Introduction
The spinal cord and brain are encased within three layers of tissue called the meninges. The spinal meninges specifically enclose the spinal cord and stretch from the brainstem down to the filum terminale. The layers of the meninges are, from deep to superficial, the pia mater, the arachnoid mater, and the dura mater. The names of these layers give information regarding their qualities. Pia, which is Latin for “loving,” and mater, which is Latin for “mother,” make up the pia mater, or “loving mother,” which is directly attached to the spinal cord and inseparable. The arachnoid mater contains a web of fiber beneath it in the subarachnoid space, and the dura mater or “hard mother” is the tough outer layer of the meninges. The principal function of the spinal meninges is to protect and support the spinal cord.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The Epidural Space
Between the ligamentum flavum and the superficial dura mater is the spinal epidural space. This location contains various structures such as adipose tissue, connective tissue, nerves, the internal vertebral venous plexus, and lymphatics. It is a site commonly used for analgesic purposes and is a potential site for infection.[1][2]
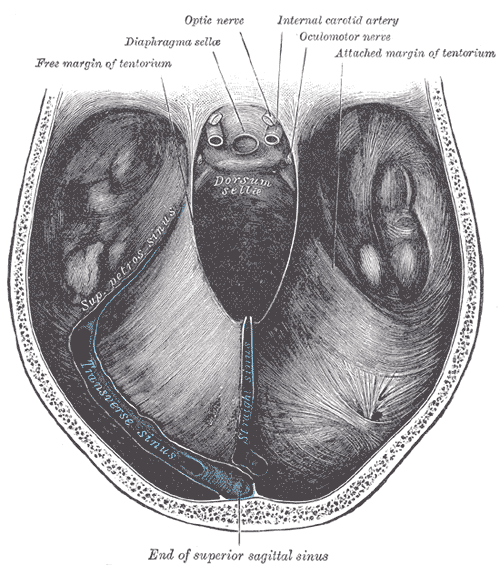
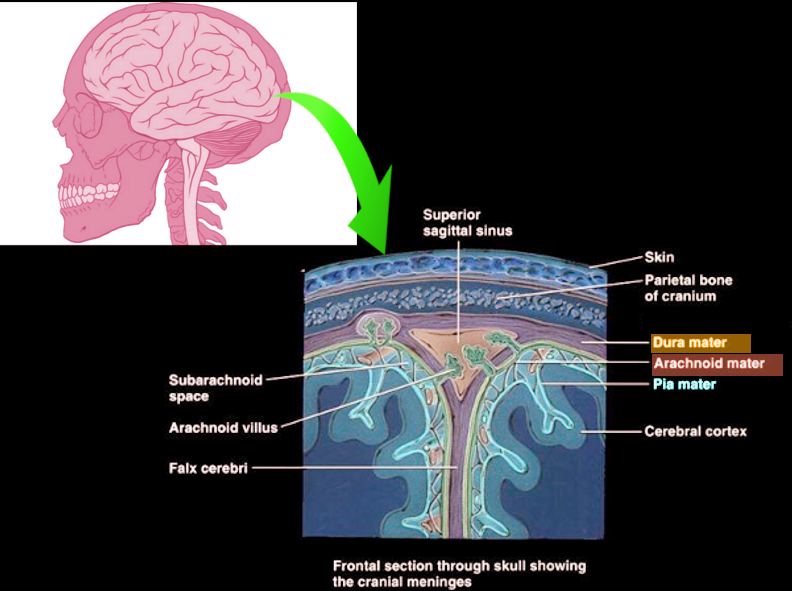
The Dura Mater
The most superficial layer of the meninges is the dura mater. While it has two layers in the cranial segment, the spinal dura mater only has the deep meningeal layer. The periosteal layer, which is the superficial layer of the dura within the calvarium, ends at the foramen magnum, with only the meningeal layer continuing down along the spinal cord.[1] The dura mater is the strongest of the three layers, with some animal studies showing that the thickness of the dura decreases as it descends towards the coccyx.[3] As they make their way out of the vertebral canal, the spinal nerves are coated with dura mater as they exit into the epidural space, creating the epineurium.
