Introduction
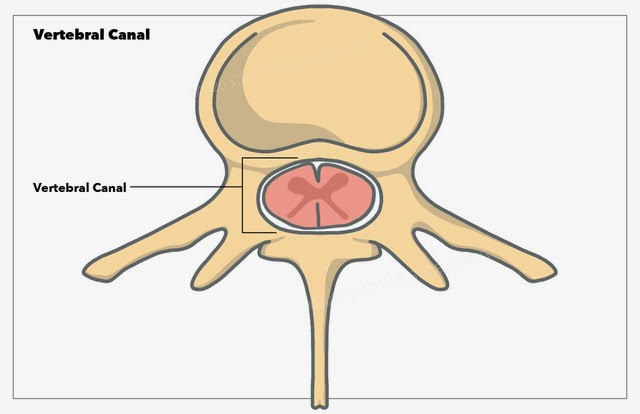
The vertebral canal, otherwise known as the vertebral cavity or spinal cavity, is an anatomical space formed by the vertebral column that stores an integral portion of the central nervous system: the spinal cord and the spinal nerve roots branching off the spinal cord bilaterally. The vertebral canal is an anatomically sterile space considered a subdivision of the dorsal body cavity, which contains the cranial cavity and the vertebral cavity/canal. The vital function of the vertebral canal is serving as a protective space for the spinal cord to traverse the length of the spinal column allowing proper innervation to the entire human body.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The vertebral canal comprises the vertebral foramen located in the cervical, thoracic, and lumbar vertebrae. The vertebral or spinal cord typically ends at the level of the L2 vertebra, where the spinal cord gives off multiple branching spinal nerves and nerve rootlets known as the cauda equina. These spinal nerves traverse at the levels of the second through the fifth lumbar vertebral levels.
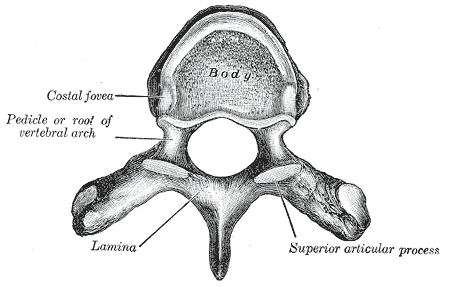
The vertebral foramen forms by the posterior portion of the vertebral body, the pedicles, the bilateral laminae, and the connection of the laminae at the transverse process. The only exceptions to this anatomical formation are the atlas and axis (C1 and C2 vertebrae), considered atypical vertebrae of the cervical spine. These two vertebrae lack a vertebral body; the atlas comprises an anterior and posterior arch, and the anatomy of the axis is made up of the odontoid process that projects superiorly into the vertebral foramen of the atlas. In addition, the transverse processes of the cervical vertebrae contain an opening - the transverse foramina (plural of foramen). The transverse foramina of C1-C6 transmit the vertebral arteries. Those of C1-C7 transmit the vertebral veins.
Two crucial structural ligaments surround the vertebral canal. These ligaments include the ligamentum flavum and the posterior longitudinal ligament. The ligamentum flavum is a ligament that traverses the entire spinal column and connects the laminae of each vertebra. The posterior longitudinal ligament runs along the posterior portion of the vertebral body, which is the anterior border of the vertebral canal.[2] The anterior longitudinal ligament connects the bodies of the vertebrae and prevents anterior dislocation of the vertebrae. It can be damaged or torn in a whiplash injury, in which violent hyperextension of the neck, as frequently seen in a rear-end automobile accident, can damage the anterior longitudinal ligament and crush the posterior portions of cervical vertebrae.[3][4]
The spinal canal diameter varies with each vertebral region, including the cervical, thoracic, and lumbar regions. The average diameter of the cervical vertebrae is 17 mm. The thoracic vertebral canal varies, with each vertebra moving in a cranial-caudal direction. Starting at the T1 vertebral level, the spinal canal diameter is 16 mm on average, and the diameter begins to decrease at the T2 level to 14 to 15 mm. The T4 vertebra has the smallest diameter moving caudally; the spinal canal diameter from T3-T11 remains relatively stable at 15 mm. At the T12 vertebra, the spinal canal diameter increases to an average of 18 mm. Compared to the cervical and thoracic regions, the lumbar vertebral group has a larger spinal canal diameter, on average, with the L5 diameter being the largest of the lumbar vertebrae at around 17.5 mm.
