Introduction
The zygomatic arch includes segments of the temporal bone (posteriorly) and the zygoma (anteriorly), contributing vital to the midface's structure and aesthetic appearance. As the primary determinant of the width of the cheeks, the zygomatic arch articulates with several bones of the craniofacial skeleton and supports critical muscles such as the masseter and zygomaticus major. The zygoma and its articulations with other facial bones comprise the zygomaticomaxillary complex (ZMC), also known as the zygomatico-orbito-maxillary complex. Fractures of the zygomatic arch or any of its bony articulations can cause significant functional and cosmetic morbidity. Managing zygomatic arch and ZMC fractures should be patient-specific but may range from simple observation to open reduction with internal fixation.
Anatomy
The zygomatic arch is the most lateral projection of the midface; this structure plays a key role because it absorbs and dissipates traumatic forces away from the cranial base. The zygoma also contributes significantly to the inferior and lateral orbital walls. Fractures of the zygoma necessitate evaluation for concomitant fractures of the orbit.
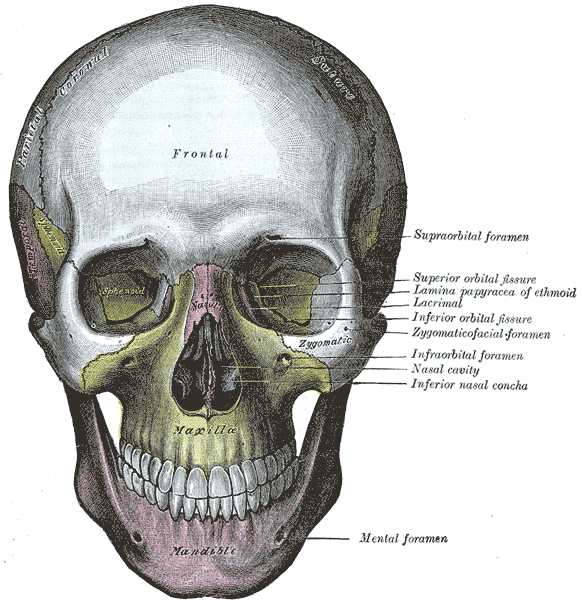
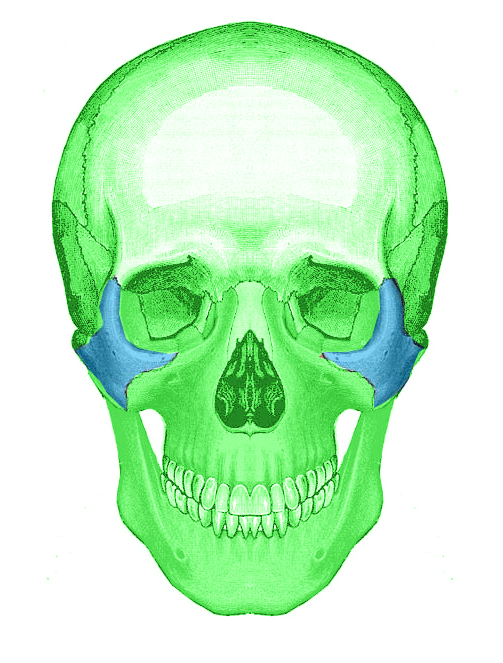
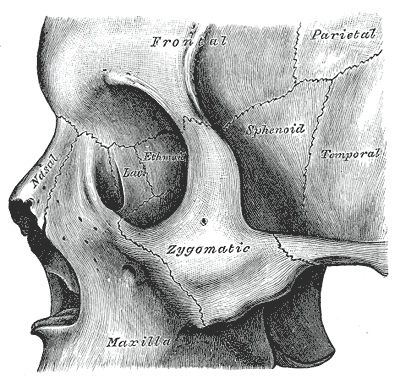
The zygoma has 4 articulations, referred to as the ZMC complex (see Images. Skull Anatomy Surface Markings and Frontal Skull and Zygomatic Bones and Left Zygomatic Bone in Situ):
- Zygomaticotemporal suture: This is the temporal process of the zygoma, which articulates with the zygomatic process of the temporal bone to form the zygomatic arch.
- Zygomaticomaxillary (ZM) suture: This suture line crosses the inferior orbital rim, resulting in the frequent coexistence of orbital floor fractures with ZMC fractures. The ZM suture is within the ZM buttress, a key vertical support structure within the midface. The other 2 vertical buttresses of the midface are the nasomaxillary and the pterygomaxillary buttresses.
- Zygomaticofrontal (ZF) suture: This is lateral to the brow and is a small suture line easily accessed via a short lateral brow incision. Properly reducing a displaced ZF suture is critical to reestablishing correct facial height.
- Zygomaticosphenoidal (ZS) suture: The alignment of this suture is critical when reducing a fracture to reestablish pre-traumatic orbital volume, even though this suture line is not typically fixated after reduction.[1]
Fractures of the zygomaticomaxillary complex may be called "tripod fractures." The correct terminology is "tetrapod fracture," given the 4 bony articulations of the zygoma.
Neuroanatomy
Paresthesia of the face is a common sequela of ZMC fractures given the proximity of sensory nerves, such as the infraorbital nerve, the zygomaticofacial nerve, and the zygomaticotemporal nerve (all branches of cranial nerve V2) to the zygoma.