The Subdural Space
The spinal subdural space is only a potential space; typically, it is not present under normal physiological conditions. It exists between the dura and arachnoid mater.[1]
The Arachnoid Mater
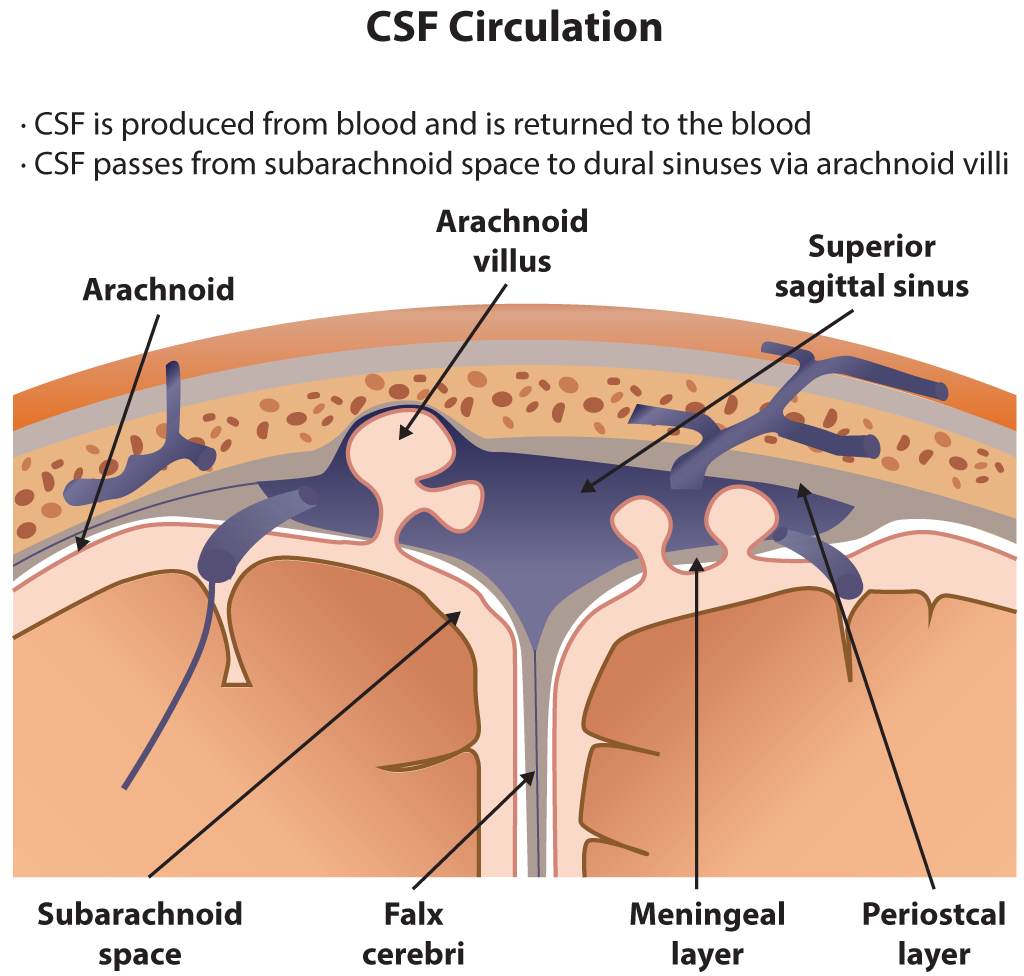
The spinal arachnoid mater is between the dura and the pia mater. The arachnoid mater is avascular and primarily exists to help maintain cerebrospinal fluid (CSF) metabolism.[4]
The Subarachnoid Space
The spinal subarachnoid space is located between the arachnoid and pia mater and is filled with CSF. Arachnoid trabeculae extend between these two layers within the subarachnoid space to give the subarachnoid space its characteristic spiderweb appearance. The choroid plexus produces CSF within the brain ventricles, and CSF enters the spinal subarachnoid spaces via the median and lateral apertures. The functions of the CSF include protection and nourishment of the brain and spinal cord.[4] The spinal subarachnoid space, specifically the lumbar cistern inferior to the conus medullaris, has clinical significance in diagnosing meningitis, as it is the site of lumbar puncture.