The spinal cord is the primary structure contained within the vertebral canal. The spinal cord gives off projections bilaterally that project out of the vertebral canal at each vertebral level. These spinal nerves contain nerve fibers from the dorsal and ventral roots of the spinal cord. The dorsal root nerves carry sensory innervation traveling back to the spinal cord from the rest of the body. The ventral roots contain motor innervation exiting from the spinal cord to travel throughout the human body.[5]
The primary and most important function of the vertebral canal is to provide a patent and protective cavity for the spinal cord to traverse from the cranium down to the sacrum. Not only does the vertebral column provide structure and support to the human body, its canal also provides physical protection for the spinal cord.
Embryology
Embryological formation of the vertebral column secondarily gives rise to the vertebral canal. During gastrulation, there are three germ layers: mesoderm, endoderm, and ectoderm. The paraxial portion of the mesoderm will ultimately differentiate into forty-two pairs of segments, somites, that develop in a cephalocaudal direction during embryological development. The somites will further develop into dermatomyotomes and sclerotomes. The sclerotomes will later develop into the bony structure of the human spine.[6]
The ossification and development of the individual vertebrae that comprise the vertebral column allow the vertebrae to form a foramen through which the spinal cord traverses. Vertebral ossification is very specific, and it includes eight different ossification centers: three primary centers and five secondary centers. The primary centers include the bilateral neural processes and the centrum of the vertebrae. The secondary ossification centers include the transverse process tips, the tip of the spinous process, and the superior and inferior surfaces of the vertebral body.[6]
Blood Supply and Lymphatics
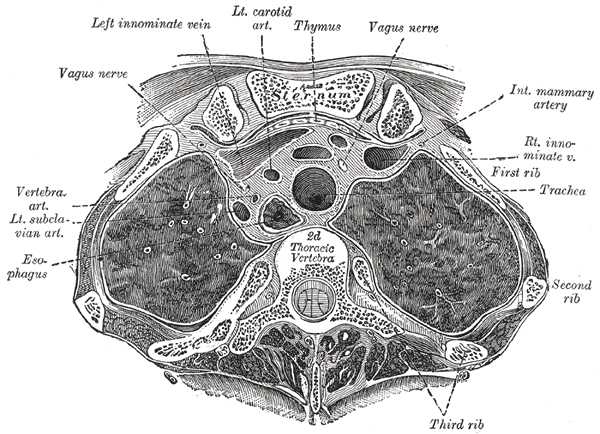
The spinal cord that travels through the vertebral canal primarily receives its blood supply from two sources: the anterior spinal artery and the two posterior spinal arteries. As these two arteries traverse the length of the spinal column, they give off branching arteries bilaterally at each vertebral level. These branching arteries are the segmental spinal arteries that enter the vertebral canal through the intervertebral foramina. Spinal branches feed the vertebral column at all segmental levels. These are derived from several arteries, beginning with the vertebral and ascending cervical arteries and continuing with the posterior intercostal arteries, subcostal, lumbar, iliolumbar, lateral sacral, and medial sacral arteries. Venous drainage occurs via the internal and external plexuses.[7][8][1][8]
The artery of Adamkiewicz, otherwise known as the great anterior radiculomedullary artery, is a perfusing branch of the radicular anterior artery arising from the posterior intercostal artery. There are multiple anatomic variants of this artery and at what vertebral level it joins with the anterior spinal artery.[9]
Nerves
The vertebral canal contains the spinal cord, from which 31 pairs of spinal nerves arise. These spinal nerves control motor, sensory, and other functions.
