Introduction
The anterolateral abdominal wall is a layered structure composed of skin, fascia, muscles, extraperitoneal fat, and peritoneum that extends from the thorax to the pelvis and bounds the abdominal cavity and its associated organs.[1] It plays an important role in the movement of the torso, stabilization of the spine, retention of a physical barrier, and increase and maintenance of intra-abdominal pressure.[2][3] Numerous nerves traverse the anterolateral abdominal wall to serve regions of the abdominal wall, pelvis, and perineum. A variety of pathologies have the potential to impact the anterolateral abdominal wall nerves, including trauma, neoplasm, and infection. Any clinical involvement of these nerves may result in pain, loss of sensation, or motor deficits and reduce an individual's quality of life.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
There is no clear consensus on the precise boundaries of the anterolateral abdominal wall. [1][4] Nevertheless, it can be defined as the region bounded by the subcostal (or thoracoabdominal) line superiorly, the superior border of the pubis and ilium inferiorly, and the posterior axillary line (a vertical line descending from the posterior axillary fold) posteriorly, and is continuous anteriorly.[5] The anterolateral abdominal wall is a term that recognizes the difficulty in demarcating boundaries between the lateral and anterior abdominal walls, although it may be possible to differentiate the lateral from the anterior abdominal walls by the anterior axillary line (a vertical line through the anterior axillary fold).[4]
The anterolateral abdominal wall, from superficial to deep, consists of skin, subcutaneous fat and fascia (including Camper's and Scarpa's fascia), abdominal wall muscles and their associated fascias, transversalis fascia, and parietal peritoneum.[6][7] The nerves present in the anterolateral abdominal wall consist of the thoracoabdominal, iliohypogastric, and ilioinguinal nerves arising from the ventral rami of the T6 to L1 spinal nerves.[6]
The thoracoabdominal nerves originate as branches of the ventral rami of the T7 to T12 spinal nerves (see Image. T7 to T11 Thoracoabdominal Nerves, T12 Thoracoabdominal Nerves).[6] The ventral rami of these spinal nerves emerge from the T6/T7 to T10/T11 intervertebral foramina, travel posterolaterally between the pleura of the lungs and the internal intercostal membrane, and carry on as intercostal nerves 7 to 11 situated between the ribs and the internal and innermost intercostal muscle layers. The 7th to 11th intercostal nerves traverse a long route along the inferior border of the ribs within the costal groove that also contains the intercostal artery and vein. These neurovascular structures are generally organized within the intercostal groove superior to inferior in order of the intercostal vein, artery, and nerve. The ventral ramus of the T12 thoracic spinal nerve continues as the subcostal nerve, running inferior to the inferior-most rib, and traverses along the inferior border of the twelfth rib, deep to the costal origin of the quadratus lumborum muscle.
The seventh through eleventh intercostal (T7-T11) and subcostal (T12) nerves give off lateral cutaneous nerve branches approximately at the mid-axillary line. The lateral cutaneous nerves arising from T7 and T8 predominantly return sensation from the inferior portion of the lateral thoracic wall, and the nerves arising from T9 to T12 predominantly return sensation from the lateral portion of the anterolateral abdominal wall. After crossing the subcostal line, intercostal nerves 7 to 12 and the subcostal nerve enter the abdominal wall and are referred to as the T7 to T12 thoracoabdominal nerves. The thoracoabdominal nerves travel within a neurovascular plane between the transversus abdominis and internal oblique muscles before piercing the posterior rectus sheath. They then travel anteriorly through openings in the linea semilunaris to return sensation from the skin overlying the rectus abdominis muscle.[8] Within the abdominal wall, the thoracoabdominal nerves travel at an anteroinferior angle so that T7 innervates skin just inferior to the xiphoid process of the sternum, T10 innervates at the region of the umbilicus, and T12 innervates suprapubic skin. This relationship is represented by the slightly inferior slope of the dermatomes of the anterolateral abdominal wall.[1] The T7 to T12 thoracoabdominal nerves provide segmental innervation to the skin overlying the anterolateral abdominal wall and the intercostal, rectus abdominis, pyramidalis, transversus abdominis, internal oblique, and external oblique muscles.
The iliohypogastric nerve originates from the superior branch of the ventral ramus of the L1 spinal nerve, which commonly receives communicating branches from T12.[6][9] The iliohypogastric nerve emerges from the lateral border of the psoas major muscle posteriorly. It travels laterally deep to the quadratus lumborum muscle to pierce the transversus abdominis muscle superior to the iliac crest. Within this neurovascular plane between the transversus abdominis and internal oblique muscles, the iliohypogastric nerve gives off a lateral cutaneous branch at the mid-axillary line to supply the skin of the L1 dermatome that overlies the buttocks and ilium. As the nerve passes the anterior superior iliac spine superiorly, it pierces the internal oblique muscle to travel between it and the external oblique muscle to continue on, superior to the inguinal ligament. The iliohypogastric nerve then pierces the external oblique aponeurosis approximately an inch superior to the superficial inguinal ring. It gives rise to terminal branches serving the skin overlying the inferior rectus abdominis muscle. Along its course, the iliohypogastric nerve will innervate the skin over the buttocks, ileum, and skin overlying the inferior portion of the rectus abdominis muscle. It will also send motor branches to the inferior portions of the transversus abdominis, external oblique, and internal oblique muscles.
