Introduction
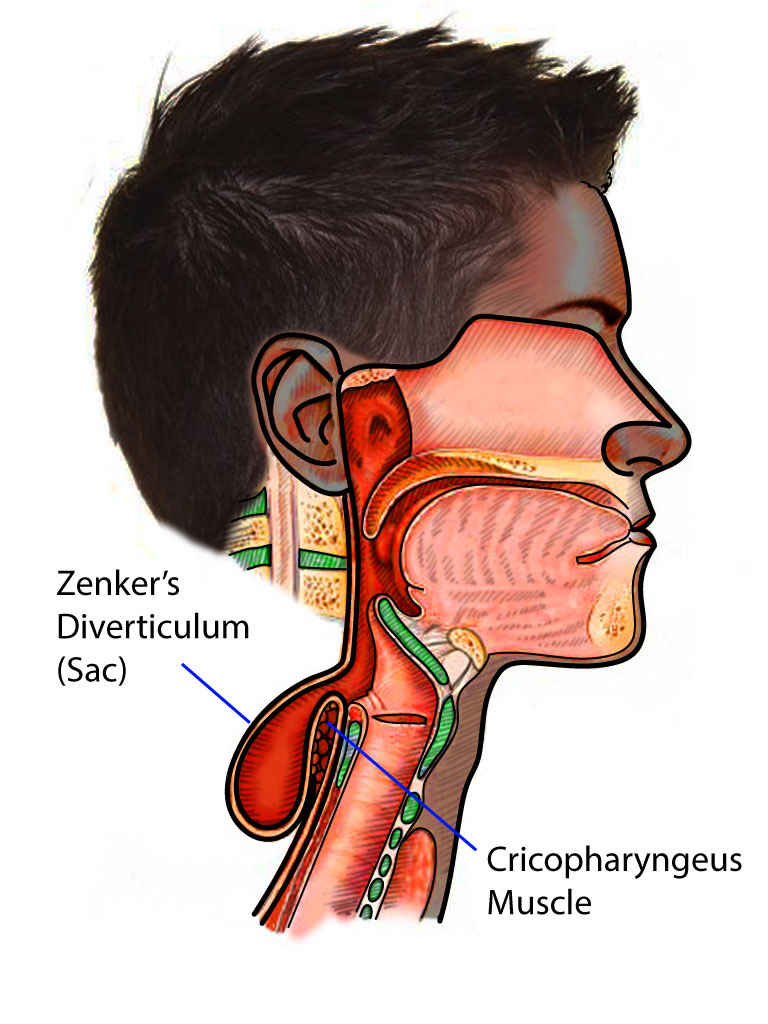
Zenker's diverticulum is a type of diverticulum that develops in the hypopharynx, typically between the cricopharyngeus (CP) muscle and the inferior pharyngeal constrictor muscle. It only involves the mucosa and submucosal layers and does not involve the muscular layer, hence making it a false diverticulum. It may also occur in other parts of the esophagus, such as between the oblique and transverse fibers of the CP muscle, known as Killian-Jamieson area, and between the CP muscle and the esophageal muscles, known as Laimer triangle.[1][2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of Zenker's diverticulum is not fully understood, but most of the hypotheses revolve around the abnormal structure and physiology of the cricopharyngeus muscle. Professionals believe that abnormal pressure during swallowing causes dehiscence of this muscle leading to the formation of a Zenker diverticulum. Therefore, this diverticulum is an acquired mucosal herniation between the horizontal and oblique fibers of the cricopharyngeus muscle.[4]
The diverticulum develops between the transverse fibers of the CP muscle and the oblique fibers of the inferior constrictor muscle; this area is often known as Killian triangle.
Epidemiology
It is a rare disorder of the esophagus, primarily seen in elderly individuals, peaking between the seventh and ninth decades of life. Occurs rates range from 0.01% to 0.11% of the population. It is more common in men than in women. Zenker diverticulum rate varies in different parts of the world being more common in northern Europe, the United States of America, and Canada and rarely occurs in Japan and Indonesia. However, the true incidence is difficult to ascertain due to a significant number of patients who do not seek treatment. Zenker diverticulum is rare before the age of 40.[5]
Pathophysiology
Although there are multiple theories regarding the pathophysiology and development of Zenker's diverticulum, no clear consensus exists. It is understood that a Zenker diverticulum involves impaired cricopharyngeal compliance, usually due to fibrotic changes, what causes increased intrabolus pressure with swallowing. As a result of this, the hypopharyngeal pressure increases, leading to herniation at the weak point just above the cricopharyngeus. The resulting false diverticulum retains food particles and salivary secretions leading to regurgitation, halitosis, dysphagia, and aspiration.
