Introduction
The vertebrobasilar (VB) system, comprised of the vertebral and basilar arteries, serves as a critical arterial supply to the cervical spinal cord brainstem, cerebellum, thalamus, and occipital lobes. Disruptions of VB circulation can have devastating neurologic consequences; thus, a thorough understanding of the anatomy and clinical significance of the VB system is critical for assessing neurologic syndromes and preoperative neurosurgical planning.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
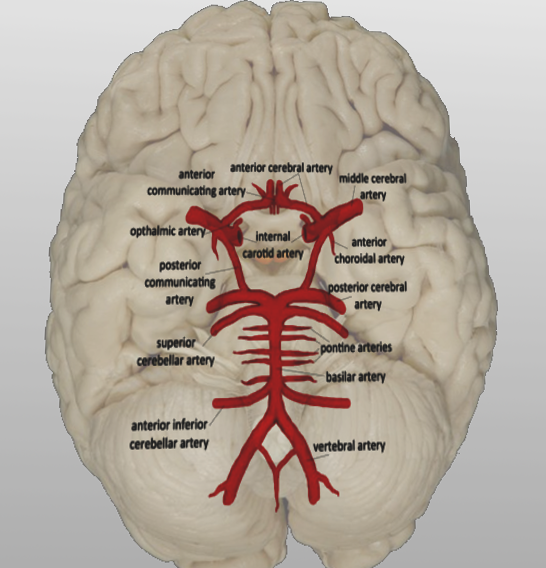
The vertebrobasilar system is comprised of bilateral vertebral arteries (VA) and an unpaired basilar artery (BA). The vertebral artery divides into four segments along its course.[1] The pre-foraminal or V1 segment arises as to the first branch of the subclavian artery, superior to the first rib,[2] and courses posteriorly between the anterior scalene and longus colli muscles. The VA then enters the transverse foramen (also known as the foramina transversarium, TF) of the sixth cervical vertebrae (C6),[3] alongside the descending vertebral venous plexus and accompanying sympathetic plexus as the foraminal or V2 segment. As the VA ascends through the cervical vertebrae, VA branches at each cervical level supply the surrounding musculature via the anterior spinal arteries. After exiting the TF of the axis, the atlanto or V3 segment of the VA courses laterally to traverse the TF of C1. The VA then travels over the posterior arch of the atlas and through the suboccipital triangle to enter the intracranial space through the foramen magnum as the intracranial, intradural, or V4 segment. Upon entering the cranium, the VA branches off the posterior inferior cerebellar artery before it unites with the contralateral VA at the base of the pons to form the BA.
