Introduction
Wellens syndrome describes a pattern of electrocardiographic (ECG) changes, particularly deeply inverted or biphasic T waves in leads V2-V3, that is highly specific for critical, proximal stenosis of the left anterior descending (LAD) coronary artery. It is alternatively known as anterior, descending, T-wave syndrome. Typically when patients with Wellens syndrome present to the emergency department they are pain-free, and usually cardiac enzymes are normal or only slightly elevated. However, it is important to recognize the ECG patterns as these patients are at high risk for impending large anterior wall acute myocardial infarction. In fact, when Drs. De Zwaan, Wellens, and colleagues first identified the syndrome in the early 1980s, they noted that 75% of patients with these ECG findings went on to develop acute, anterior, wall, myocardial infarction within weeks if they were treated with only medical management. Definitive treatment typically involves cardiac catheterization with percutaneous coronary intervention (PCI) to relieve the occlusion.[1][2][3][4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The causes of Wellens syndrome are similar to any conditions that cause cardiac heart disease, including the following:
- Atherosclerotic plaque
- Coronary artery vasospasm
- Hypoxia
- Increase in cardiac demand
Risk factors:
- Diabetes mellitus
- Family history of premature heart disease
- Hypertension
- Increased age
- Hypercholesterolemia
- Hyperlipidemia
- Metabolic syndrome
- Occupational stress
- Smoking
Epidemiology
Wellens syndrome represents a pre-infarction state of coronary artery disease. The risk factors for Wellens syndrome are therefore the same as those for coronary artery disease including dyslipidemia, hypertension, diabetes, sedentary lifestyle, obesity, familial history, and smoking. The ECG pattern of Wellens syndrome is relatively common in patients who exhibit symptoms consistent with unstable angina. In studies performed by Dr. Wellens and colleagues, the ECG pattern was present in 14% to 18% of patients admitted for unstable angina.
Pathophysiology
Wellens syndrome results from a temporary obstruction of the LAD coronary artery. Usually, this is caused by the rupture of an atherosclerotic plaque leading to LAD occlusion, with subsequent clot lysis or other disruption of the occlusion before complete myocardial infarction has taken place. Wellens syndrome represents a pre-infarction state. However, due to the unstable nature of the coronary perfusion, these patients are at high risk for extensive myocardial infarction of the anterior cardiac wall and possibly death. The exact mechanism of the ECG changes of Wellens syndrome is not known, but some theorize that coronary artery spasm and stunned myocardium cause it. Others postulate that it is caused by repetitive transmural ischemia-reperfusion leading to myocardial edema.
History and Physical
Patients with Wellens syndrome usually exhibit symptoms consistent with acute coronary syndrome. The typical complaints include chest pain that is described as tightness or pressure-like, often induced by physical activity and relieved by rest. The pain may radiate to the neck, jaw, or shoulder. Upon presentation to the emergency department, patients will usually be pain-free. However, the ECG pattern as described below may persist. Patients typically appear comfortable with an unremarkable physical exam though they may demonstrate some mild distress with diaphoresis, similar to those patients having an acute myocardial infarction.