- The infraorbital nerve exits the maxilla via the infraorbital foramen, medial to the articulation between the maxilla and the zygoma. The infraorbital nerve provides sensory input from the cheek, upper lip, nose, and anterior maxillary dentition.
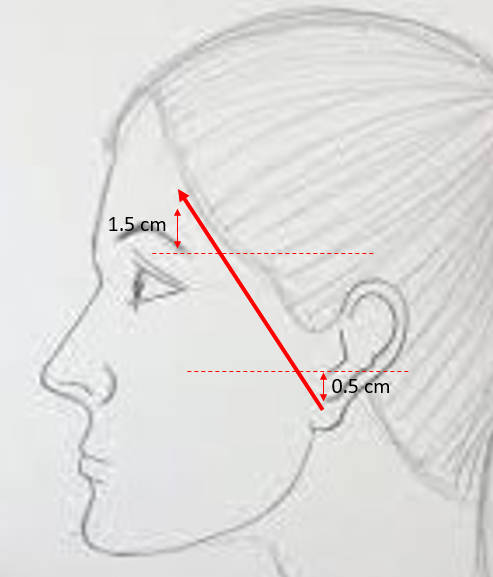
- The zygomaticofacial and zygomaticotemporal nerves transmit sensory input from the lateral cheek and anterior temporal area, respectively. They are branches of the zygomatic nerve that arise in the pterygopalatine fossa and enter the orbit via the inferior orbital fissure before traveling along the lateral orbital wall (See Image. Temporal Branch Course). The zygomaticofacial and zygomaticotemporal branches then exit via correspondingly named foramina in the zygoma.
Severe ZMC fractures may also result in ipsilateral facial palsy because the facial nerve is intimately associated with the zygomatic arch (see Image. Zygomatic Arch). The facial nerve's frontal branch emerges from the parotid gland deep into the superficial musculoaponeurotic system and crosses the zygomatic arch on its superficial surface. The frontal branch then transitions to the undersurface of the temporoparietal fascia, where it travels to innervate the frontalis muscle.[2]
Muscular Anatomy
The temporalis muscle originates along the temporal line of the parietal and frontal bones and travels deep to the ZA to insert into the coronoid process of the mandible; it also has attachments to the zygoma. Depressed fractures of the zygomatic arch may impede movement of the temporalis muscle and cause trismus.
The masseter muscle originates on the inferior aspect of the zygoma and zygomatic arch and inserts on the angle of the mandible. This is a powerful muscle of mastication, and its contraction can displace unstable bone segments inferiorly in certain cases.
The zygomaticus major and minor are muscles of facial expression that originate on the zygoma and are inserted near the modiolus of the oral commissure to assist with corner-of-mouth elevation and lateralization during smiling.
Other Landmarks
The tubercle of Whitnall is the attachment site of the lateral canthal tendon, located on the medial surface of the frontal process of the zygoma.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Zygomatic arch fractures tend to result from high-energy impact trauma, such as interpersonal violence, motor vehicle accidents, or sporting injuries (see Image. Zygoma Fracture). In a 2020 study published by Cohn et al, assault was the most common cause of ZA fractures (55%), followed by falls (27%), and motor vehicle accidents (18%). In contrast, a 2012 study performed by Ungari et al reported equal rates of ZA fractures between assaults and motor vehicle accidents (29%), with sports injuries following (16%), then falls (14%), domestic accidents (9%), and work accidents (5%).[3]
Epidemiology
Most zygomatic arch fractures occur in males (~80%) in the third to fourth decades of life.[4][5] Zygomaticomaxillary complex fractures are common, and estimates suggest that ZMC fractures account for 25% of facial fractures.[5] African Americans appear to be affected most commonly (61%-64%), with Caucasians second (18%-25%), Hispanic patients third (7%-12%), and Asians fourth (5%-7%).[4]
History and Physical
History
When evaluating patients with zygoma fractures, it is crucial to ascertain the mechanism and timing of the injury. Determining whether the injury was caused by blunt or penetrating trauma is also essential, as penetrating trauma is more likely to involve deeper neurovascular structures.[5] A history of prior facial trauma or facial surgeries may complicate fracture repair and should be ascertained preoperatively.
Physical Examination
As with any patient with trauma, it is important to begin the examination by evaluating the "ABCs." Ensuring the patient has an adequate airway, is breathing spontaneously, and has any bleeding under control is critical. Evaluating the cervical spine for any associated injury, as high-energy impacts to the face or head are also liable to affect the spine, is crucial. The face should be inspected, noting any obvious asymmetry, lacerations, and ecchymosis. Ipsilateral epistaxis is common and may require packing if severe. An ophthalmologic examination should include visual acuity, visual field assessments, and extraocular movement evaluation. In a patient with a ZMC injury, depression of the malar eminence may cause facial flattening and may be apparent from a "bird's eye" view. However, facial flattening may be obscured by overlying soft tissue edema in the acute phase. Applying cold compresses may alleviate the edema and facilitate a more detailed physical examination. The clinician should also note the position of the globe; enophthalmos may be visible from a "worm's-eye" view. The face should be palpated, noting any bony step-offs or mobility of the underlying craniofacial skeleton. A comprehensive cranial nerve examination should be completed, paying particular attention to facial movement and sensation.