The ilioinguinal nerve originates from the superior branch of the ventral ramus of the L1 spinal nerve.[6] Although there is considerable variation in its appearance in the posterior abdominal wall, the ilioinguinal nerve typically emerges from the lateral border of the psoas major muscle and travels anterolaterally, deep to the quadratus lumborum muscle, and pierces the transversus abdominis muscle at the iliac crest. The iliohypogastric and ilioinguinal nerves sometimes arise lateral to the psoas or even the quadratus lumborum from a common trunk of L1 before continuing along their typical largely parallel paths. The ilioinguinal nerve travels within the neurovascular plane between the transversus abdominis and internal oblique muscles until it reaches the superficial inguinal ring. At the superficial inguinal ring, the ilioinguinal nerve pierces the internal oblique muscle enters the inguinal canal, and travels along the spermatic cord (in males) or the round ligament (in females). The ilioinguinal nerve innervates the skin overlying the inguinal ligament, medial thigh, mons pubis, scrotum, root of the penis, and labia majora. It also contributes to the motor innervation of the inferior portions of the transversus abdominis, external oblique, and internal oblique muscles.
Embryology
During human embryonic development, usually 38 to 39 somites arise from paired paraxial mesoderm masses on either side of the neural tube during Carnegie Stages (CS) 9 to 13.[10]
The somites are the basis of the segmentation of the human body and produce the sclerotomes, dermatomes, myotomes, and syndetomes. The sclerotome produces segmental bony elements that develop adjacent to the notochord and result in the somites directing cellular migration of neural crest cells and spinal nerve axons and following the consequent development of the dermatome and myotome.[1][10] At Carnegie Stage 15, separate epaxial and hypaxial myotomes are formed with individual ventral and dorsal spinal nerve branches. From Carnegie Stage 17 and Carnegie Stage 18, spinal nerves originating from the neural tube are seen to penetrate the correspondent myotome. Three separate muscle layers develop as the myotome elongates ventrally during Carnegie Stage 18. The fusion of the left and right myotomes at the midline occurs during Carnegie Stages 20 to 23.
Blood Supply and Lymphatics
The seventh to eleventh intercostal (T7-T11) and subcostal (T12) nerves travel with the corresponding posterior intercostal arteries and veins to form intercostal neurovascular bundles in the relevant intercostal spaces.[11] The seventh through ninth posterior intercostal arteries anastomose with the corresponding anterior intercostal arteries that arise from the musculophrenic artery. The tenth and eleventh posterior intercostal arteries continue with the thoracoabdominal nerves to travel as neurovascular bundles in the abdominal wall.[1]
The structures of the anterolateral abdominal wall receive arterial supply from the superior and inferior epigastric, superficial epigastric, musculophrenic, posterior intercostal, and anterior intercostal arteries.
Venous drainage of the anterolateral abdominal wall consists of a large venous plexus that drains into the superior epigastric, internal thoracic, and lateral thoracic veins superiorly and the inferior and superficial epigastric veins inferiorly (see Image. The Sympathetic Nerves).