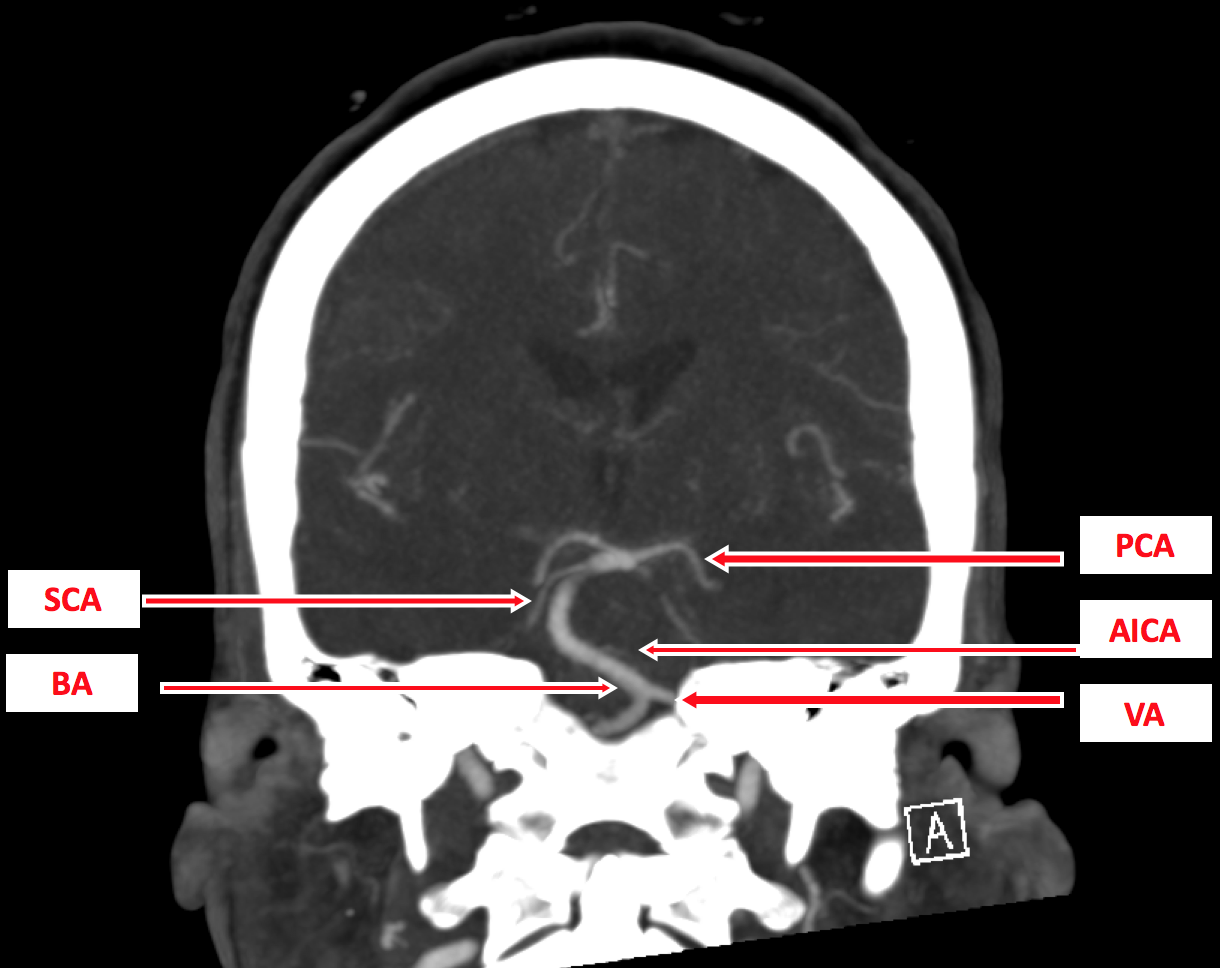
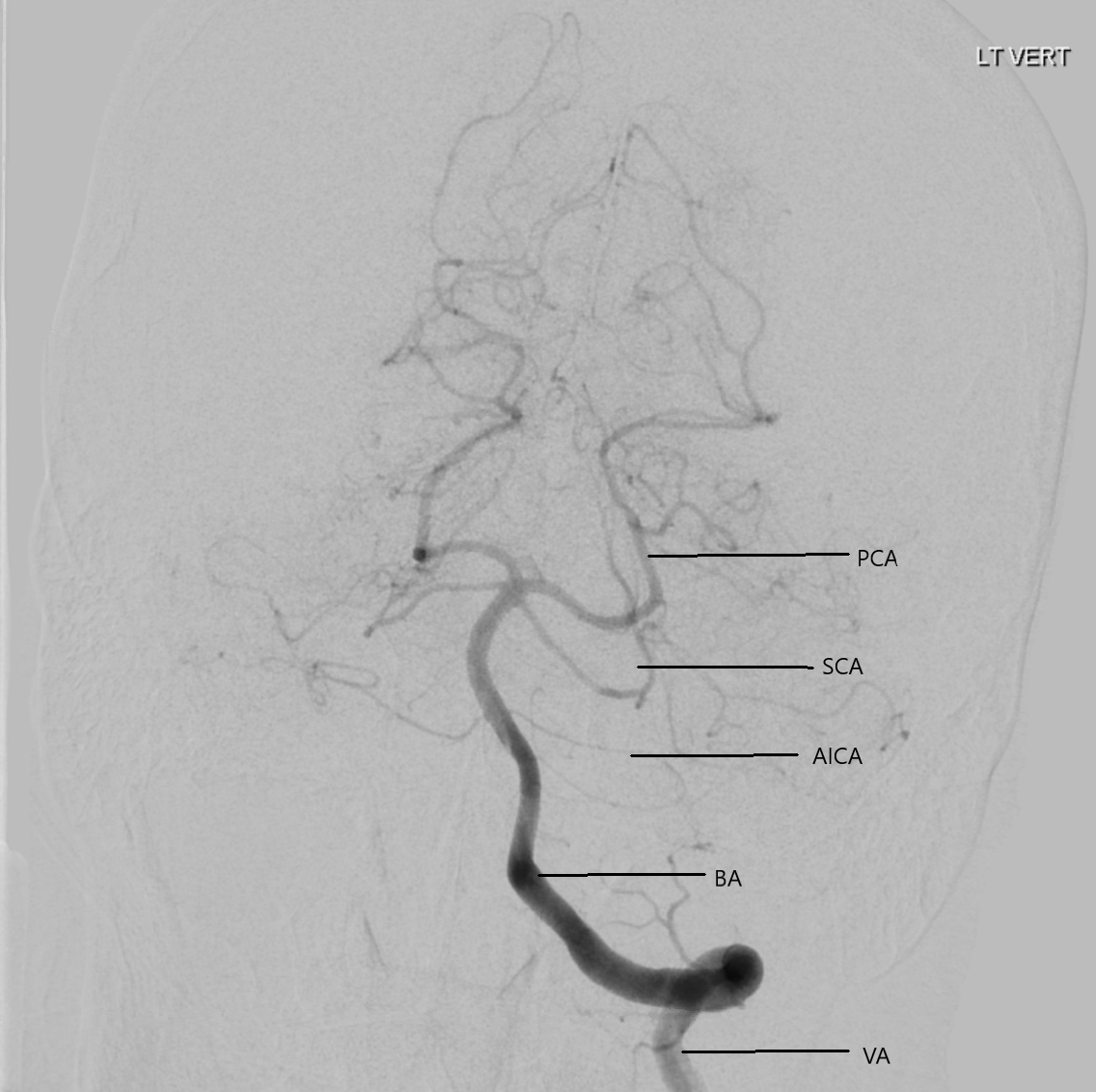
The basilar artery serves as the primary source of arterial supply to the brainstem and posterior cerebral hemispheres. The BA courses anterosuperiorly within the basilar sulcus of the pons, giving off bilateral anterior inferior cerebellar arteries, multiple paramedian perforating pontine arteries, and the paired superior cerebellar arteries. As the BA approaches the base of the pituitary gland, it divides to give rise to the bilateral posterior cerebral arteries and posterior communicating arteries to complete the circle of Willis. The connection of the BA to the circle of Willis allows for the collateral pathway of the BA to supply anterior brain structures if flow through one of the internal carotid arteries (ICA) is compromised.
Embryology
The development of the fetal cerebrovascular system begins with the development of the ICA from the third branchial arch arteries at day 24.[4] By day 28, the ICAs divide into anterior and posterior divisions, with the posterior branch giving rise to the anastomosing pro-atlantal, hypoglossal, otic, and trigeminal arteries that supply bilateral network-like longitudinal neural channels.[4] The hypoglossal, otic, and trigeminal arteries supply flow to the hindbrain for approximately one week, until the posterior communicating artery develops and connects to the BA formed by the consolidation of the paired neural channels.[4]
Between 33 and 55 days of development, the VA begins to form from anastomoses of the seven cervical intersegmental arteries, starting with the pro-atlantal artery and proceeding caudally to the sixth intersegmental artery.[2][4] The first to sixth intersegmental arteries obliterate quickly, as the seventh intersegmental artery develops into the subclavian artery and forms an anastomosis with the primitive vertebral artery to complete the posterior cerebrovascular system.[2][4]