Evaluation
Diagnostic criteria for Wellens syndrome are as follows:
- Deeply inverted T waves in leads V2 and V3 (may also be seen in leads V1, V4, V5, and V6) OR biphasic T waves (with initial positivity and terminal negativity) in V2 and V3[5][6]
PLUS
- Isoelectric or minimally elevated ST segment, less than 1 mm (in other words, no signs of an acute anterior wall myocardial infarction)
- Preservation of precordial R-wave progression AND no precordial Q waves (in other words, no signs of old anterior wall infarct)
- Recent history of angina
- ECG pattern present in a pain-free state
- Normal or slightly elevated cardiac markers
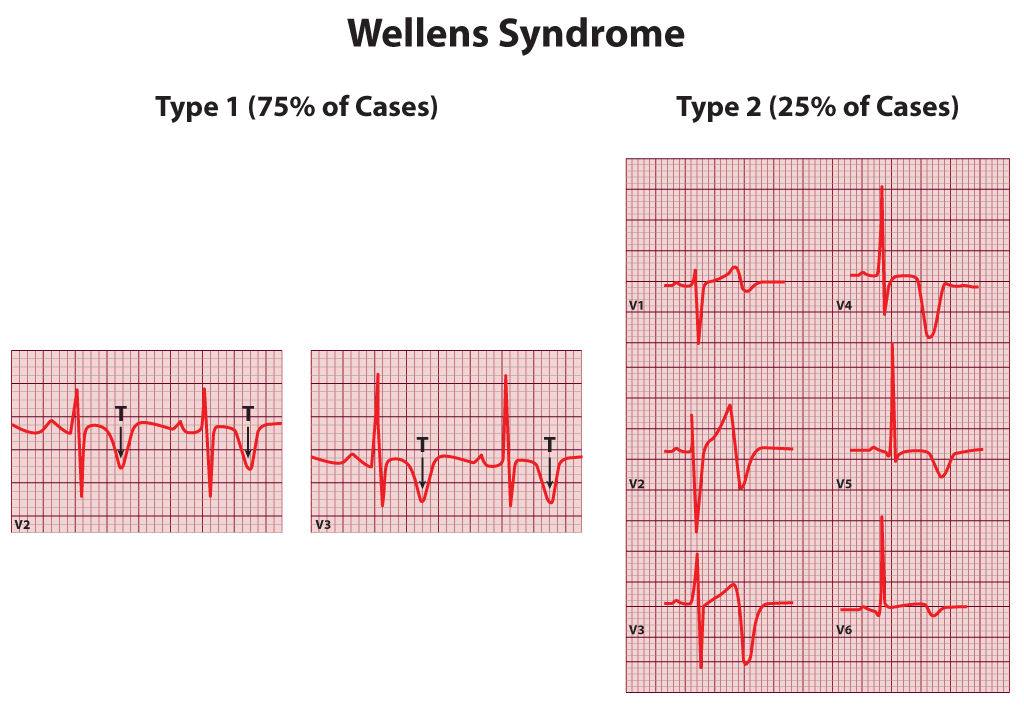
Two patterns of T waves can be seen in Wellens syndrome. Type-A T waves are biphasic, with initial positivity and terminal negativity. These T wave findings are present in approximately 25% of cases. Type-B T waves are deeply and symmetrically inverted. These findings are present in approximately 75% of cases. The 2 types of T waves found in Wellens syndrome exist on a spectrum of disease with type-A T waves evolving into type-B T waves. The T-wave abnormalities may be persistent, remaining in place for hours to weeks, even when the patient is pain-free.
Wellens syndrome is not always an acute process. It can develop over days to weeks. The ECG pattern often develops when the patient is not experiencing chest pain. When the patient does experience chest pain, the ST segment and T-wave pattern can appear to normalize into hyperacute upright T waves (so-called “pseudo-normalization”) or even develop into ST-segment elevations.
Cardiac biomarkers including troponin may be falsely reassuring in patients with Wellens syndrome as they frequently result within normal limits. In one prospective study, only 12% of patients with Wellens’ pattern on ECG had elevated cardiac enzymes, and these elevations were less than twice the upper limit of normal.
Treatment / Management
As soon as the diagnosis of Wellens syndrome is made or suspected, consult a cardiologist. In addition, contact an interventional cardiologist because the definitive treatment is cardiac catheterization with PCI. Until this occurs, treat Wellens syndrome similarly to an acute myocardial infarction including antiplatelet therapy with aspirin, anticoagulation with heparin, and nitrates and beta blockers if the patient is not hypotensive. However, it is important to note that Wellens’ patients do poorly with medical management alone, and as stated above, definitive treatment is procedural. Admit patients that are pain-free and stable on a monitored floor. All symptomatic patients need intensive care until (ICU) admission and immediate consultation with an interventional cardiologist for cardiac catheterization on a more emergent basis. Because Wellens syndrome patients have critical narrowing of the LAD coronary artery, a stress test should be avoided as this can precipitate an acute myocardial infarction and sudden death. Upon coronary angiography, the cardiologist can plan for revascularization of the LAD coronary artery.[7][8][9][10](B3)
Differential Diagnosis
The differential for anterior T-wave inversion (TWI) also includes central nervous system (CNS) injury (so-called “cerebral” T waves), left ventricular hypertrophy (LVH), right bundle branch block (RBBB), hypertrophic cardiomyopathy (HOCM), and pulmonary embolism (PE) among others. These patterns typically can be distinguished via additional electrocardiographic features that are outside the scope of this discussion.