In most cases, Zenker diverticulum extends in the left neck and this is believed to be due to the slight convexity of the cervical esophagus.
In general, manometry is not used to evaluate patient's with Zenker diverticulum because the resulting pressure measurements are often confused with pressure generated by swallowing and contractions of the upper esophageal sphincter.
Histopathology
Histological examination of a Zenker diverticulum is rarely done. Microscopic evaluation of the pouch usually shows a sac containing stratified squamous epithelium, and the submucosa lining often shows fibrous tissue. Rarely, ulcerations or evidence of cancer, squamous cell or carcinoma in situ, may be present.
History and Physical
The development of this diverticulum leads to retention of food particles which leads to complaints of regurgitation, halitosis, aspiration, and difficulty swallowing. Patients with Zenker diverticulum will typically present with a long history of dysphagia followed by a sensation of food stuck in the throat. Up to 98% of patients have the primary complaints of dysphagia. Other common symptoms include recurrent coughing, fetor ex ore (halitosis), and unexplained weight loss. Rarely, a visible lump might be seen in the neck.
The symptoms may be present for months or years.
Evaluation
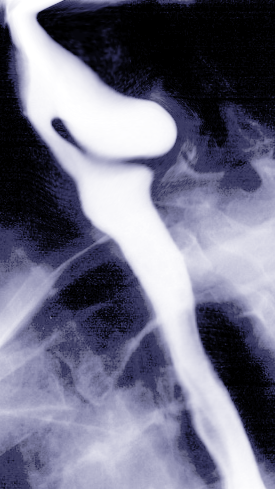
Barium swallow with videofluoroscopy provides information regarding its size, location, and character of the mucosal lining, and diagnoses the condition. Upper endoscopy, which includes both flexible and rigid assessment, are also used and typically essential in the surgical evaluation. Staging of the Zenker diverticulum is imperative to the overall evaluation. There are 3 staging systems: Lahey, Morton, and Van Overbeek staging systems. Only one of the 3 may be used. The staging is typically reliant on the size of the pouch in which the bigger the size, the higher the staging.[6]
Endoscopy may reveal fibrosis around the diverticulum which limits the risk of local abscess formation. Endoscopy may reveal pooling of food in the diverticulum.
Treatment / Management
Only symptomatic lesions need treatment; lesions less than 2 centimeters rarely require any treatment. In some cases of Zenker diverticulum associated with achalasia, botulinum toxin may help relieve symptoms of dysphagia. For all other large Zenker diverticulum, surgery is indicated. However, since Zenker diverticula occur in the elderly population, great care is required in selecting patients for surgery. The Zenker diverticulum can be treated by an open procedure or via an endoscopic approach. During surgery, it is vital to divide the cricopharyngeus muscle to relieve the elevated pressure zone and eliminate the pouch of the diverticulum. A 1-cm myotomy is adequate in most cases.
However, myotomy alone is associated with a high recurrence of symptoms. Hence, the myotomy should be combined with a more definitive procedure.
Recently lasers have been used during upper endoscopy to resect the diverticulum instead of staples. Overall, lasers have been shown to have fewer recurrences and faster improvement in symptoms compared to the use of staplers. Open surgery usually is more invasive and requires longer hospitalization but does provide rapid symptom relief and low rates of recurrence. Complications of surgery include injury to the laryngeal nerve, bleeding, esophageal perforation, and trauma to the oral cavity.[3][4][7]
Pros and cons
Diverticulectomy with myotomy
- Is a definitve procedure and removes the diverticulum
- Tissue is available for histopathological analysis
- Symptom relief is immediate
- Recurrence of symptoms is low
- Surgery can take time and patients do need to be admitted. Initiation of an oral diet is delayed until the suture line has healed.
- There is a risk of RLN injury, esophageal stenosis, fistula formation, esophageal perforation and mediastinitis.
Endoscopic diverticulectomy with stapler
- Short surgery and can be repeated
- Hosptial stay is short and oral diet can be started quickly
- Effective and safe procedure
- However, endoscopy surgery may not be possible in all patients and does not remove the diverticulum. There is no tissue for analysis but recurrences can be managed by a repeat procedure. There is a risk of RLN injury, esophageal stenosis, fistula formation, esophageal perforation and mediastinitis.
