzepa J. Intense remodeling of extracellular matrix within the varicose vein: the role of gelatinases and vascular endothelial growth factor. Irish journal of medical science. 2021 Feb:190(1):255-259. doi: 10.1007/s11845-020-02289-1. Epub 2020 Jun 27 [PubMed PMID: 32594304]
Ortega MA, Fraile-Martínez O, García-Montero C, Ruiz-Grande F, Barrena S, Montoya H, Pekarek L, Zoullas S, Alvarez-Mon MA, Sainz F, Asúnsolo A, Acero J, Álvarez-Mon M, Buján J, García-Honduvilla N, Guijarro LG. Chronic venous disease patients show increased IRS-4 expression in the great saphenous vein wall. The Journal of international medical research. 2021 Sep:49(9):3000605211041275. doi: 10.1177/03000605211041275. Epub [PubMed PMID: 34590920]
Zalewski DP, Ruszel KP, Stępniewski A, Gałkowski D, Feldo M, Kocki J, Bogucka-Kocka A. miRNA Regulatory Networks Associated with Peripheral Vascular Diseases. Journal of clinical medicine. 2022 Jun 16:11(12):. doi: 10.3390/jcm11123470. Epub 2022 Jun 16 [PubMed PMID: 35743538]
Yetkin E, Kutlu Karadag M, Ileri M, Atak R, Erdil N, Tekin G, Ozyasar M, Ozturk S. Venous leg symptoms, ecchymosis, and coldness in patients with peripheral varicose vein: A multicenter assessment and validation study (VEIN-VIOLET study). Vascular. 2021 Oct:29(5):767-775. doi: 10.1177/1708538120980207. Epub 2020 Dec 18 [PubMed PMID: 33334264]
Level 1 (high-level) evidenceLattimer CR, Mendoza E. Reappraisal of the Utility of the Tilt-table in the Investigation of Venous Disease(†). European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2016 Dec:52(6):854-861. doi: 10.1016/j.ejvs.2016.09.012. Epub 2016 Oct 24 [PubMed PMID: 27789144]
Tolu I, Durmaz MS. Frequency and Significance of Perforating Venous Insufficiency in Patients with Chronic Venous Insufficiency of Lower Extremity. The Eurasian journal of medicine. 2018 Jun:50(2):99-104. doi: 10.5152/eurasianjmed.2018.18338. Epub 2018 Apr 30 [PubMed PMID: 30002576]
Nybo J, Nybo M, Hvas AM. [Diagnostic work-up and treatment of superficial vein thrombosis]. Ugeskrift for laeger. 2018 Aug 13:180(33):. pii: V01180014. Epub [PubMed PMID: 30084349]
Singh AK, Karmacharya RM, Vaidya S, Thapa P. Quantification of Superficial Venous Reflux by Duplex Ultrasound - Role of Peak Reflux Velocity and Reflux Time in the Assessment of Varicose Vein. Journal of Nepal Health Research Council. 2020 Nov 14:18(3):442-447. doi: 10.33314/jnhrc.v18i3.2558. Epub 2020 Nov 14 [PubMed PMID: 33210638]
Khilnani NM. Duplex ultrasound evaluation of patients with chronic venous disease of the lower extremities. AJR. American journal of roentgenology. 2014 Mar:202(3):633-42. doi: 10.2214/AJR.13.11465. Epub [PubMed PMID: 24555602]
Demirtaş H, Dolu İ. The prevalence of poor sleep quality and its association with the risk of obstructive sleep apnea and restless legs syndrome in diabetic patients treated with cyanoacrylate glue for varicose veins. Sleep & breathing = Schlaf & Atmung. 2023 May:27(2):745-755. doi: 10.1007/s11325-022-02676-1. Epub 2022 Jul 1 [PubMed PMID: 35776370]
Level 2 (mid-level) evidenceLi J, Wu C, Song D, Wang L, Guo L. Polidocanol Sclerotherapy for the Treatment of Pyogenic Granuloma in Children. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2021 Jun 1:47(6):802-804. doi: 10.1097/DSS.0000000000002967. Epub [PubMed PMID: 33625133]
Davies HOB, Popplewell M, Bate G, Ryan RP, Marshall TP, Bradbury AW. Analysis of Effect of National Institute for Health and Care Excellence Clinical Guideline CG168 on Management of Varicose Veins in Primary Care Using the Health Improvement Network Database. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2018 Dec:56(6):880-884. doi: 10.1016/j.ejvs.2018.07.023. Epub 2018 Aug 24 [PubMed PMID: 30150075]