Blood Supply and Lymphatics
The VB system provides circulation to the cervical spinal cord, cerebellum, brainstem, and posterior cerebrum via its major branches:
- Vertebral arteries
- Anterior spinal arteries supply the cervical spinal cord
- Muscular branches supply the deep cervical musculature
- Posterior inferior cerebellar arteries supply the cerebellum and the choroid plexus of the fourth ventricle
- Basilar artery
- Anterior inferior cerebellar arteries supply the inferolateral pons, anteroinferior cerebellum, and the middle cerebellar peduncle
- Paramedian arteries supply the thalamus and pons
- Superior cerebellar arteries supply the superior cerebellum and parts of the midbrain
Venous drainage from the territory supplied by the VB system is mainly via the vertebral venous plexus surrounding the vertebral arteries within the transverse foramina and the dural venous sinuses, which drain into the internal jugular veins.
Nerves
The vertebrobasilar system has an intimate relationship with many nerves along its course. The V1 segment of the vertebral artery courses anteriorly to the inferior cervical ganglion and the sympathetic trunk at the level of C7. As V2 ascends within the transverse foramina, it is surrounded by branches of the sympathetic plexus. As V3 crosses the posterior arch of C1, it passes laterally to the suboccipital nerve. After entering the cranium, V4 courses along the medulla oblongata between the anterior nerve root of C1 and the hypoglossal nerve. The basilar artery ascends along the anteroinferior surface of the pons and terminally gives off the superior cerebellar artery and posterior cerebral artery with the sixth cranial nerve traversing between them.