Innervation of the vertebrae is by the recurrent meningeal branches. These arise from the mixed spinal nerve, formed by the union of the posterior (dorsal) spinal root, which is sensory, and the anterior (ventral) spinal root, which is motor. The sensory neurons have cell bodies in the posterior (dorsal) root ganglia, whereas the anterior (ventral) neurons have cell bodies in the anterior gray horn. Two to four recurrent meningeal branches in each right and left mixed spinal nerve supply sensation for the vertebrae. Motor functions reside in the paraspinal muscles (erector spinae).
Clinical Significance
VACTERL syndrome is a multi-factorial condition affecting the embryological development of multiple organ systems. One of those systems is the skeletal system and, more specifically, the vertebral column. This condition can lead to skeletal malformations such as missing, fused, or even extra vertebrae present in the spine that can compromise the spinal cord due to variations in the size of the vertebral canal in which the spinal cord resides.[10]
Spondylolisthesis occurs when a vertebral body slips anteriorly relative to the inferior vertebral body. This condition can arise from a congenital malformation of the lumbosacral joint L5-S1, or it can more commonly occur in people who repetitively hyperextend and rotate their movements—this is why spondylolisthesis most commonly presents in gymnastics, swimming, diving, and weightlifting populations. If the anterior slippage is severe, typically less than 50% displacement of the superior vertebra concerning its inferior vertebra, there can be neurological deficits present due to compression of the spinal cord resulting from a reduction in the vertebral canal space. Spondylolisthesis can also be associated with spondylolysis, a bilateral fracture of the pars interarticularis portion of the vertebra. When this occurs, the stabilization of the vertebral column is compromised, and the vertebral body can now slip anteriorly.[11][12]
Disc herniation is when the nucleus pulposus portion of the intervertebral disc herniates through the weakened annular fibrosis fibers of the outer disc, causing compression of the spinal cord and the spinal nerve roots. Annular fiber weakening is associated with degenerative disc disease.[13] Multiple types of disc herniations exist, including protrusion, extrusion, and sequestration. One way to differentiate between disc protrusion and extrusion is the ratio of the length of the apex of the herniated disc compared to the length of the base of the herniated disc portion. Disc protrusion is when the base length is greater than the length of the herniated disc apex, and for extrusion, the length of the herniated apex is greater than the base of the herniated portion of the disc. Disc sequestration occurs when a herniated portion of the nucleus pulposus portion of an intervertebral disc fragment from the disc becomes a free-floating segment within the spinal canal, allowing it to migrate caudally or cranially.[14][15]
Spinal stenosis occurs when there is a narrowing of the spinal canal that results in spinal cord compression. Multiple etiologies of spinal stenosis exist and include degenerative bone diseases such as osteoarthritis, rheumatoid arthritis, and Paget disease; the latter potentially leads to bony overgrowth due to dysregulation of osteoblast and osteoclast activity. Due to the stenotic process, neurovascular compression can lead to neurological pain symptoms that can be debilitating depending on the severity and patient tolerance.[16][17]
Several abnormal spinal curvatures can rise to the level of clinical significance. The upper thoracic region normally has a curvature with the concave surface facing anteriorly. When exaggerated, this forms a kyphosis, characterized by the posterior surface being convex and the anterior surface being concave. The most common cause of this is osteoporosis, which is usually most severe in the post-menopausal female due to decreased serum estrogen levels.[18][19]
Lordosis is an exaggeration of the normal lumbar curvature in which the anterior surface is convex, and the posterior surface is concave. This curvature is exaggerated in pregnancy due to the anatomical changes needed to accommodate a growing fetus. This is a normal development. However, this curvature is exaggerated in osteomalacia or muscle weakness; the condition is termed lordosis.[20][21][19]
Lateral curvature of the vertebral column is termed scoliosis. This condition is usually developmental in origin. It can result from abnormal growth of the vertebral column, vertebral damage or erosion, or abnormalities of the vertebral muscles.[22][23][24]
In the pelvic region, the deep dorsal vein of the penis and the prostate venous plexus communicates with the vertebral venous plexuses, accounting for the spread of prostate cancer into the bodies of the lumbar vertebrae. These lesions are especially painful, as bone has a rich innervation for pain sensation.