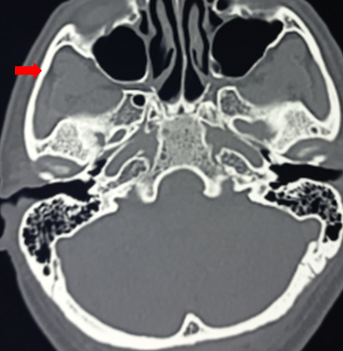
Evaluation
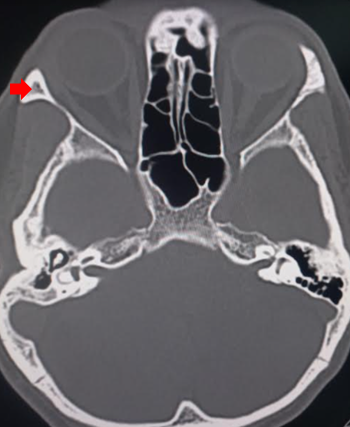
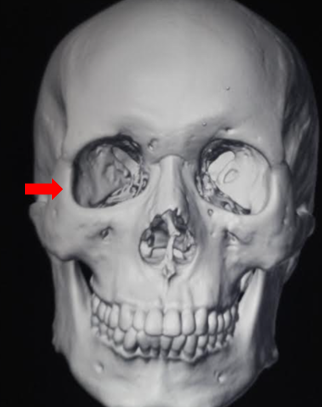
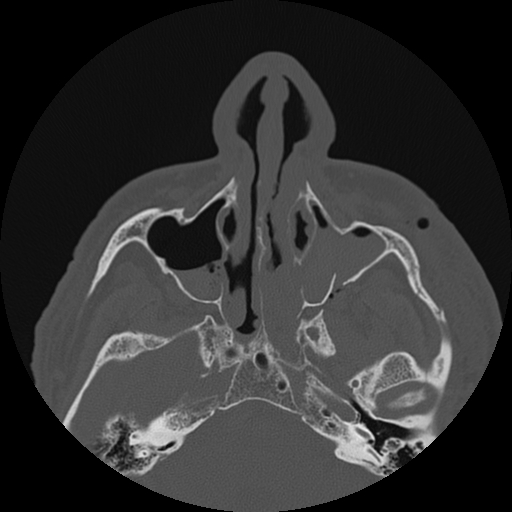
After a comprehensive history and physical examination, imaging is necessary for a suspected zygomatic arch or ZMC fracture see Image. Zygomatic Arch). Historically, the Waters view plain film x-ray was used to evaluate facial fractures, although a submentovertex view provides better visualization for evaluating zygomatic arch fractures. A computed tomography (CT) scan is now the gold standard imaging modality, typically performed using fine cuts (<1 mm) without contrast (see Image. Face CT, Tripod Fracture). Three-dimensional reconstruction is beneficial for preoperative planning (see Images. Zygomatic Bone in 3D and 3D Reconstructions of Left ZOMC.). There may also be a role for intraoperative CT scanning to assess the adequacy of fracture reduction, but there is not strong evidence to support its use on a routine basis.[6]
Classification of ZMC Fractures
Various classification systems have been used to categorize ZMC fractures. Below is a system proposed by Zingg et al in 1992:
Type A: an incomplete zygomatic fracture that involves one articulation of the zygoma
- A1: zygomatic arch fracture
- A2: lateral orbital wall fracture
- A3: infraorbital rim fracture
Type B: all 4 articulations are fractured (a complete tetrapod fracture), with the zygomatic bone itself remaining intact
Type C: a multi-fragment zygomatic fracture, wherein all 4 articulations are fractured, and the body of the zygoma is fractured as well [7]
Treatment / Management
Managing ZMC fractures can be broadly classified into 3 categories: medical management, closed reduction, and open reduction internal fixation. Further, managing ZMC fractures is controversial and requires an individual approach to each case.
Medical Management
Zygoma fractures are usually manageable by observation alone if there is minimal or no displacement of fracture segments. Additionally, medical management may be the choice if other comorbidities preclude safe surgery. No strong evidence supports the use of prophylactic antibiotics for patients with upper and midface fractures. However, some surgeons prescribe a 5- to 7-day course of antibiotics, particularly if communication exists with the maxillary sinus. If prescribed, antibiotics should cover sinonasal flora, eg, amoxicillin-clavulanate.[8] Additionally, a soft diet is usually recommended to prevent the distraction of fractures by muscle contraction.
Operative Management
The indications for operative management of zygomatic arch (ZA) and ZMC fractures are to restore the form and function of the midface. Fractures of the ZMC or ZA can often lead to unsightly malar depression, which should be corrected to restore normal facial contour and symmetry. Zygomaticomaxillary complex fractures can also cause significant functional issues, including trismus, enophthalmos, diplopia, and paresthesias of the infraorbital nerve. A suspected globe injury is a contraindication to operative management of ZMC fractures and should be addressed before any other surgical intervention is performed in the facial skeleton.
A key principle of facial fracture repair is a reduction with the fixation of fractures that involve the facial buttresses to restore the structural integrity of the midface. Several methods have evolved to repair ZA and ZMC fractures. However, closed reduction may be adequate for simple, low-velocity injuries of the ZA (see Type A1 below) that are nondisplaced or minimally displaced and remain stable after initial reduction.[5] Open reduction and internal fixation (see Image. ORIF of ZOMC Fracture) should be the approach of choice for fractures that are comminuted or are likely to be unstable after reduction. Typically, low-profile titanium mini-plates are used to fixate the fractured bone segments, working to repair fractures from laterally to medially and from stable to non-stable segments. Absorbable plates may also be used for fixation in cases where follow-up is unlikely, but such plates should not be routinely used because absorbable plates are biomechanically weaker than titanium plates.[9] In any case, the conventional sequence of events involves surgical exposure of the displaced fracture site(s) as described below, reduction of the fractured bone segment(s), confirmation of alignment by direct visualization via the exposure obtained initially, and finally, rigid fixation. It is common practice among trauma surgeons to plate the zygomaticofrontal (ZF) suture first, then the zygomaticomaxillary (ZM) buttress or the infraorbital, and lastly, to repair the orbital floor, if necessary.