Although the Wellens pattern is highly specific for stenosis of the LAD coronary artery by an occlusive plaque, there exist mimics of Wellens syndrome or so-called “pseudo-Wellens syndrome.” Causes of this include cocaine use, in which coronary vasospasm can result in the typical Wellens ECG pattern. This usually resolves following the clearance of cocaine from the body, and the ECG ultimately returns to normal. It is important to recognize this and obtain an appropriate history, especially in a young patient with no risk factors for acute myocardial ischemia, as giving beta blockers could be detrimental due to potential unopposed stimulation of alpha receptors. In some case reports, marijuana use has also been shown to result in the Wellens pattern for unclear reasons. Another rare cause is myocardial bridging, in which the coronary artery tunnels under a bridge of myocardium resulting in LAD coronary artery stenosis. Additionally, the Wellens pattern can be seen in Takotsubo cardiomyopathy, which is thought be the result of myocardial edema.
Prognosis
As discussed above, Wellens syndrome is the result of critical stenosis of the left anterior descending coronary artery manifesting in characteristic ECG changes. It is a pre-infarction state. However, if not recognized early and properly treated, the disease tends to progress to a large acute anterior wall myocardial infarction, which can lead to substantial morbidity and mortality. Therefore it is important for clinicians to recognize Wellens pattern early.
Pearls and Other Issues
Wellens syndrome describes a pattern of electrocardiographic (ECG) changes discussed above that is highly specific for critical, proximal stenosis of the LAD coronary artery. Typically when patients with Wellens syndrome present to the emergency department they are pain-free, and usually cardiac enzymes are normal or only slightly elevated. However, it is important to recognize the ECG patterns as these patients are at high risk for impending large acute anterior wall acute myocardial infarction. Definitive treatment typically involves cardiac catheterization with percutaneous coronary intervention (PCI) to relieve the occlusion.
Enhancing Healthcare Team Outcomes
The diagnosis and management of Wellens syndrome are best with an interprofessional team that includes the nurse practitioner, primary care provider, cardiologist, and cardiac surgeon. As soon as the diagnosis of Wellens syndrome is made or suspected, the cardiologist must be consulted. Until this occurs, treat Wellens syndrome similarly to an acute myocardial infarction including antiplatelet therapy with aspirin, anticoagulation with heparin, and nitrates and beta-blockers if the patient is not hypotensive. However, it is important to note that Wellens’ patients do poorly with medical management alone, definitive treatment is procedural. These patients must always be admitted and monitored. An immediate cardiac catheterization is necessary. Because Wellens syndrome patients have critical narrowing of the LAD coronary artery, a stress test should be avoided as this can precipitate an acute myocardial infarction and sudden death. Upon coronary angiography, the cardiologist can plan for revascularization of the LAD coronary artery. The prognosis for patients who are managed with surgery or PCI is good, but if treatment is delayed or medical therapy is undertaken, the outcomes are poor.[11][12]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
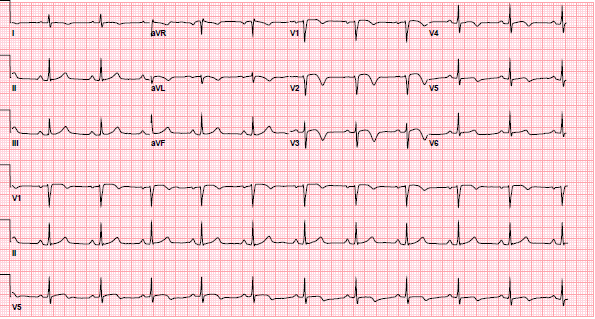
Wellens Syndrome. ECG demonstrating the second type of pattern associated with Wellens syndrome. In leads V2-V3, the T waves are deeply inverted, typical of Type-B T waves. As discussed, Type-A T waves often evolve into Type-B T waves, which is what occurred in this patient.