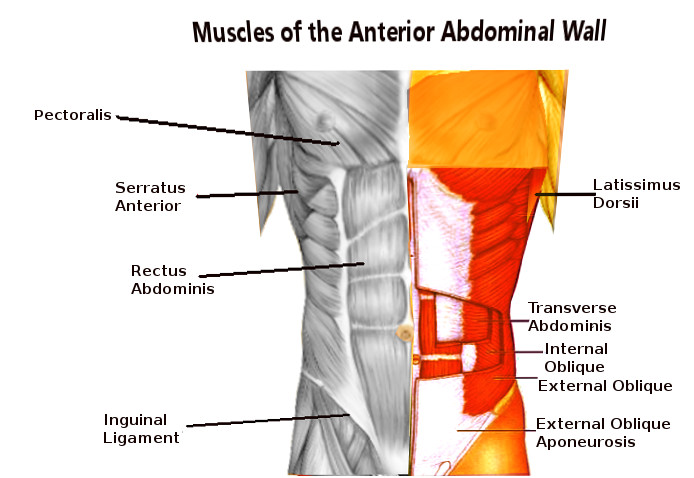
Muscles
Muscles in the anterolateral abdominal wall include the transversus abdominis, internal oblique, external oblique, pyramidalis, and rectus abdominis muscles (see Image. Abdominal Wall Muscles). The rectus abdominis muscle is enclosed by the anterior and posterior rectus sheaths formed by the transversus abdominis, internal oblique, and external oblique aponeurosis. The linea alba separates the left and right rectus abdominis muscles as a combination of the anterior and posterior rectus sheaths. The linea semilunaris forms the lateral enclosure of the rectus abdominis muscles formed by the aponeurosis of the transversus abdominis, internal oblique, and external oblique muscles. The transversus abdominis, external oblique, and internal oblique muscles are layered (deep to superficial, respectively) and extend from the lateral border of the rectus abdominis across the remainder of the abdominal wall. These muscles have attachments to the inguinal ligament and form the borders of the inguinal canal. The pyramidalis muscle is a physiological variant and is present in 80% of the population.[7] When present, it has significant variation, typically being found between the anterior border of the rectus abdominis muscle and the posterior border of the posterior rectus sheath on the lower part of the rectus abdominis muscle.[12]
Surgical Considerations
Specific nerve blocks in the anterolateral abdominal wall can provide regional anesthesia by infiltrating local anesthetic around the relevant nerve. As such, the transversus abdominis plane block (between the transversus abdominis and internal oblique muscles) is used to anesthetize the thoracoabdominal, iliohypogastric, and ilioinguinal nerves that run in this plane.[13] Ilioinguinal and iliohypogastric nerve blocks can also be performed by infiltrating local anesthetic superior to the anterior superior iliac spine.[14] Blocks of the anterolateral abdominal wall nerves can be used for surgeries of the abdominal or inguinal region, such as necessary in hernia repairs or trauma repair.
An indirect hernia repair may require the manipulation and visualization of the superficial inguinal ring, which puts the ilioinguinal nerve at risk. The nerve enters the inguinal canal here and can subsequently be damaged, resulting in a sensory alteration of the scrotum, root of the penis, labia major, and inner thigh.[15]
The intercostal nerves can be crushed or severed during thoracotomies. This can result in subsequent thoracoabdominal nerve dysfunction, typically causing chronic pain and rectus muscle paresis.[9][16] The placement of thoracic drains can also cause inadvertent damage to the intercostal nerves as they travel just inferior to the ribs.[17]
Surgical incisions over the anterolateral abdominal wall pose the risk of nerve damage. Depending on the location of the incision, different nerves can be affected. Pfannenstiel incisions can damage the ilioinguinal and iliohypogastric nerves, while paramedian and subcostal incisions are more likely to damage the thoracoabdominal nerves.[18][19] Incisions running perpendicular to the course of the nerves (at an anteroinferior angle) tend to correspond to a larger sensory-motor deficit.
Clinical Significance
Dysfunction of the anterolateral abdominal nerves can potentially result in abdominal weakness, hernia, chronic pain, movement impairment, sensory loss, and sexual dysfunction. Each of these factors can implicate and reduce the quality of life of an individual.[9][15][16]
Compression of the thoracoabdominal nerves most commonly occurs at the point where the nerves pierce the posterior rectus sheath, given that they turn 90 degrees to travel anteriorly through the linea semilunaris.[8] This can result in abdominal cutaneous nerve entrapment syndrome, often mistreated as gynecological pain.[8][20]
Media
(Click Image to Enlarge)

The Sympathetic Nerves. The illustration shows the right sympathetic chain and its connections with the thoracic, abdominal, and pelvic plexuses.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Jelinek LA, Scharbach S, Kashyap S, Ferguson T. Anatomy, Abdomen and Pelvis: Anterolateral Abdominal Wall Fascia. StatPearls. 2024 Jan:(): [PubMed PMID: 29083814]