Management algorithm based on Zingg's classification system of ZMC fractures as described above (see Evaluation):[10]
- Type A1 (zygomatic arch fracture): Nondisplaced fractures of the ZA are often managed conservatively. In contrast, displaced fractures of the ZA require reduction, which is possible via a Gillies approach using a temporal incision, a transcutaneous Carroll-Girard screw directly over the depressed fracture site, or a Keen approach via an intraoral incision in the maxillary vestibule. Isolated arch fractures that are unstable after reduction can be splinted externally with steel wires or heavy sutures or plated via a coronal incision.[11]
- Type A2 (lateral orbital wall fracture): Reduction and fixation of this area are best accomplished via a lateral brow incision or an upper blepharoplasty incision. Mini-plates provide adequate stabilization of these fractures.
- Type A3 (infraorbital rim): The infraorbital rim should be reduced and plated to restore its normal contour and approached via either a transconjunctival or a subciliary lower eyelid incision.
- Type B (tetrapod fracture): Mildly displaced tetrapod fractures may occasionally be reduced via a Gillies or Keene approach. Most tetrapod fractures, however, remain unstable after such reduction attempts and ultimately require open reduction and internal fixation with single-point fixation (zygomaticomaxillary or zygomaticofrontal suture), 2-point fixation (ZM and ZF sutures), or 3-point fixation (ZM and ZF sutures, and infraorbital rim). Finally, the ZA can be plated via a coronal incision or pre-existing lacerations as the fourth point of fixation if necessary.
- Type C (comminuted tetrapod fracture): These fractures constitute absolute indications for open reduction and internal fixation (ORIF). Treatment is similar to that used for type B fractures, with ORIF of the ZM buttress, infraorbital rim, ZF suture, zygomaticotemporal suture, and zygoma fragments as necessary.
Orbital Floor Exploration and Repair
Indications for repair of the orbital floor remain controversial. Generally, if greater than 50% of the floor is disrupted or the defect is ≥1 cm2 in area, the orbital floor should be repaired. Additional indications include non-resolving oculocardiac reflex, diplopia in primary gaze, >3 mm of enophthalmos, and entrapment of extraocular muscles. Different materials may be used to reconstitute the orbital floor, including titanium mesh, porous polyethylene, vinyl or polydioxanone sheeting, dura, split calvarium, or temporalis fascia.[10] After repair, a forced duction test should be performed to ensure normal mobility of the globe (see Video. Forced Duction Testing).
Number of Fixation Points
No consensus exists on how many fixation points are necessary when treating ZMC fractures. In general, the more comminuted or unstable a fracture is, the more fixation points will be needed to ensure a good result, and most surgeons will typically place at least two screws in each plate on each side of a fracture line to prevent rotation of the bone fragments around the screws. A 2019 meta-analysis published by Jazayeri et al suggested that 3-point fixation reduced fracture instability and orbital dystopia at three months post-operatively compared to 2-point fixation, but the quality of evidence was low.[12] The zygoma and its articulations should be palpated after fixation to determine if additional fixation points are needed, and an intraoperative or postoperative CT scan should be used to visualize the articulations of the zygoma and verify adequate reduction.(A1)
Order of Plating
There is no universally accepted plating order for multipoint fixation of ZMC fractures. During single-point fixation, the ZM suture is usually plated. The ZF suture can also be plated, although most surgeons would argue that the intraoral incision used to plate the ZM buttress is less morbid than the external incision needed to access the ZF suture. When performing two-point fixation, the ZF suture should be plated first, followed by the ZM buttress. During 3 or 4-point fixation, the ZF requires plating first, then the ZM buttress, then the infraorbital rim. If one plans to plate the ZA from the outset, it can often be plated first to ensure adequate projection of the ZMC. If concomitant repair of the orbital floor is necessary, it should take place after the zygoma has been reduced, as mobilizing the zygoma often affects the configuration of the orbital floor; if the zygoma is impacted significantly, reducing it into its anatomical position will frequently increase the size of the defect by distracting the bone segments of the orbital floor.
Soft Tissue Suspension
If the lateral canthal tendon has been avulsed, it requires resuspension with suturing to the tubercle of Whitnall. The malar soft tissue may also require suspension to the periosteum of the zygoma to prevent ectropion or scleral show in the long term.