Differential Diagnosis
Although rare, cancers, such as squamous cell carcinomas may be present in conjunction with a Zenker's diverticulum. This is imperative to rule out during an assessment. One must ask about smoking history and consumption of very hot or very cold liquids (teas, coffee). Other differential diagnoses that one must think about is achalasia, GERD or Barrett esophagus, esophagitis (radiation, immunocompromised, STI), stroke in the acute setting, and ulcerations due to retention of food. It is important to be thorough in the evaluation of these patients.
Staging
The Lahey, Mortons, and Van Overbeek staging systems are used for evaluation of a Zenker's diverticulum. These staging systems are used to describe the degree of the Zenker's diverticulum, usually in the sense of pouch size. Barium swallow with videofluoroscopy is the radiographic methods used for staging.
The Lahey classification is often used to stage Zenker diverticulum and includes the following:
- Stage 1: Small mucosal protrusion is visible
- Stage ll: A definite sac is seen bu the esophagus and hypopharynx are in line
- Stage lll: The hypopharynx is seen in line with the diverticulum and the esophagus is pushed anteriorly and appears indented.
Prognosis
The prognosis for these patients is dependant on which surgical procedure was performed. Patients who undergo diverticulectomy with cricopharyngeus myotomy, immediate symptoms relief occurred in 90% to 100% of patient. The long-term symptoms recurrent rate is 2% to 33%. Mortality occurs in zero to 9.5% of these patients while morbidity, which includes mediastinitis, esophageal stenosis, recurrent laryngeal nerve damage, pharyngocutaneous fistula, hematoma, and esophageal perforation occurs in 4% to 47% of patients who underwent this procedure. In patients who received treatment via endoscopic diverticulectomy with a stapler, immediate symptoms relief occurred in 94% to 100% of patients. The long-term symptoms recurrence rate ranges from zero to 47%. Mortality occurs in zero to 1% and morbidity, which includes recurrent laryngeal nerve damage, bleeding, mediastinitis, dental injury, esophageal perforation, diverticulum perforation, and cervical emphysema occurred in 10% to 31%. Prognosis is varied and dependent on multiple factors that include patients age and comorbidities.
Complications
Complications of this disease are varied and dependant on the surgical approach taken, patient age and comorbidities. Since this disease is mainly a disease of the elderly, the prognosis is typically poor, and recurrence rates are high.
A serious complication of Zenker diverticulum is aspiration. Other complications include bleeding, fistula formation with the trachea and obstruction of the esophagus.
Patients and clinicians need to aware of potential complications which include recurrent laryngeal nerve paralysis, mediastinitis, esophageal perforation/stenosis, cervical emphysema, among others.
Postoperative and Rehabilitation Care
Proper follow-up is imperative to minimizing post-operative complications and infections.
Deterrence and Patient Education
Patients must be aware of the benefits and risk of Zenker's diverticulum and the potential usefulness of surgery.
Enhancing Healthcare Team Outcomes
an interprofessional approach to Zenker diverticulum is necessary as the diagnosis can be delayed because of the vague symptoms. Zenker diverticulum usually presents in the middle-aged and elderly population with symptoms of dysphagia and regurgitation. The condition is progressive and can lead to aspiration, halitosis, chronic cough, and hoarseness. Patients admitted with a diagnosis of Zenker diverticulum need to be looked after an interprofessional team of healthcare professionals because there are many treatment options. There is no data to show that one treatment is better than the other. The best treatment depends on patient age, presence of comorbidity, size of the diverticulum, surgeon experience, and patient preferences.
Hence, the nurse should educate the patient and family about the disease, its outlook, and management. At the same time, the nurse should take aspiration precautions by avoiding a supine position. A speech consult should be obtained to determine the risk of aspiration and a dietary consult to determine what type of foods are safe. Because many of these patients are frail and weak, a physical therapy consult may help increase exercise tolerance and ambulation. After the surgery, the patient should be closely monitored by the nurse for dysphagia and aspiration. Only a team approach can lower the morbidity associated with Zenker diverticulum. [8][9](Level V).