Any fracture of the atlas is a potentially dangerous condition. This is because the transverse ligament of the atlas is stronger than the dens, which is most commonly fractured at its base. Such a fracture can cause loss of blood supply to the dens, causing it to undergo avascular necrosis, in which the structure dies due to loss of its blood supply. This is why supporting the neck at an accident site is essential before transporting the patient.
Media
(Click Image to Enlarge)
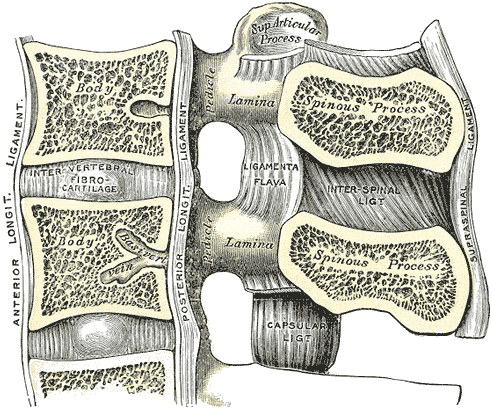
Lumbar Vertebral Anatomy. This medial sagittal section shows the relationship between the anterior longitudinal ligament, vertebral bodies, intervertebral fibrocartilage, posterior longitudinal ligament, vertebral laminae, ligamenta flava, superior articular processes, pedicles, spinous processes, interspinal ligament, capsular ligament, and supraspinal ligament.
Gray's Anatomy
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Longatti P, Fiorindi A, Marton E, Sala F, Feletti A. Where the central canal begins: endoscopic in vivo description. Journal of neurosurgery. 2022 Mar 1:136(3):895-904. doi: 10.3171/2020.12.JNS203649. Epub 2021 Aug 13 [PubMed PMID: 34388726]
DeSai C, Reddy V, Agarwal A. Anatomy, Back, Vertebral Column. StatPearls. 2023 Jan:(): [PubMed PMID: 30247844]
Chen HB, Yang KH, Wang ZG. Biomechanics of whiplash injury. Chinese journal of traumatology = Zhonghua chuang shang za zhi. 2009 Oct:12(5):305-14 [PubMed PMID: 19788851]
Sarrami P,Armstrong E,Naylor JM,Harris IA, Factors predicting outcome in whiplash injury: a systematic meta-review of prognostic factors. Journal of orthopaedics and traumatology : official journal of the Italian Society of Orthopaedics and Traumatology. 2017 Mar; [PubMed PMID: 27738773]
Level 1 (high-level) evidenceBasit H, Reddy V, Varacallo M. Anatomy, Back, Spinal Nerve-Muscle Innervation. StatPearls. 2023 Jan:(): [PubMed PMID: 30855906]
Kalamchi L, Valle C. Embryology, Vertebral Column Development. StatPearls. 2023 Jan:(): [PubMed PMID: 31751107]
Devereaux MW. Anatomy and examination of the spine. Neurologic clinics. 2007 May:25(2):331-51 [PubMed PMID: 17445732]
Colman MW, Hornicek FJ, Schwab JH. Spinal Cord Blood Supply and Its Surgical Implications. The Journal of the American Academy of Orthopaedic Surgeons. 2015 Oct:23(10):581-91. doi: 10.5435/JAAOS-D-14-00219. Epub 2015 Sep 16 [PubMed PMID: 26377671]
Lindeire S, Hauser JM. Anatomy, Back, Artery Of Adamkiewicz. StatPearls. 2023 Jan:(): [PubMed PMID: 30422566]
Solomon BD. The etiology of VACTERL association: Current knowledge and hypotheses. American journal of medical genetics. Part C, Seminars in medical genetics. 2018 Dec:178(4):440-446. doi: 10.1002/ajmg.c.31664. Epub [PubMed PMID: 30580478]