Summary of Surgical Approaches
- Existing lacerations are utilized to approach fixation sites (if possible)
- Zygomaticofrontal suture
- Lateral brow incision
- Upper blepharoplasty incision
- Transconjunctival incision with lateral canthotomy and cantholysis
- Coronal or hemicoronal incision
- Zygomaticomaxillary suture
- Intraoral gingivolabial sulcus incision
- Infraorbital rim and orbital floor
- Subciliary or subtarsal incision
- Transconjunctival incision
- Zygomatic arch
- Percutaneous stab incision for placement of Carroll-Girard screw: requires a conspicuous scar and theoretically puts the facial nerve at risk
- Temporal incision (Gillies): conceals the scar in the hairline. Facial nerve can be preserved by dissecting deep into the temporalis fascia during dissection
- Intraoral incision (Sheen): conceals the scar in the mouth and avoids facial nerve injury. Careful, watertight closure of intraoral incision can prevent plate exposure in the mouth and oroantral fistula formation to maxillary sinus
- Coronal or hemicoronal incision
Timing of Repair
Fracture repair should take place as quickly as possible before scarring and setting of bony fragments into their posttraumatic positions begins. Because significant facial edema disguises aesthetic deformities and increases exposure difficulty, fracture repair should ideally be performed within 2 to 3 days of the initial injury. Fracture repair from 2 to 6 weeks post-injury is more difficult due to fibrosis and scarring. Fracture repair beyond 6 weeks is challenging but possible using intraoperative imaging and navigation. If orbital floor repair is necessary, it should ideally be performed within 2 weeks of injury.[10]
Differential Diagnosis
The zygoma contributes a significant portion of the inferior and lateral orbital walls. Any zygoma fracture warrants evaluating possible fractures or injury of the orbit, particularly open globe injuries. Cervical spine injury must be ruled out, as well as concomitant facial fractures, including frontal sinus, nasal, midface (eg, Lefort, naso-orbito-ethmoid), and mandible fractures. Midface trauma may result in nasal septal hematoma formation, which should be assessed and managed as necessary to avoid septal necrosis and perforation or saddle nose deformity. Lastly, malocclusion may result from mandibular or midfacial trauma and should be evaluated and addressed as well.
Prognosis
Comminuted fractures of the ZMC have worse outcomes than non-comminuted fractures, with a 33% higher rate of corrective surgery.[13] Some (5%-9%) patients, including those with non-comminuted fractures, will require a second operation due to inadequate fracture reduction.[13][14] Indications for revision surgery include persistent enophthalmos, diplopia, facial contour irregularity, and temporomandibular joint dysfunction.[13][15] Some degree of postoperative asymmetry occurs in 20% to 40% of patients, with major asymmetry occurring in 3% to 4%. Paresthesia may be persistent in the long term for 22% to 65% of patients.[16]
Complications
Complications from ZMC fractures can be related to the initial injury or operative management and can include:
- Pain
- Wound infection
- Facial asymmetry
- Scarring
- Bleeding (epistaxis)
- Hardware failure (exposure, palpability)
- Infraorbital nerve paresthesia
- Temperature sensitivity
- Facial paresis or paralysis
- Poor cosmetic result
- Trismus [13][17]
Orbital complications (usually related to concomitant orbital floor fracture):
- Blindness
- Decreased visual acuity
- Ectropion/entropion/lid malposition
- Corneal exposure/abrasion
- Ptosis
- Epiphora
- Enophthalmos/orbital dystopia
- Diplopia
- Superior orbital fissure syndrome
Postoperative and Rehabilitation Care
Postoperative care and recovery vary depending on the degree of injury and reconstructive methods employed. Regardless of fracture severity or technique selected, the patient should be advised to refrain from strenuous activity for at least 2 weeks to allow for complete healing with minimal bruising and swelling. Depending on the fractures involved, ancillary care postoperatively may include:
- Lubricating eye drops (orbital fractures)
- Nasal irrigations (communication with the sinonasal contents)
- Oral rinses (intraoral incisions used)
- Soft diet (displaced ZA or mandible fractures/malocclusion)
Skin incision lines require antibiotic ointment application (must be an ophthalmic ointment for periorbital incisions) for at least 72 hours postoperatively before transitioning to petrolatum ointment until the incisions heal completely. Avoiding sun exposure and proper sun protection, as well as using silicone-based scar creams and lotions may help improve the appearance of any scars. Postoperatively, the patient should be followed closely for any potential complications, particularly infection-related and visual complaints. Visits usually occur 1 week postoperatively and then every few weeks after until the fractures appear stable and any complications that may arise have resolved.
Consultations
Any patient with sufficient trauma to sustain a ZA or ZMC fracture should undergo a full trauma evaluation to rule out any concomitant injuries to determine the most appropriate consultations (eg, neurosurgery, ophthalmology, orthopedic surgery, plastic surgery, otolaryngology, oral-maxillofacial surgery, vascular surgery). Other than the primary craniofacial trauma surgery service (otolaryngology/oral-maxillofacial surgery/plastic surgery), the most likely consultant will be an ophthalmologist or oculoplastic surgeon because of the high rate with which ocular injuries accompany ZMC fractures.
The most common concomitant ocular injury is subconjunctival hemorrhage, which occurs in 67% to 87% of patients with ZMC fractures.[18][19] Other less common ocular complications include symptomatic diplopia (16% of patients), hyphema (13%), decreased visual acuity (13%), traumatic optic neuropathy (6%), choroidal rupture (6%), corneal abrasion (5%), vitreous hemorrhage (3%), retinal detachment (3%), retinal hemorrhage (1.5%), and mydriasis (1.5%).[18][19]
Deterrence and Patient Education
As with any facial fractures, the risk of sustaining ZA or ZMC fractures may be lowered with the wear of helmets with face protection, particularly during participation in certain sports (ice hockey, American football, etc) or when riding motorcycles, all-terrain vehicles or snowmobiles. Proper helmet wear will also help to prevent other injuries, such as skull fractures and traumatic brain injuries.[20][21]
Pearls and Other Issues
Additional information on zygomatic arch fracture include:
- Existing evidence regarding the management of ZMC fractures is relatively sparse, and universally accepted management standards are lacking; attention to form and function remains crucial when evaluating and repairing such fractures.