Outcomes
Even though there are several methods to manage Zenker diverticulum, the outcomes after all of these treatments are safe and effective. Almost all patients report an improvement in immediate symptoms. Unfortunately, there are no randomized trials or long-term studies to determine which is the most effective procedure and which is durable. The key is to have an experienced surgeon or endoscopist. The low prevalence of this disorder may make it difficult to conduct large randomized trials; hence the choice of treatment remains one of personal choice. [10][11][12](Level V)
Media
(Click Image to Enlarge)
References
Achille G, Castellana M, Russo S, Montepara M, Giagulli VA, Triggiani V. Zenker Diverticulum: A Potential Pitfall in Thyroid Ultrasound Evaluation: A Case Report and Systematic Review of Literature. Endocrine, metabolic & immune disorders drug targets. 2019:19(1):95-99. doi: 10.2174/1871530318666180910122003. Epub [PubMed PMID: 30198446]
Level 3 (low-level) evidenceTabola R, Lewandowski A, Cirocchi R, Augoff K, Kozminska U, Strzelec B, Grabowski K. Zenker diverticulum: Experience in surgical treatment of large diverticula. Medicine. 2018 May:97(19):e0557. doi: 10.1097/MD.0000000000010557. Epub [PubMed PMID: 29742690]
Ciuc D, Birlă R, Panaitescu E, Tanţău M, Constantinoiu S. Zenker Diverticulum Treatment: Endoscopic or Surgical? Chirurgia (Bucharest, Romania : 1990). 2018 Mar-Apr:113(2):234-243. doi: 10.21614/chirurgia.113.2.234. Epub [PubMed PMID: 29733017]
Ishaq S, Sultan H, Siau K, Kuwai T, Mulder CJ, Neumann H. New and emerging techniques for endoscopic treatment of Zenker's diverticulum: State-of-the-art review. Digestive endoscopy : official journal of the Japan Gastroenterological Endoscopy Society. 2018 Jul:30(4):449-460. doi: 10.1111/den.13035. Epub 2018 Mar 7 [PubMed PMID: 29423955]
Hoffmann M, Fazel A, Mews KG, Ambrosch P. 32 years of experience with CO(2) -LASER-assisted treatment for Zenker's Diverticulum - an update of 227 patients treated in Kiel. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2017 Jun:42(3):592-596. doi: 10.1111/coa.12777. Epub 2016 Nov 9 [PubMed PMID: 27762065]
Henry MA, Lerco MM, Tagliarini JV, Castilho EC, Novaes FT, Lamonica VC. Pharyngoesophageal diverticulum: evaluation of treatment results. Revista do Colegio Brasileiro de Cirurgioes. 2013 Mar-Apr:40(2):104-9 [PubMed PMID: 23752635]
Level 2 (mid-level) evidenceTenorio L,Palacios F, [Efficacy and safety of the endoscopic management of Zenker diverticulum with IT-Knife 2 device]. Revista de gastroenterologia del Peru : organo oficial de la Sociedad de Gastroenterologia del Peru. 2017 Jul-Sep [PubMed PMID: 29093582]
Shapiro J. Oropharyngeal dysphagia: pathophysiology, clinical assessment and management. Revista de gastroenterologia de Mexico. 1994 Apr-Jun:59(2):91-5 [PubMed PMID: 7991973]
Wasserzug O, Zikk D, Raziel A, Cavel O, Fleece D, Szold A. Endoscopically stapled diverticulostomy for Zenker's diverticulum: results of a multidisciplinary team approach. Surgical endoscopy. 2010 Mar:24(3):637-41. doi: 10.1007/s00464-009-0651-8. Epub 2009 Aug 18 [PubMed PMID: 19688391]
Level 2 (mid-level) evidenceMazza M, Bergamini AN, Parise P, Cossu A, Adamenko O, Elmore U, Rosati R. Treatment of Zenker's Diverticulum With Endoscopic Stapled Esophago-divertisculostomy (ESD): Analysis of Long-term Outcome. Surgical laparoscopy, endoscopy & percutaneous techniques. 2017 Dec:27(6):445-448. doi: 10.1097/SLE.0000000000000473. Epub [PubMed PMID: 28915203]
Desbeaux A, Gronnier C, Piessen G, Vanderbeken M, Ruolt N, Triboulet JP, Mariette C. Same-day discharge in benign esophageal surgery: a prospective cohort study. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus. 2017 Apr 1:30(4):1-7. doi: 10.1093/dote/dow036. Epub [PubMed PMID: 28375480]
Jones D, Aloraini A, Gowing S, Cools-Lartigue J, Leimanis M, Tabah R, Ferri L. Evolving Management of Zenker's Diverticulum in the Endoscopic Era: A North American Experience. World journal of surgery. 2016 Jun:40(6):1390-6. doi: 10.1007/s00268-016-3442-0. Epub [PubMed PMID: 26956900]