Daniels JM, Arguelles C, Gleason C, Dixon WH. Back Injuries. Primary care. 2020 Mar:47(1):147-164. doi: 10.1016/j.pop.2019.10.008. Epub 2019 Oct 17 [PubMed PMID: 32014131]
Shamrock AG, Donnally III CJ, Varacallo M. Lumbar Spondylolysis And Spondylolisthesis. StatPearls. 2023 Jan:(): [PubMed PMID: 28846329]
Sharrak S, Al Khalili Y. Cervical Disc Herniation. StatPearls. 2023 Jan:(): [PubMed PMID: 31536225]
De Cicco FL, Camino Willhuber GO. Nucleus Pulposus Herniation. StatPearls. 2023 Jan:(): [PubMed PMID: 31194447]
Dydyk AM, Khan MZ, Singh P. Radicular Back Pain. StatPearls. 2023 Jan:(): [PubMed PMID: 31536200]
Wu L, Cruz R. Lumbar Spinal Stenosis. StatPearls. 2023 Jan:(): [PubMed PMID: 30285388]
Munakomi S, Foris LA, Varacallo M. Spinal Stenosis and Neurogenic Claudication. StatPearls. 2023 Jan:(): [PubMed PMID: 28613622]
Solla F, Clément JL, Cunin V, Bertoncelli CM, Fière V, Rampal V. Patient-specific rods for thoracic kyphosis correction in adolescent idiopathic scoliosis surgery: Preliminary results. Orthopaedics & traumatology, surgery & research : OTSR. 2020 Feb:106(1):159-165. doi: 10.1016/j.otsr.2019.07.027. Epub 2019 Nov 19 [PubMed PMID: 31757655]
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A. Sagittal balance of the spine. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2019 Sep:28(9):1889-1905. doi: 10.1007/s00586-019-06083-1. Epub 2019 Jul 22 [PubMed PMID: 31332569]
Shepherd A, James SS, Rengan R. The Practicality of ICRU and Considerations for Future ICRU Definitions. Seminars in radiation oncology. 2018 Jun:28(3):201-206. doi: 10.1016/j.semradonc.2018.02.005. Epub [PubMed PMID: 29933880]
Berven S, Wadhwa R. Sagittal Alignment of the Lumbar Spine. Neurosurgery clinics of North America. 2018 Jul:29(3):331-339. doi: 10.1016/j.nec.2018.03.009. Epub [PubMed PMID: 29933801]
Shakil H, Iqbal ZA, Al-Ghadir AH. Scoliosis: review of types of curves, etiological theories and conservative treatment. Journal of back and musculoskeletal rehabilitation. 2014:27(2):111-5. doi: 10.3233/BMR-130438. Epub [PubMed PMID: 24284269]
Vialle R, Thévenin-Lemoine C, Mary P. Neuromuscular scoliosis. Orthopaedics & traumatology, surgery & research : OTSR. 2013 Feb:99(1 Suppl):S124-39. doi: 10.1016/j.otsr.2012.11.002. Epub 2013 Jan 19 [PubMed PMID: 23337438]
Mackel CE, Jada A, Samdani AF, Stephen JH, Bennett JT, Baaj AA, Hwang SW. A comprehensive review of the diagnosis and management of congenital scoliosis. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2018 Nov:34(11):2155-2171. doi: 10.1007/s00381-018-3915-6. Epub 2018 Aug 4 [PubMed PMID: 30078055]