- Treatment options for ZMC fractures include observation, closed reduction, or open reduction and internal fixation, depending on the severity of the fractures.
- The smallest incision and fixation points possible should achieve a stable reduction and fixation.
- There should be a low threshold for consulting ophthalmology to rule out orbital injury.
- There is no compelling evidence for routine antibiotic use when treating zygomatic fractures.
Enhancing Healthcare Team Outcomes
Successful management of ZA and ZMC fractures requires coordination between the surgical team (otolaryngology/plastic surgery/oral and maxillofacial surgery), ophthalmology, anesthesiology, trauma surgery, and perioperative nursing. Specialists in these fields must operate as a cohesive, interprofessional team to facilitate safe and effective healthcare for patients with ZA and ZMC fractures. Meticulous preoperative evaluation is paramount; it is essential to identify and document concomitant injuries to ensure that the most pressing issues are addressed first. Ocular injuries require attention before fracture management.
Comorbidities require consideration when deciding between operative and conservative management. Postoperatively, the nursing staff should carefully monitor visual acuity and extraocular movements. The patient should understand that paresthesia of the infraorbital nerve and trismus are not uncommon and may persist. The interprofessional team should caution the patient to abstain from heavy lifting and strenuous activity for at least 2 weeks after surgery. This interprofessional approach is the best way to obtain optimal patient outcomes with minimal adverse events.
Media
(Click Image to Enlarge)
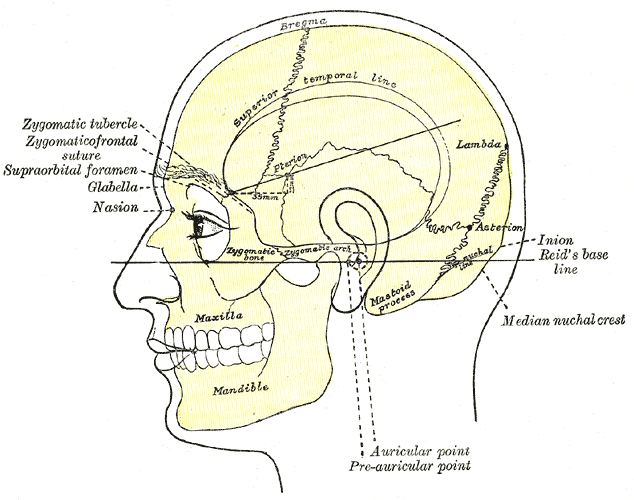
Skull Anatomy Surface Markings. Side view of the head showing the surface relations of the bones of the skull and markings, including the zygomatic tubercle, zygomaticofrontal suture, supraorbital foramen, glabella, nasion, inion, Reid baseline, superior temporal line, bregma, lambda, and asterion.
Henry Vandyke Carter, Public domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
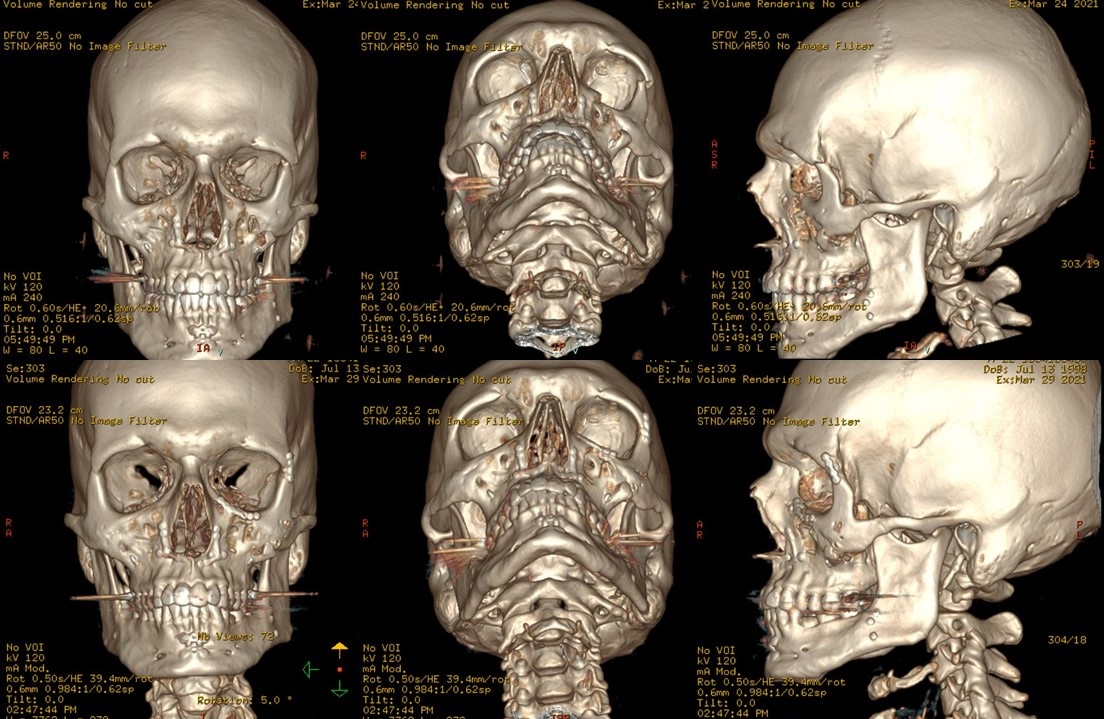
3D Reconstructions of Left ZOMC. Reconstructions are from noncontrast computed tomography scans of a left zygomatico-orbito-maxillary complex fracture (ZOMC or tripod fracture). Preoperative views are on the top, demonstrating displacement of the zygomaticomaxillary, zygomaticofrontal, and zygomaticosphenoid sutures. Postoperative views are on the bottom, demonstrating reduction and plating of the infraorbital rim and zygomaticofrontal suture.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
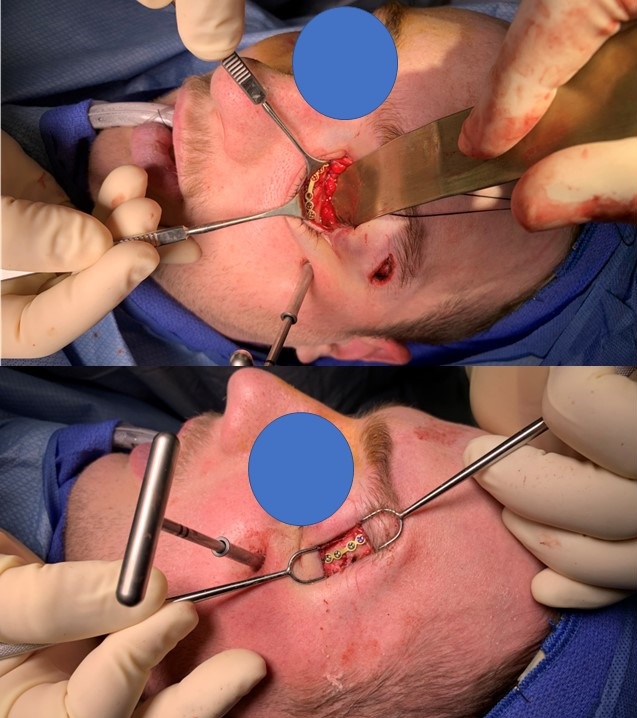
ORIF of ZOMC Fracture. Open reduction and internal fixation of a zygomatico-orbito-maxillary complex fracture. The upper image demonstrates a transconjunctival approach to the orbital floor and infraorbital rim, with a titanium miniplate in place on the infraorbital rim. The lower image demonstrates a lateral brow incision approach to the zygomaticofrontal suture, with a miniplate in place on the suture. Of note, there is a Carroll-Girard screw in place, which was used to reduce the zygoma into its anatomical position.
Contributed by Marc H Hohman, MD, FACS
(Click Video to Play)