Physiologic Variants
While commonly arising from the subclavian arteries, the left vertebral artery may anomalously arise from the aorta in 2.4 to 5.8% of patients due to failed anastomosis between the sixth and seventh intersegmental arteries.[2] Such variants have an increased incidence of vertebral artery dissection, cerebrovascular events, and iatrogenic injury during carotid artery procedures.[5][6] Even more atypical is the vertebral arteria lusoria variant, in which the right VA arises from the aortic arch and takes a retro-esophageal course, which may be problematic during esophageal surgery.[7] Asymmetry in the size of VAs is common, with over 50% of individuals having a larger, dominant VA, most frequently on the left.[8] In approximately 10% of cases, the PICA arises from the extradural V3 segment rather than the intracranial V4 portion of the VA, most commonly in the non-dominant VA.[9] Other aberrations of the VA include dual or accessory arteries, fenestrations, kinking, tortuosity, elongation, hypoplasia, and aplasia.[2] Although most VA anomalies are asymptomatic, any variations along the course of the VA may elevate the risk of occlusion, dissection, and even add up the risk of Alzheimer disease.[1][10][11][2]
Anomalies may also arise in the TF of the cervical vertebrae. The VA most commonly enter the TF at the level of C6, although in a small percentage of individuals, the arteries delve into the TF at C4, C5, or C7, which may predispose to injury during cervical spinal surgery from an anterior approach.[3][12][13] Such anomalous entries are most commonly associated with VAs of aortic origin.[3] Partial or complete ossification of the atlantooccipital membrane covering the C1 TF, known as an arcuate foramen or Kimmerle anomaly, has an estimated prevalence of 15% and is more common among women.[14] Clinical manifestations of the arcuate foramen include neck and upper extremity pain, headache, vertigo, hearing loss, and VA dissection.[14][15][16] Duplication, triplication, and hypoplasia of the TF, as well as accessory foramen, have also been described.[17][18] 60% of patients with TF abnormalities also displayed asymmetry or variants of the corresponding VA, versus 25% of patients without TF variants.[1]
Nearly 4% of autopsy specimens display fenestrations of the BA, also known as segmental duplication.[4] The fenestration most commonly occurs proximally, near the VB junction, and is an embryological variant that typically remains unchanged throughout adulthood.[4] Other variants of the BA include persistence of the anastomosing arteries giving rise to the posterior fetal circulation, leading to persistent carotid-basilar anastomosis into adulthood.[19][4] Anomalous branches may arise from the BA. The internal auditory or labyrinthine artery typically arises from the anterior inferior cerebellar artery but may arise from the BA in 15%. Similarly, the posterior inferior cerebellar artery arises from the BA in 10%, rather than from the VA, to supply the structures of the inner ear.[19]
Surgical Considerations
Although injury to the vertebral arteries is an uncommon complication of spinal surgery, particular care must be taken to avoid disturbing the vertebrobasilar system, as bleeding may be profuse and uncontrollable.[20][21] Such injury leads to permanent neurologic injury or death in 10% of cases.[21][22] Tamponade is often sufficient to control bleed, though endovascular embolization may be necessary for the management of pseudoaneurysms.[20] Given the relatively high prevalence of VA variants, preoperative imaging with computed tomography angiography is recommended whenever a variant artery is suspected or in case of the traumatic cervical spine subluxations.[1]
For the surgical management of symptomatic intracranial VB stenosis secondary to atherosclerosis, patients may undergo intracranial angioplasty with or without stent placement.[23][24][25] Such a procedure carries an annual stroke rate of 3.2% in the treated territory and 4.4% overall.[23] Surgical approaches for the management of extracranial VB stenosis include VA endarterectomy, VA transection distal to the stenosis and reimplantation, and vein patch angioplasty.[26] Complications of surgical revascularization include thrombosis, Horner syndrome, recurrent laryngeal nerve palsy, and chylothorax.[26]
Clinical Significance
One of the direst neurologic presentations, locked-in syndrome, is resultant from thrombosis of the proximal and middle portions of the BA, sparing the pontine tegmentum.[19] Clinical manifestations of the locked-in syndrome include nearly complete paralysis of all voluntary muscles, except for blinking and vertical eye movements, with preserved consciousness and cognitive function. Alternatively, distal BA embolism may present with the top-of-the-basilar syndrome, resulting in the upper brainstem and thalamic ischemia.[19][27] Features of the top-of-the-basilar syndrome include oculomotor and pupillary disturbances, visual hallucinations, and alterations in consciousness.[27]
Transient partial ischemia of the posterior circulation due to decreased VB blood flow is known as VB insufficiency and may be classified as a transient ischemic attack if symptoms resolve within 24 hours. Vertigo is often the only symptom of VB insufficiency, although patients may also develop diplopia or suffer from drop attacks (sudden fall without a loss of consciousness).[28] VB insufficiency most commonly results from atherosclerosis; risk factors include age, male sex, hypertension, hyperlipidemia, and smoking.[28] Episodes may be provoked by a rapid decrease in blood pressure, such as postural changes, or increased blood flow to the lower body, such as exercise, cycling, or climbing stairs.