Brown SH, Ward SR, Cook MS, Lieber RL. Architectural analysis of human abdominal wall muscles: implications for mechanical function. Spine. 2011 Mar 1:36(5):355-62. doi: 10.1097/BRS.0b013e3181d12ed7. Epub [PubMed PMID: 21325932]
Brown SH, Banuelos K, Ward SR, Lieber RL. Architectural and morphological assessment of rat abdominal wall muscles: comparison for use as a human model. Journal of anatomy. 2010 Sep:217(3):196-202. doi: 10.1111/j.1469-7580.2010.01271.x. Epub 2010 Jul 14 [PubMed PMID: 20646108]
Level 3 (low-level) evidenceCirocchi R,Boselli C,Renzi C,Corsi A,Cagini L,Boccolini A,Noya G,Fingerhut A, The surface landmarks of the abdominal wall: a plea for standardization. Archives of medical science : AMS. 2014 Jun 29; [PubMed PMID: 25097589]
Flament JB. [Functional anatomy of the abdominal wall]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen. 2006 May:77(5):401-7 [PubMed PMID: 16703394]
Seeras K, Qasawa RN, Ju R, Prakash S. Anatomy, Abdomen and Pelvis: Anterolateral Abdominal Wall. StatPearls. 2024 Jan:(): [PubMed PMID: 30247850]
Flynn W, Vickerton P. Anatomy, Abdomen and Pelvis: Abdominal Wall. StatPearls. 2024 Jan:(): [PubMed PMID: 31869113]
Kanakarajan S,High K,Nagaraja R, Chronic abdominal wall pain and ultrasound-guided abdominal cutaneous nerve infiltration: a case series. Pain medicine (Malden, Mass.). 2011 Mar; [PubMed PMID: 21332928]
Level 3 (low-level) evidencevan Ramshorst GH, Kleinrensink GJ, Hermans JJ, Terkivatan T, Lange JF. Abdominal wall paresis as a complication of laparoscopic surgery. Hernia : the journal of hernias and abdominal wall surgery. 2009 Oct:13(5):539-43. doi: 10.1007/s10029-009-0473-6. Epub 2009 Feb 12 [PubMed PMID: 19212701]
Level 3 (low-level) evidenceMekonen HK, Hikspoors JP, Mommen G, Köhler SE, Lamers WH. Development of the ventral body wall in the human embryo. Journal of anatomy. 2015 Nov:227(5):673-85. doi: 10.1111/joa.12380. Epub [PubMed PMID: 26467243]
Glenesk NL, Rahman S, Lopez PP. Anatomy, Thorax, Intercostal Nerves. StatPearls. 2024 Jan:(): [PubMed PMID: 30855826]
Lovering RM, Anderson LD. Architecture and fiber type of the pyramidalis muscle. Anatomical science international. 2008 Dec:83(4):294-7. doi: 10.1111/j.1447-073X.2007.00226.x. Epub [PubMed PMID: 19159363]
Level 3 (low-level) evidenceTsai HC, Yoshida T, Chuang TY, Yang SF, Chang CC, Yao HY, Tai YT, Lin JA, Chen KY. Transversus Abdominis Plane Block: An Updated Review of Anatomy and Techniques. BioMed research international. 2017:2017():8284363. doi: 10.1155/2017/8284363. Epub 2017 Oct 31 [PubMed PMID: 29226150]
Kulacoglu H, Ergul Z, Esmer AF, Sen T, Akkaya T, Elhan A. Percutaneous ilioinguinal-iliohypogastric nerve block or step-by-step local infiltration anesthesia for inguinal hernia repair: what cadaveric dissection says? Journal of the Korean Surgical Society. 2011 Dec:81(6):408-13. doi: 10.4174/jkss.2011.81.6.408. Epub 2011 Nov 25 [PubMed PMID: 22200042]
Cho HM, Park DS, Kim DH, Nam HS. Diagnosis of Ilioinguinal Nerve Injury Based on Electromyography and Ultrasonography: A Case Report. Annals of rehabilitation medicine. 2017 Aug:41(4):705-708. doi: 10.5535/arm.2017.41.4.705. Epub 2017 Aug 31 [PubMed PMID: 28971057]
Level 3 (low-level) evidenceGerner P. Postthoracotomy pain management problems. Anesthesiology clinics. 2008 Jun:26(2):355-67, vii. doi: 10.1016/j.anclin.2008.01.007. Epub [PubMed PMID: 18456219]
Level 3 (low-level) evidenceWraight WM, Tweedie DJ, Parkin IG. Neurovascular anatomy and variation in the fourth, fifth, and sixth intercostal spaces in the mid-axillary line: a cadaveric study in respect of chest drain insertion. Clinical anatomy (New York, N.Y.). 2005 Jul:18(5):346-9 [PubMed PMID: 15971216]
. Abdominal incisions in general surgery: a review. Annals of Ibadan postgraduate medicine. 2007 Dec:5(2):59-63 [PubMed PMID: 25161434]
Emrecan B, Onem G, Ocak E, Arslan M, Yagci B, Baltalarli A, Akdag B. Retroperitoneal approach via paramedian incision for aortoiliac occlusive disease. Texas Heart Institute journal. 2010:37(1):70-4 [PubMed PMID: 20200630]
Level 2 (mid-level) evidencevan Assen T, Brouns JA, Scheltinga MR, Roumen RM. Incidence of abdominal pain due to the anterior cutaneous nerve entrapment syndrome in an emergency department. Scandinavian journal of trauma, resuscitation and emergency medicine. 2015 Feb 8:23():19. doi: 10.1186/s13049-015-0096-0. Epub 2015 Feb 8 [PubMed PMID: 25887961]