Contributed by E Regan, MD
References
Singh D, Suliman I, Chyshkevych I, Dabage N. A Pathognomonic Electrocardiogram That Requires Urgent Percutaneous Intervention: A Case of Wellens Syndrome in a Previously Healthy 55-Year-Old Male. The American journal of case reports. 2019 Jan 28:20():117-120. doi: 10.12659/AJCR.912056. Epub 2019 Jan 28 [PubMed PMID: 30686820]
Level 3 (low-level) evidenceRamanathan S, Soaly E, Cherian A, Heidous MA. 'T' twist: Wellens syndrome. QJM : monthly journal of the Association of Physicians. 2019 May 1:112(5):373-374. doi: 10.1093/qjmed/hcy276. Epub [PubMed PMID: 30476339]
Wang X, Sun J, Feng Z, Gao Y, Sun C, Li G. Two case reports of Wellens' syndrome. The Journal of international medical research. 2018 Nov:46(11):4845-4851. doi: 10.1177/0300060518800857. Epub 2018 Oct 3 [PubMed PMID: 30282519]
Level 3 (low-level) evidenceMarzlin KM. Wellens Syndrome. AACN advanced critical care. 2018 Fall:29(3):360-364. doi: 10.4037/aacnacc2018289. Epub [PubMed PMID: 30185504]
Udechukwu N, Shrestha P, Khan MZ, Donato AA. Wellens' syndrome: a close call. BMJ case reports. 2018 Jun 21:2018():. pii: bcr-2018-225376. doi: 10.1136/bcr-2018-225376. Epub 2018 Jun 21 [PubMed PMID: 29930191]
Level 3 (low-level) evidenceRamires TG, Sant'Anna J, Pais J, Picarra BC. Wellens' syndrome: a pattern to remember. BMJ case reports. 2018 Apr 10:2018():. pii: bcr-2018-224582. doi: 10.1136/bcr-2018-224582. Epub 2018 Apr 10 [PubMed PMID: 29636339]
Level 3 (low-level) evidenceStankovic I, Kafedzic S, Janicijevic A, Cvjetan R, Vulovic T, Jankovic M, Ilic I, Putnikovic B, Neskovic AN. T-wave changes in patients with Wellens syndrome are associated with increased myocardial mechanical and electrical dispersion. The international journal of cardiovascular imaging. 2017 Oct:33(10):1541-1549. doi: 10.1007/s10554-017-1181-4. Epub 2017 May 27 [PubMed PMID: 28551719]
Yasin OZ, Rubio-Tapia A, Sarano ME. Wellens Syndrome with Syncope but Not Chest Pain. Cardiology. 2017:137(1):9-13. doi: 10.1159/000452707. Epub 2016 Dec 13 [PubMed PMID: 27951539]
Coutinho Cruz M, Luiz I, Ferreira L, Cruz Ferreira R. Wellens' Syndrome: A Bad Omen. Cardiology. 2017:137(2):100-103. doi: 10.1159/000455911. Epub 2017 Feb 15 [PubMed PMID: 28196358]
Grautoff S. Wellens' syndrome can indicate high-grade LAD stenosis in case of left bundle branch block. Herzschrittmachertherapie & Elektrophysiologie. 2017 Mar:28(1):57-59. doi: 10.1007/s00399-017-0489-z. Epub 2017 Feb 9 [PubMed PMID: 28185080]
Level 3 (low-level) evidenceMoseley MJ, Allen D, Martell M. Electrocardiogram lead selection using critical thinking: concerning women and heart disease and a case of wellens syndrome. Dimensions of critical care nursing : DCCN. 2010 Nov-Dec:29(6):253-8. doi: 10.1097/DCC.0b013e3181f0b7db. Epub [PubMed PMID: 20940576]
Level 3 (low-level) evidenceCosta AP, Hirdes JP, Heckman GA, Dey AB, Jonsson PV, Lakhan P, Ljunggren G, Singler K, Sjostrand F, Swoboda W, Wellens NI, Gray LC. Geriatric syndromes predict postdischarge outcomes among older emergency department patients: findings from the interRAI Multinational Emergency Department Study. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2014 Apr:21(4):422-33. doi: 10.1111/acem.12353. Epub [PubMed PMID: 24730405]