The Pia Mater
The spinal pia mater is the deepest layer of the meninges and is directly attached to the surface of the spinal cord. The pia mater is composed primarily of collagen and reticular fibers.[5] The pia mater will continue past the conus medullaris and fuse into the filum terminale, anchoring the spinal cord to the coccyx inferiorly. One of the main functions of the spinal pia mater is that it has important elastic qualities that help maintain the stiffness of the spinal cord, and it assists the cord return to its original shape after compression.[6] The spinal pia mater also contains denticulate ligaments, which extend outwards to help anchor the spinal cord to the spinal dura mater, further assisting with stabilizing the cord.[7]
Embryology
The spinal meninges, along with the cranial meninges, have a complex embryologic origin. The pia and arachnoid mater, collectively known as the leptomeninges, are derived from the neural crest. The neural crest itself forms from the ectoderm-derived neuroectoderm and neural plate. The dura mater derives from the mesoderm.[4][8]
Blood Supply and Lymphatics
The blood supply to the spinal meninges comes primarily from the anterior and posterior spinal arteries. The single anterior spinal artery originates from the vertebral arteries, which each gives of collaterals that fuse and descend as the anterior spinal artery before becoming the basilar artery. The paired posterior spinal arteries also receive their blood supply from the vertebral arteries. Additional segmental medullary arteries also feed into these anterior and posterior spinal arteries via entrance points at the nerve roots, the largest being the artery of Adamkiewicz, which provides additional blood supply to the anterior spinal artery and is typically present between T9 and L2.[9][10]
The venous drainage of the spinal meninges is through the internal and external vertebral venous plexuses. These form a complex and valve-less system of drainage that is continuous with the venous system of the brain and has drainage into the azygos venous system, the portal venous system, renal veins, and the superior and inferior vena cava, among others.[11]
Nerves
The spinal meninges have significant nonspecific innervation, including both sensory and sympathetic fiber. Abundant sympathetic nerve fibers with strong associations to blood vessels are present within all three layers of the meninges.[12][13] Additionally, the peridural membrane has abundant sensory and nociceptive innervations, which likely play a role in back pain.[14]
Surgical Considerations
There are many tumors of the spinal meninges, one example being a meningioma. While the majority of meningiomas appear in the cranial meninges, they are also known to grow in the spinal portions, especially in the thoracic and cervical portions. Spinal meningiomas are typically benign and slow-growing and typically occur in women aged 50 to 70. Children with neurofibromatosis type 2 are also susceptible to developing spinal cord tumors, such as meningiomas and intramedullary tumors.[15][16]
The more common tumors that impact the spinal meninges are epidural metastases, which can primarily arise from breast, lung, and prostate primary cancers. These metastases can grow on either the bony vertebra, the paravertebral tissues, or within the epidural space overlying the spinal meninges. These metastases are most common in the thoracic region and can cause significant compression of the spinal cord or cauda equina syndrome if in the lumbar-sacral region.[17]
Clinical Significance
Clinically, the spinal meninges are important for their role in the spread of cancers and diagnosing of meningitis. The spinal epidural space contains a system of epidural veins known as the Batson plexus, which appears to carry implications for the spread of various infections and metastatic cancer, such as prostate cancer, resulting in the metastatic epidural masses described earlier.[1][17] Compression of the spinal cord by tumors of the meninges and epidural space can cause a plethora of neurological symptoms, such as motor weakness, upper motor signs (i.e., positive Babinski reflex), urinary incontinence, and pain.[17]
Clinicians utilize the spinal subarachnoid space when performing a diagnostic lumbar puncture, which may be useful in assessing the presence of meningitis, a subarachnoid bleed, or recording the opening pressure of CSF. A lumbar puncture is among the first tests performed when a patient presents with the cardinal features of meningitis (headache, fever, and nuchal rigidity). In adults, the L3/L4 interspinal space is the preferred location to collect the CSF from the lumbar cistern safely. The L4 spinous process is roughly midline at the level of the iliac crests, known as the intercristal or Tuffier line, making the L3/L4 interspinal space just above this landmark.