Forced Duction Testing in a Pediatric Patient. Performed with 0.3-0.5 mm forceps after orbital floor fracture to identify entrapment of orbital contents within the maxillary sinus. The test should also be performed after orbital floor repair to ensure no tissue is entrapped. If tissue is entrapped, the range of motion is decreased, particularly with the upward rotation of the globe.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)
References
Lee EI, Mohan K, Koshy JC, Hollier LH Jr. Optimizing the surgical management of zygomaticomaxillary complex fractures. Seminars in plastic surgery. 2010 Nov:24(4):389-97. doi: 10.1055/s-0030-1269768. Epub [PubMed PMID: 22550463]
Agarwal CA, Mendenhall SD 3rd, Foreman KB, Owsley JQ. The course of the frontal branch of the facial nerve in relation to fascial planes: an anatomic study. Plastic and reconstructive surgery. 2010 Feb:125(2):532-537. doi: 10.1097/PRS.0b013e3181c82e9d. Epub [PubMed PMID: 20124839]
Ungari C, Filiaci F, Riccardi E, Rinna C, Iannetti G. Etiology and incidence of zygomatic fracture: a retrospective study related to a series of 642 patients. European review for medical and pharmacological sciences. 2012 Oct:16(11):1559-62 [PubMed PMID: 23111970]
Level 2 (mid-level) evidenceCohn JE, Othman S, Bosco S, Shokri T, Evarts M, Papajohn P, Zwillenberg S. Management of Isolated Zygomatic Arch Fractures and a Review of External Fixation Techniques. Craniomaxillofacial trauma & reconstruction. 2020 Mar:13(1):38-44. doi: 10.1177/1943387520905164. Epub 2020 Mar 17 [PubMed PMID: 32642030]
Strong EB, Gary C. Management of Zygomaticomaxillary Complex Fractures. Facial plastic surgery clinics of North America. 2017 Nov:25(4):547-562. doi: 10.1016/j.fsc.2017.06.006. Epub [PubMed PMID: 28941507]
van Hout WM, Van Cann EM, Muradin MS, Frank MH, Koole R. Intraoperative imaging for the repair of zygomaticomaxillary complex fractures: a comprehensive review of the literature. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2014 Dec:42(8):1918-23. doi: 10.1016/j.jcms.2014.07.012. Epub 2014 Aug 13 [PubMed PMID: 25213198]
Zingg M, Laedrach K, Chen J, Chowdhury K, Vuillemin T, Sutter F, Raveh J. Classification and treatment of zygomatic fractures: a review of 1,025 cases. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 1992 Aug:50(8):778-90 [PubMed PMID: 1634968]
Level 3 (low-level) evidenceMundinger GS, Borsuk DE, Okhah Z, Christy MR, Bojovic B, Dorafshar AH, Rodriguez ED. Antibiotics and facial fractures: evidence-based recommendations compared with experience-based practice. Craniomaxillofacial trauma & reconstruction. 2015 Mar:8(1):64-78. doi: 10.1055/s-0034-1378187. Epub 2014 Sep 17 [PubMed PMID: 25709755]
Chu SG, Lee JS, Lee JW, Yang JD, Chung HY, Cho BC, Choi KY. Comparisons among four types of absorbable plates used for internal fixation of zygomaticomaxillary complex fractures. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2019 Mar:47(3):383-388. doi: 10.1016/j.jcms.2019.01.014. Epub 2019 Jan 17 [PubMed PMID: 30711471]
Marinho RO, Freire-Maia B. Management of fractures of the zygomaticomaxillary complex. Oral and maxillofacial surgery clinics of North America. 2013 Nov:25(4):617-36. doi: 10.1016/j.coms.2013.07.011. Epub 2013 Sep 20 [PubMed PMID: 24055372]