Vertebral artery dissections result from a tear in the tunica intima of the VA, leading to blood accumulation within the tunica media. The blood eventually thromboses within the arterial wall, causing the stenosis of the VA and increasing the risk of embolic stroke. Dissections may be traumatic or spontaneous, with spontaneous dissections associated with connective tissue disorders, including Ehlers-Danlos syndrome type IV and Marfan syndrome.[29] Traumatic causes include motor vehicle accidents, blows to the neck, strangulation, and chiropractic manipulation. Symptoms of VA dissections include symptoms of VB insufficiency, a dull or throbbing headache, dysarthria, dysphagia, ataxia, visual loss, and a partial Horner's syndrome. Complications include infarction of the posterior circulation and subarachnoid hemorrhage.
The subclavian steal phenomenon is resultant from the redundancy of the VB system. Proximal stenosis of the subclavian artery by atherosclerosis, a cervical rib, or Takayasu arteritis results in a high resistance path to blood flow through the subclavian artery. The low resistance distal to the occlusion leads to retrograde blood flow down the ipsilateral VA to the affected upper extremity and diminished blood supply to the posterior circulation.[30] Once stenosis exceeds 50% occlusion, over 90% of patients will experience continuous or episodic retrograde VA blood flow.[31] Although typically asymptomatic, manifestations of subclavian steal syndrome include syncope, presyncope, neurologic deficits, a blood pressure differential between arms, and unilateral arm claudication, particularly with the exertion of the affected upper extremity.[31]
Diagnostic evaluation of the VB system can be performed via several imaging modalities. Doppler ultrasonography was the initial technique used to assess the patency of the extracranial segments of the VAs, although it is unable to visualize the origin of the VAs in some patients.[2] Presently, computed tomography or magnetic resonance angiography, and digital subtraction angiography (DSA) are the diagnostic modalities of choice in the evaluation of the vertebral and basilar arteries.[32][33]
Other Issues
The hemodynamic alterations from vascular variants can predispose to aneurysm formation within the VB system. Other vascular anomalies include arteriovenous malformations (AVM), dural AV fistulas (DAVF), and sometimes persistent primitive carotid-vertebrobasilar communications. Aneurysms and AVM though less common compared to their supratentorial counterparts, the risk of rupture as well as ensuing morbidity and mortality is substantially high. Though micro-neurosurgery remains a gold standard in their management, other modalities like radiotherapy and endovascular modalities also play a pivotal role in selecting and planning a correct therapeutic algorithm in many of them.[34]
The intrasellar primitive persistent trigeminal artery can be inadvertently damaged during trans-nasal transsphenoidal endoscopic or microscopic pituitary surgery thereby leading to neurological deficits contributable to vascular compromise in territories within the distal VB system.[35]