The patient should then be in either the left lateral decubitus position or seated with the spine flexed. The needle should be inserted with the bevel parallel to the fibers of the dura mater (up or down if left lateral decubitus and bevel to either the right or left if seated position, to reduce resistance when passing through the meninges and avoid harming any fibers of the cauda equina) into the L3/L4 interspinal space at a slight angle. The needle will then pass through the following structures: skin, subcutaneous tissue, the supraspinous ligament, the interspinous ligament, the ligamentum flavum, the epidural space, the dura mater, the arachnoid mater, and the subarachnoid space/lumbar cistern. The patient should receive counsel to expect common side effects such as headache, which occurs in a third of all cases, and pain is often relieved when lying supine.[18]
Anesthesia during childbirth can also be delivered using the same landmarks as placing a lumbar puncture needle. An epidural anesthetic would be placed in the epidural space, while the placement of spinal anesthesia will be within the CSF of the lumbar cistern. Epidurals are typically more precise but have a longer onset of action and require a larger dose than spinal anesthesia. Levobupivacaine and bupivacaine are two commonly used agents for epidural and spinal anesthesia.[19]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
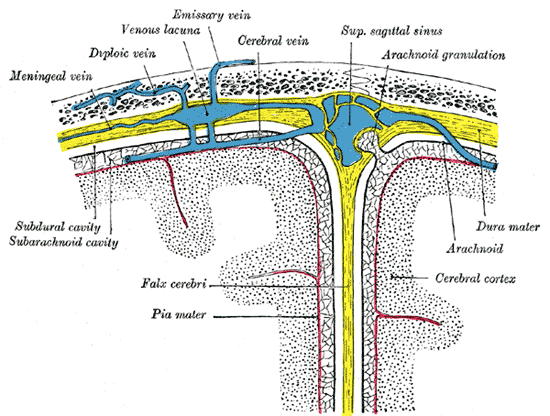
Diagrammatic Cross Section the top of the skull, showing the membranes of the brain, Meningeal vein, Diploic vein, Venous lacuna, Emissary vein, Cerebral vein, Superior sagittal sinus, Arachnoid granulation, Subdural cavity, Subarachnoid cavity, Falx cerebri, Pia mater, Dura mater, Arachnoid, Cerebral cortex
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Bican O, Minagar A, Pruitt AA. The spinal cord: a review of functional neuroanatomy. Neurologic clinics. 2013 Feb:31(1):1-18. doi: 10.1016/j.ncl.2012.09.009. Epub [PubMed PMID: 23186894]
Elsharkawy H, Sonny A, Chin KJ. Localization of epidural space: A review of available technologies. Journal of anaesthesiology, clinical pharmacology. 2017 Jan-Mar:33(1):16-27. doi: 10.4103/0970-9185.202184. Epub [PubMed PMID: 28413269]
Yang C, Yang X, Lan X, Zhang H, Wang M, Zhang Y, Xu Y, Zhen P. [Structure and mechanical characteristics of spinal dura mater in different segments of sheep's spine]. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi = Chinese journal of reparative and reconstructive surgery. 2019 Feb 15:33(2):232-238. doi: 10.7507/1002-1892.201807085. Epub [PubMed PMID: 30739422]
Ghannam JY, Al Kharazi KA. Neuroanatomy, Cranial Meninges. StatPearls. 2023 Jan:(): [PubMed PMID: 30969704]
Nam MH, Baek M, Lim J, Lee S, Yoon J, Kim J, Lee MS, Soh KS. Discovery of a novel fibrous tissue in the spinal pia mater by polarized light microscopy. Connective tissue research. 2014 Apr:55(2):147-55. doi: 10.3109/03008207.2013.879864. Epub [PubMed PMID: 24409813]
Level 3 (low-level) evidenceOzawa H, Matsumoto T, Ohashi T, Sato M, Kokubun S. Mechanical properties and function of the spinal pia mater. Journal of neurosurgery. Spine. 2004 Jul:1(1):122-7 [PubMed PMID: 15291032]