Hindin DI, Muetterties CE, Mehta C, Boukovalas S, Lee JC, Bradley JP. Treatment of Isolated Zygomatic Arch Fracture: Improved Outcomes with External Splinting. Plastic and reconstructive surgery. 2017 May:139(5):1162e-1171e. doi: 10.1097/PRS.0000000000003281. Epub [PubMed PMID: 28445374]
Jazayeri HE, Khavanin N, Yu JW, Lopez J, Shamliyan T, Peacock ZS, Dorafshar AH. Fixation Points in the Treatment of Traumatic Zygomaticomaxillary Complex Fractures: A Systematic Review and Meta-Analysis. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2019 Oct:77(10):2064-2073. doi: 10.1016/j.joms.2019.04.025. Epub 2019 Apr 30 [PubMed PMID: 31132344]
Level 1 (high-level) evidencevan Hout WM, Van Cann EM, Koole R, Rosenberg AJ. Surgical treatment of unilateral zygomaticomaxillary complex fractures: A 7-year observational study assessing treatment outcome in 153 cases. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2016 Nov:44(11):1859-1865. doi: 10.1016/j.jcms.2016.09.002. Epub 2016 Sep 13 [PubMed PMID: 27733307]
Level 2 (mid-level) evidenceStarch-Jensen T, Linnebjerg LB, Jensen JD. Treatment of Zygomatic Complex Fractures with Surgical or Nonsurgical Intervention: A Retrospective Study. The open dentistry journal. 2018:12():377-387. doi: 10.2174/1874210601812010377. Epub 2018 May 21 [PubMed PMID: 30202484]
Level 2 (mid-level) evidenceRajantie H, Snäll J, Thorén H. Postoperative temporomandibular dysfunction in patients with fractures of the zygomatic complex: a prospective follow-up study. The British journal of oral & maxillofacial surgery. 2018 Sep:56(7):573-577. doi: 10.1016/j.bjoms.2018.05.017. Epub 2018 Jun 30 [PubMed PMID: 29970263]
Balakrishnan K, Ebenezer V, Dakir A, Kumar S, Prakash D. Management of tripod fractures (zygomaticomaxillary complex) 1 point and 2 point fixations: A 5-year review. Journal of pharmacy & bioallied sciences. 2015 Apr:7(Suppl 1):S242-7. doi: 10.4103/0975-7406.155937. Epub [PubMed PMID: 26015723]
Birgfeld CB, Mundinger GS, Gruss JS. Evidence-Based Medicine: Evaluation and Treatment of Zygoma Fractures. Plastic and reconstructive surgery. 2017 Jan:139(1):168e-180e. doi: 10.1097/PRS.0000000000002852. Epub [PubMed PMID: 28027253]
Jamal BT, Pfahler SM, Lane KA, Bilyk JR, Pribitkin EA, Diecidue RJ, Taub DI. Ophthalmic injuries in patients with zygomaticomaxillary complex fractures requiring surgical repair. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2009 May:67(5):986-9. doi: 10.1016/j.joms.2008.12.035. Epub [PubMed PMID: 19375007]
Malik AH, Shah AA, Ahmad I, Shah BA. Ocular Injuries in Patients of Zygomatico-Complex (ZMC) Fractures. Journal of maxillofacial and oral surgery. 2017 Jun:16(2):243-247. doi: 10.1007/s12663-016-0907-5. Epub 2016 Apr 20 [PubMed PMID: 28439168]
Alfrey EJ, Tracy M, Alfrey JR, Carroll M, Aranda-Wikman ED, Arora T, Maa J, Minnis J. Helmet Usage Reduces Serious Head Injury Without Decreasing Concussion After Bicycle Riders Crash. The Journal of surgical research. 2021 Jan:257():593-596. doi: 10.1016/j.jss.2020.08.009. Epub 2020 Sep 12 [PubMed PMID: 32932191]
Rughani AI, Lin CT, Ares WJ, Cushing DA, Horgan MA, Tranmer BI, Jewell RP, Florman JE. Helmet use and reduction in skull fractures in skiers and snowboarders admitted to the hospital. Journal of neurosurgery. Pediatrics. 2011 Mar:7(3):268-71. doi: 10.3171/2010.12.PEDS10415. Epub [PubMed PMID: 21361765]
Level 2 (mid-level) evidence