The presence of fetal posterior communicating arteries plays a significant role while managing internal carotid artery (ICA) bifurcation, posterior communicating artery (PCOM), and basilar tip aneurysms. The fetal PCOMs should be preserved, and their patency assured to maintain normal vascularity in the posterior cerebral artery (PCA) territory.[36] There is also an utmost need to outline and preserve perforators in cases of rare variations in their origin from the PCA to prevent the artery of Percheron infarction.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
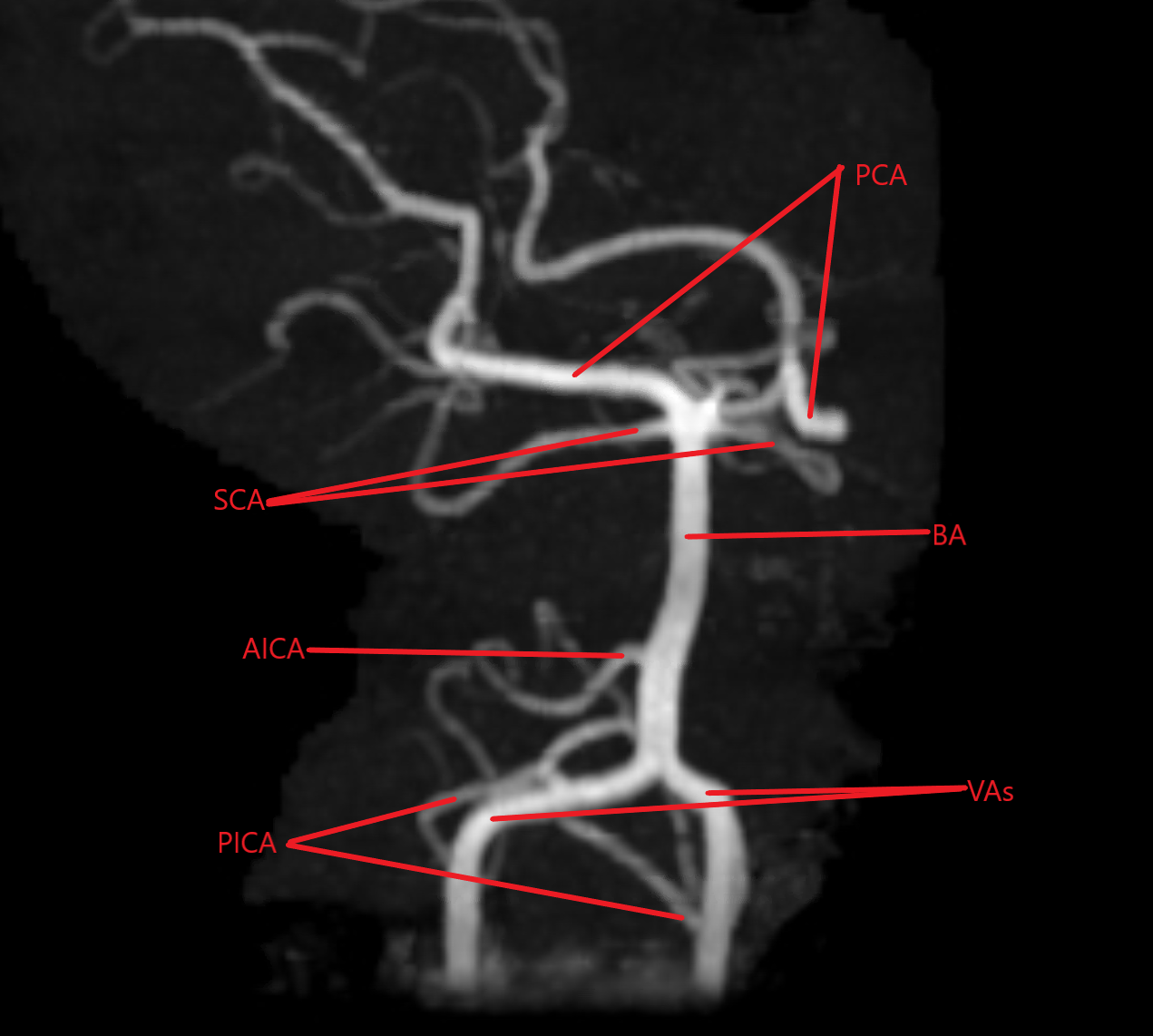
Magnetic Resonance Angiogram of the posterior circulation. PCA (posterior circulation arteries), SCA (superior cerebellar arteries), BA (basilar artery), AICA (right anterior inferior cerebellar artery), VAs (vertebral arteries), PICA (posterior inferior cerebellar arteries Contributed by Divyajot Sandhu, MD
References
Zibis A, Mitrousias V, Galanakis N, Chalampalaki N, Arvanitis D, Karantanas A. Variations of transverse foramina in cervical vertebrae: what happens to the vertebral artery? European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2018 Jun:27(6):1278-1285. doi: 10.1007/s00586-018-5523-2. Epub 2018 Feb 17 [PubMed PMID: 29455293]
Yuan SM. Aberrant Origin of Vertebral Artery and its Clinical Implications. Brazilian journal of cardiovascular surgery. 2016 Feb:31(1):52-9. doi: 10.5935/1678-9741.20150071. Epub [PubMed PMID: 27074275]
Meila D, Tysiac M, Petersen M, Theisen O, Wetter A, Mangold A, Schlunz-Hendann M, Papke K, Brassel F, Berenstein A. Origin and course of the extracranial vertebral artery: CTA findings and embryologic considerations. Clinical neuroradiology. 2012 Dec:22(4):327-33. doi: 10.1007/s00062-012-0171-0. Epub 2012 Sep 1 [PubMed PMID: 22941252]
Menshawi K, Mohr JP, Gutierrez J. A Functional Perspective on the Embryology and Anatomy of the Cerebral Blood Supply. Journal of stroke. 2015 May:17(2):144-58. doi: 10.5853/jos.2015.17.2.144. Epub 2015 May 29 [PubMed PMID: 26060802]
Level 3 (low-level) evidenceKomiyama M, Morikawa T, Nakajima H, Nishikawa M, Yasui T. High incidence of arterial dissection associated with left vertebral artery of aortic origin. Neurologia medico-chirurgica. 2001 Jan:41(1):8-11; discussion 11-2 [PubMed PMID: 11218642]
Level 3 (low-level) evidenceGabrielli R, Rosati MS. Ataxia and vertigo due to anomalous origin of the left vertebral artery. Journal of vascular surgery. 2013 Sep:58(3):803. doi: 10.1016/j.jvs.2012.04.045. Epub [PubMed PMID: 23972248]
Level 3 (low-level) evidenceLacout A, Khalil A, Figl A, Liloku R, Marcy PY. Vertebral arteria lusoria: a life-threatening condition for oesophageal surgery. Surgical and radiologic anatomy : SRA. 2012 May:34(4):381-3. doi: 10.1007/s00276-011-0867-x. Epub 2011 Sep 8 [PubMed PMID: 21901375]
Level 3 (low-level) evidenceGhandehari K, Ghandehari K. Interesting basis of vertebrobasilar arterial territory. Iranian journal of neurology. 2012:11(3):111-4 [PubMed PMID: 24250875]
Isaji T, Yasuda M, Kawaguchi R, Aoyama M, Niwa A, Nakura T, Matsuo N, Takayasu M. Posterior inferior cerebellar artery with an extradural origin from the V(3) segment: higher incidence on the nondominant vertebral artery. Journal of neurosurgery. Spine. 2018 Feb:28(2):154-159. doi: 10.3171/2017.5.SPINE161286. Epub 2017 Dec 1 [PubMed PMID: 29192876]
Zhou R, Liu D, Yu K, Chen Y, Li L, Xu J, Zhou H. Carotid and vertebral arterial variations in Alzheimer's disease. Current Alzheimer research. 2015:12(4):368-76 [PubMed PMID: 25817257]