Level 3 (low-level) evidenceCeylan D, Tatarlı N, Abdullaev T, Şeker A, Yıldız SD, Keleş E, Konya D, Bayri Y, Kiliç T, Çavdar S. The denticulate ligament: anatomical properties, functional and clinical significance. Acta neurochirurgica. 2012 Jul:154(7):1229-34. doi: 10.1007/s00701-012-1361-x. Epub 2012 May 4 [PubMed PMID: 22555553]
O'Rahilly R, Müller F. The meninges in human development. Journal of neuropathology and experimental neurology. 1986 Sep:45(5):588-608 [PubMed PMID: 3746345]
N'da HA, Chenin L, Capel C, Havet E, Le Gars D, Peltier J. Microsurgical anatomy of the Adamkiewicz artery-anterior spinal artery junction. Surgical and radiologic anatomy : SRA. 2016 Jul:38(5):563-7. doi: 10.1007/s00276-015-1596-3. Epub 2015 Dec 1 [PubMed PMID: 26627692]
Kunam VK, Velayudhan V, Chaudhry ZA, Bobinski M, Smoker WRK, Reede DL. Incomplete Cord Syndromes: Clinical and Imaging Review. Radiographics : a review publication of the Radiological Society of North America, Inc. 2018 Jul-Aug:38(4):1201-1222. doi: 10.1148/rg.2018170178. Epub [PubMed PMID: 29995620]
Tobinick E, Vega CP. The cerebrospinal venous system: anatomy, physiology, and clinical implications. MedGenMed : Medscape general medicine. 2006 Feb 22:8(1):53 [PubMed PMID: 16915183]
BRIDGE CJ. Innervation of spinal meninges and epidural structures. The Anatomical record. 1959 Mar:133(3):553-63 [PubMed PMID: 13670446]
Yamada H, Honda T, Yaginuma H, Kikuchi S, Sugiura Y. Comparison of sensory and sympathetic innervation of the dura mater and posterior longitudinal ligament in the cervical spine after removal of the stellate ganglion. The Journal of comparative neurology. 2001 May 21:434(1):86-100 [PubMed PMID: 11329131]
Level 3 (low-level) evidenceBosscher HA, Heavner JE, Grozdanov P, Warraich IA, Wachtel MS, Dertien J. The Peridural Membrane of the Human Spine is Well Innervated. Anatomical record (Hoboken, N.J. : 2007). 2016 Apr:299(4):484-91. doi: 10.1002/ar.23315. Epub 2016 Jan 30 [PubMed PMID: 26861845]
Kunimatsu A, Kunimatsu N, Kamiya K, Katsura M, Mori H, Ohtomo K. Variants of meningiomas: a review of imaging findings and clinical features. Japanese journal of radiology. 2016 Jul:34(7):459-69. doi: 10.1007/s11604-016-0550-6. Epub 2016 May 2 [PubMed PMID: 27138052]
Kushel' YV, Belova YD, Tekoev AR. [Intramedullary spinal cord tumors and neurofibromatosis]. Zhurnal voprosy neirokhirurgii imeni N. N. Burdenko. 2017:81(1):70-73. doi: 10.17116/neiro201780770-73. Epub [PubMed PMID: 28291216]
Yáñez ML, Miller JJ, Batchelor TT. Diagnosis and treatment of epidural metastases. Cancer. 2017 Apr 1:123(7):1106-1114. doi: 10.1002/cncr.30521. Epub 2016 Dec 27 [PubMed PMID: 28026861]
Doherty CM, Forbes RB. Diagnostic Lumbar Puncture. The Ulster medical journal. 2014 May:83(2):93-102 [PubMed PMID: 25075138]
Cheng Q, Zhang W, Lu Y, Chen J, Tian H. Ropivacaine vs. levobupivacaine: Analgesic effect of combined spinal-epidural anesthesia during childbirth and effects on neonatal Apgar scores, as well as maternal vital signs. Experimental and therapeutic medicine. 2019 Sep:18(3):2307-2313. doi: 10.3892/etm.2019.7776. Epub 2019 Jul 16 [PubMed PMID: 31410181]