Wallace T, El-Sheikha J, Nandhra S, Leung C, Mohamed A, Harwood A, Smith G, Carradice D, Chetter I. Long-term outcomes of endovenous laser ablation and conventional surgery for great saphenous varicose veins. The British journal of surgery. 2018 Dec:105(13):1759-1767. doi: 10.1002/bjs.10961. Epub 2018 Aug 22 [PubMed PMID: 30132797]
Kemp N. A synopsis of current international guidelines and new modalities for the treatment of varicose veins. Australian family physician. 2017:46(4):229-233 [PubMed PMID: 28376578]
Rigby KA, Palfreyman SJ, Beverley C, Michaels JA. Surgery for varicose veins: use of tourniquet. The Cochrane database of systematic reviews. 2013 Jun 10:2013(6):CD001486. doi: 10.1002/14651858.CD001486.pub2. Epub 2013 Jun 10 [PubMed PMID: 23749738]
Level 1 (high-level) evidenceWu H, Chen LX, Li YL, Wu Q, Wu QL, Ning GZ, Feng SQ. Tourniquet used in anterior cruciate ligament reconstruction: a system review. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2014 Aug:24(6):999-1003. doi: 10.1007/s00590-013-1351-6. Epub 2013 Nov 13 [PubMed PMID: 24220745]
Chen K, Yu GF, Huang JY, Huang LD, Su X, Ni HZ, Pan LM, Zheng XT. Incidence and risk factors of early deep venous thrombosis after varicose vein surgery with routine use of a tourniquet. Thrombosis research. 2015 Jun:135(6):1052-6. doi: 10.1016/j.thromres.2015.03.008. Epub 2015 Mar 9 [PubMed PMID: 25921935]
Casoni P, Lefebvre-Vilardebo M, Villa F, Corona P. Great saphenous vein surgery without high ligation of the saphenofemoral junction. Journal of vascular surgery. 2013 Jul:58(1):173-8. doi: 10.1016/j.jvs.2012.11.116. Epub 2013 May 22 [PubMed PMID: 23706654]
Level 1 (high-level) evidenceGuarinello GG, Coral FE, Timi JRR, Machado SF. Assessment of residual stumps 12 months after saphenectomy without high ligation of the saphenofemoral junction. Jornal vascular brasileiro. 2021:20():e20210029. doi: 10.1590/1677-5449.210029. Epub 2021 Jul 5 [PubMed PMID: 34267791]
Recek C. Significance of Reflux Abolition at the Saphenofemoral Junction in Connection with Stripping and Ablative Methods. The International journal of angiology : official publication of the International College of Angiology, Inc. 2015 Dec:24(4):249-61. doi: 10.1055/s-0035-1546439. Epub 2015 Mar 23 [PubMed PMID: 26648666]
Kusagawa H,Ozu Y,Inoue K,Komada T,Katayama Y, Clinical Results 5 Years after Great Saphenous Vein Stripping. Annals of vascular diseases. 2021 Jun 25 [PubMed PMID: 34239635]
Zhan HT, Bush RL. A review of the current management and treatment options for superficial venous insufficiency. World journal of surgery. 2014 Oct:38(10):2580-8. doi: 10.1007/s00268-014-2621-0. Epub [PubMed PMID: 24803347]
Chen S, Zeng Q, Fu Q, Li F, Zhang M, Zhao Y. Transilluminated powered phlebectomy in the treatment of large area venous leg ulcers: A case-control study with 3 years follow-up. Microcirculation (New York, N.Y. : 1994). 2019 Apr:26(3):e12523. doi: 10.1111/micc.12523. Epub 2019 Jan 30 [PubMed PMID: 30556350]
Level 2 (mid-level) evidenceOrhurhu V, Chu R, Xie K, Kamanyi GN, Salisu B, Salisu-Orhurhu M, Urits I, Kaye RJ, Hasoon J, Viswanath O, Kaye AJ, Karri J, Marshall Z, Kaye AD, Anahita D. Management of Lower Extremity Pain from Chronic Venous Insufficiency: A Comprehensive Review. Cardiology and therapy. 2021 Jun:10(1):111-140. doi: 10.1007/s40119-021-00213-x. Epub 2021 Mar 11 [PubMed PMID: 33704678]
Paravastu SC,Horne M,Dodd PD, Endovenous ablation therapy (laser or radiofrequency) or foam sclerotherapy versus conventional surgical repair for short saphenous varicose veins. The Cochrane database of systematic reviews. 2016 Nov 29; [PubMed PMID: 27898181]
Level 1 (high-level) evidenceNesbitt C, Bedenis R, Bhattacharya V, Stansby G. Endovenous ablation (radiofrequency and laser) and foam sclerotherapy versus open surgery for great saphenous vein varices. The Cochrane database of systematic reviews. 2014 Jul 30:(7):CD005624. doi: 10.1002/14651858.CD005624.pub3. Epub 2014 Jul 30 [PubMed PMID: 25075589]