Park JH, Kim JM, Roh JK. Hypoplastic vertebral artery: frequency and associations with ischaemic stroke territory. Journal of neurology, neurosurgery, and psychiatry. 2007 Sep:78(9):954-8 [PubMed PMID: 17098838]
Level 2 (mid-level) evidenceWaxenbaum JA, Reddy V, Black AC, Futterman B. Anatomy, Back, Cervical Vertebrae. StatPearls. 2023 Jan:(): [PubMed PMID: 29083805]
Eskander MS, Drew JM, Aubin ME, Marvin J, Franklin PD, Eck JC, Patel N, Boyle K, Connolly PJ. Vertebral artery anatomy: a review of two hundred fifty magnetic resonance imaging scans. Spine. 2010 Nov 1:35(23):2035-40. doi: 10.1097/BRS.0b013e3181c9f3d4. Epub [PubMed PMID: 20938397]
Level 2 (mid-level) evidenceCakmak O, Gurdal E, Ekinci G, Yildiz E, Cavdar S. Arcuate foramen and its clinical significance. Saudi medical journal. 2005 Sep:26(9):1409-13 [PubMed PMID: 16155658]
Cushing KE,Ramesh V,Gardner-Medwin D,Todd NV,Gholkar A,Baxter P,Griffiths PD, Tethering of the vertebral artery in the congenital arcuate foramen of the atlas vertebra: a possible cause of vertebral artery dissection in children. Developmental medicine and child neurology. 2001 Jul; [PubMed PMID: 11463182]
Level 3 (low-level) evidenceKoutsouraki E, Avdelidi E, Michmizos D, Kapsali SE, Costa V, Baloyannis S. Kimmerle's anomaly as a possible causative factor of chronic tension-type headaches and neurosensory hearing loss: case report and literature review. The International journal of neuroscience. 2010 Mar:120(3):236-9. doi: 10.3109/00207451003597193. Epub [PubMed PMID: 20374094]
Level 3 (low-level) evidenceZibis AH, Mitrousias V, Baxevanidou K, Hantes M, Karachalios T, Arvanitis D. Anatomical variations of the foramen transversarium in cervical vertebrae: findings, review of the literature, and clinical significance during cervical spine surgery. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2016 Dec:25(12):4132-4139 [PubMed PMID: 27554348]
Murlimanju BV, Prabhu LV, Shilpa K, Rai R, Dhananjaya KV, Jiji PJ. Accessory transverse foramina in the cervical spine: incidence, embryological basis, morphology and surgical importance. Turkish neurosurgery. 2011:21(3):384-7. doi: 10.5137/1019-5149.JTN.4047-10.0. Epub [PubMed PMID: 21845576]
Adigun OO, Reddy V, Sevensma KE. Anatomy, Head and Neck: Basilar Artery. StatPearls. 2023 Jan:(): [PubMed PMID: 29083786]
Neo M, Fujibayashi S, Miyata M, Takemoto M, Nakamura T. Vertebral artery injury during cervical spine surgery: a survey of more than 5600 operations. Spine. 2008 Apr 1:33(7):779-85. doi: 10.1097/BRS.0b013e31816957a7. Epub [PubMed PMID: 18379405]
Level 2 (mid-level) evidenceLunardini DJ, Eskander MS, Even JL, Dunlap JT, Chen AF, Lee JY, Ward TW, Kang JD, Donaldson WF. Vertebral artery injuries in cervical spine surgery. The spine journal : official journal of the North American Spine Society. 2014 Aug 1:14(8):1520-5. doi: 10.1016/j.spinee.2013.09.016. Epub 2013 Oct 10 [PubMed PMID: 24411832]
Level 2 (mid-level) evidenceSmith MD, Emery SE, Dudley A, Murray KJ, Leventhal M. Vertebral artery injury during anterior decompression of the cervical spine. A retrospective review of ten patients. The Journal of bone and joint surgery. British volume. 1993 May:75(3):410-5 [PubMed PMID: 8496209]
Level 2 (mid-level) evidenceMarks MP, Wojak JC, Al-Ali F, Jayaraman M, Marcellus ML, Connors JJ, Do HM. Angioplasty for symptomatic intracranial stenosis: clinical outcome. Stroke. 2006 Apr:37(4):1016-20 [PubMed PMID: 16497979]
Level 2 (mid-level) evidenceMohammadian R, Sharifipour E, Mansourizadeh R, Sohrabi B, Nayebi AR, Haririan S, Farhoudi M, Charsouei S, Najmi S. Angioplasty and stenting of symptomatic vertebral artery stenosis. Clinical and angiographic follow-up of 206 cases from Northwest Iran. The neuroradiology journal. 2013 Aug:26(4):454-63 [PubMed PMID: 24007733]
Level 3 (low-level) evidenceZhou Y, Wang L, Zhang JR, Zhou K, Shuai J, Gong ZL, Liu Y, Wei F, Han YF, Shen L, Yang QW. Angioplasty and stenting for severe symptomatic atherosclerotic stenosis of intracranial vertebrobasilar artery. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2019 May:63():17-21. doi: 10.1016/j.jocn.2019.02.017. Epub 2019 Mar 6 [PubMed PMID: 30850180]
Jenkins JS, Subramanian R. Vertebral and intracranial artery angioplasty. The Ochsner journal. 2003 Winter:5(1):36-9 [PubMed PMID: 22470254]
Caplan LR. "Top of the basilar" syndrome. Neurology. 1980 Jan:30(1):72-9 [PubMed PMID: 7188637]
Level 3 (low-level) evidencePirau L, Lui F. Vertebrobasilar Insufficiency. StatPearls. 2023 Jan:(): [PubMed PMID: 29489229]
Brandt T, Morcher M, Hausser I. Association of cervical artery dissection with connective tissue abnormalities in skin and arteries. Frontiers of neurology and neuroscience. 2005:20():16-29. doi: 10.1159/000088131. Epub [PubMed PMID: 17290108]
Klingelhöfer J, Conrad B, Benecke R, Frank B. Transcranial Doppler ultrasonography of carotid-basilar collateral circulation in subclavian steal. Stroke. 1988 Aug:19(8):1036-42 [PubMed PMID: 3041649]
Level 3 (low-level) evidencePotter BJ,Pinto DS, Subclavian steal syndrome. Circulation. 2014 Jun 3; [PubMed PMID: 24891625]
Level 3 (low-level) evidenceProvenzale JM, Sarikaya B. Comparison of test performance characteristics of MRI, MR angiography, and CT angiography in the diagnosis of carotid and vertebral artery dissection: a review of the medical literature. AJR. American journal of roentgenology. 2009 Oct:193(4):1167-74. doi: 10.2214/AJR.08.1688. Epub [PubMed PMID: 19770343]
Level 1 (high-level) evidenceVillablanca JP, Nael K, Habibi R, Nael A, Laub G, Finn JP. 3 T contrast-enhanced magnetic resonance angiography for evaluation of the intracranial arteries: comparison with time-of-flight magnetic resonance angiography and multislice computed tomography angiography. Investigative radiology. 2006 Nov:41(11):799-805 [PubMed PMID: 17035870]
Almeida JP, Medina R, Tamargo RJ. Management of posterior fossa arteriovenous malformations. Surgical neurology international. 2015:6():31. doi: 10.4103/2152-7806.152140. Epub 2015 Feb 25 [PubMed PMID: 25745586]
Machado MC, Kodaira S, Musolino NR. Persistence of intrasellar trigeminal artery and simultaneous pituitary adenoma: description of two cases and their importance for the differential diagnosis of sellar lesions. Arquivos brasileiros de endocrinologia e metabologia. 2014 Aug:58(6):661-5 [PubMed PMID: 25211451]
Level 3 (low-level) evidenceLambert SL, Williams FJ, Oganisyan ZZ, Branch LA, Mader EC Jr. Fetal-Type Variants of the Posterior Cerebral Artery and Concurrent Infarction in the Major Arterial Territories of the Cerebral Hemisphere. Journal of investigative medicine high impact case reports. 2016 Jul-Sep:4(3):2324709616665409. doi: 10.1177/2324709616665409. Epub 2016 Sep 13 [PubMed PMID: 27660767]
Level 3 (low-level) evidence