Level 1 (high-level) evidenceChang SL, Huang YL, Lee MC, Hu S, Hsiao YC, Chang SW, Chang CJ, Chen PC. Association of Varicose Veins With Incident Venous Thromboembolism and Peripheral Artery Disease. JAMA. 2018 Feb 27:319(8):807-817. doi: 10.1001/jama.2018.0246. Epub [PubMed PMID: 29486040]
Pannucci CJ, Shanks A, Moote MJ, Bahl V, Cederna PS, Naughton NN, Wakefield TW, Henke PK, Campbell DA, Kheterpal S. Identifying patients at high risk for venous thromboembolism requiring treatment after outpatient surgery. Annals of surgery. 2012 Jun:255(6):1093-9. doi: 10.1097/SLA.0b013e3182519ccf. Epub [PubMed PMID: 22584630]
Mościcka P, Szewczyk MT, Cwajda-Białasik J, Jawień A. The role of compression therapy in the treatment of venous leg ulcers. Advances in clinical and experimental medicine : official organ Wroclaw Medical University. 2019 Jun:28(6):847-852. doi: 10.17219/acem/78768. Epub [PubMed PMID: 30085435]
Level 3 (low-level) evidenceLurie F, Lal BK, Antignani PL, Blebea J, Bush R, Caprini J, Davies A, Forrestal M, Jacobowitz G, Kalodiki E, Killewich L, Lohr J, Ma H, Mosti G, Partsch H, Rooke T, Wakefield T. Compression therapy after invasive treatment of superficial veins of the lower extremities: Clinical practice guidelines of the American Venous Forum, Society for Vascular Surgery, American College of Phlebology, Society for Vascular Medicine, and International Union of Phlebology. Journal of vascular surgery. Venous and lymphatic disorders. 2019 Jan:7(1):17-28. doi: 10.1016/j.jvsv.2018.10.002. Epub [PubMed PMID: 30554745]
Level 1 (high-level) evidenceMo M, Hirokawa M, Satokawa H, Yasugi T, Yamaki T, Ito T, Onozawa S, Kobata T, Shirasugi N, Shokoku S, Sugano N, Sugiyama S, Hoshina K, On Behalf Of Guideline Committee Japanese Society Of Phlebology, Ogawa T, On Behalf Of Japanese Commitee Of Endovenous Treatment For Varicose Veins. Supplement of Clinical Practice Guidelines for Endovenous Thermal Ablation for Varicose Veins: Overuse for the Inappropriate Indication. Annals of vascular diseases. 2021 Dec 25:14(4):323-327. doi: 10.3400/avd.ra.21-00006. Epub [PubMed PMID: 35082936]
Level 1 (high-level) evidenceMii S, Guntani A, Yoshiga R, Matsumoto T, Kawakubo E, Okadome J. Optimal Duration of Compression Stocking Therapy after Endovenous Laser Ablation Using a 1470-nm Diode Dual-Ring Radial Laser Fiber for Great Saphenous Vein Insufficiency. Annals of vascular diseases. 2021 Jun 25:14(2):122-131. doi: 10.3400/avd.oa.21-00012. Epub [PubMed PMID: 34239637]
Elderman JH, Krasznai AG, Voogd AC, Hulsewé KW, Sikkink CJ. Role of compression stockings after endovenous laser therapy for primary varicosis. Journal of vascular surgery. Venous and lymphatic disorders. 2014 Jul:2(3):289-96. doi: 10.1016/j.jvsv.2014.01.003. Epub 2014 Feb 14 [PubMed PMID: 26993388]
Caputo WJ, Kaplan MD, Kamieniecki RE, Hawkins M, Monterosa P, Eagen K, Ike T, Iannitelli A. Venous Intervention Improves Patient Outcomes. Surgical technology international. 2017 Jul 25:30():77-79 [PubMed PMID: 28693044]
Marola S, Ferrarese A, Solej M, Enrico S, Nano M, Martino V. Management of venous ulcers: State of the art. International journal of surgery (London, England). 2016 Sep:33 Suppl 1():S132-4. doi: 10.1016/j.ijsu.2016.06.015. Epub 2016 Jun 21 [PubMed PMID: 27353850]
Alavi A, Sibbald RG, Phillips TJ, Miller OF, Margolis DJ, Marston W, Woo K, Romanelli M, Kirsner RS. What's new: Management of venous leg ulcers: Approach to venous leg ulcers. Journal of the American Academy of Dermatology. 2016 Apr:74(4):627-40; quiz 641-2. doi: 10.1016/j.jaad.2014.10.048. Epub [PubMed PMID: 26979354]
Al Shakarchi J, Wall M, Newman J, Pathak R, Rehman A, Garnham A, Hobbs S. The role of compression after endovenous ablation of varicose veins. Journal of vascular surgery. Venous and lymphatic disorders. 2018 Jul:6(4):546-550. doi: 10.1016/j.jvsv.2018.01.021. Epub 2018 Apr 19 [PubMed PMID: 29680439]
