Introduction
The forearm is the section of the upper limb from the elbow to the wrist, whose bony structure is formed by the radius (laterally) and ulna (medially). Two muscular compartments - an anterior (flexor) and posterior (extensor) compartment - contain together twenty muscles that act on the elbow and wrist joints, as well as carpometacarpal, metacarpophalangeal, and interphalangeal joints of the hand. Thus, the forearm muscles are essential to the fine motor actions of the upper limb, allowing for complex movements of the arm, wrist, and fingers.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The forearm muscles are broadly divided into two compartments: the anterior flexor compartment and the posterior extensor compartment. Fascial layers define the boundaries of these compartments within the forearm. The deep fascia of the forearm encircles the musculature related to the ulna and radius. Dividing the compartments are the intermuscular septum, which originates from the anterior aspect of the radius, and is continuous with the deep fascia of the forearm, and the interosseus membrane, which forms between the radius and ulna[1].
The muscles of the forearm or antebrachium work together to move the elbow, forearm, wrist, and digits of the hand. They fall into two categories: intrinsic and extrinsic muscles. The intrinsic muscles function to move the forearm by pronating and supinating the radius and ulna. The extrinsic muscles flex and extend the digits of the hand. One muscle, the brachioradialis, traverses the elbow joint, running from the arm to the wrist, helping to flex the elbow.
Embryology
The skeletal muscles of the limbs are formed from myoblasts that migrate to the developing bones after epitheliomesenchymal transformation. During this transformation, the somatic mesoderm of the ventral somite responds to molecular signals causing migration to the developing limb bud. Once the cells have moved to their final location, the notochord and neural tube release peptides that induce further migration and growth.
Blood Supply and Lymphatics
As the brachial artery runs down the arm and passes through the elbow, it divides into two terminal branches: the radial artery and the ulnar artery. These two arteries provide the blood supply for the entire forearm and hand.
The radial artery gives off the recurrent radial branch just distal to the radial head and traverses back up to the arm to form an anastomosis with the radial collateral of the deep brachial artery. The recurrent radial branch provides blood to the supinator and the brachioradialis muscle. The radial artery then continues down through the forearm to the wrist, where it wraps posteriorly before diving into the hand.
Similarly, the ulnar artery gives off two recurrent branches, the anterior and posterior, as it passes the elbow. These two turn upward and create anastomoses with the inferior and superior collateral arteries that branch off the deep brachial artery. The anterior ulnar recurrent artery provides blood to the pronator teres and brachialis, while the posterior ulnar recurrent artery provides blood supply to the proximal portions of the flexor muscles, bones, and elbow joint. After giving off the recurrent branches, the ulnar artery gives rise to the common interosseous branch, which will continue to divide into the anterior and posterior interosseous arteries. The names of these arteries denote which side of the interosseous membrane they run on. The anterior interosseous branch supplies blood to the muscles of the flexor compartment. As it travels down the forearm, it will eventually pierce the interosseous membrane and anastomose with the posterior interosseous artery, which is the blood supply for the extensor compartment of the forearm[2].
The venous system for the forearm comprises superficial and deep veins. The deep veins compose a plexus that run with the arteries described above. The major superficial veins include the basilic vein (running on the medial side of the forearm), the cephalic vein (running on the lateral side of the forearm), and the median vein (running up the forearm to the median antecubital vein and draining the hand).
Nerves
The three main nerves of the forearm are the median, ulnar, and radial nerves. There are also three nerves that innervate the skin (medial, lateral, and posterior cutaneous nerves). All of these nerves branch from the brachial plexus in the axillary region of the arm and traverse down the upper extremity to the hand. The median and ulnar nerve provide the innervation for the muscles of the flexor compartment, while the radial nerve provides innervation for the extensor compartment.
The median nerve gives off one main branch known as the anterior interosseous nerve. It innervates the flexor pollicis longus, part of the flexor digitorum profundus, and gives off multiple muscular branches that go directly to the muscles of the flexor compartment. The ulnar nerve does not have any terminal branches until it reaches the hand, but it does give off muscular branches as it goes down the forearm that will supply the flexor carpi ulnaris and the medial side of the flexor digitorum profundus. The radial nerve gives off the posterior interosseous nerve, which supplies all of the muscles in the posterior compartment except anconeus, brachioradialis, and extensor carpi radialis longus.[1]
Muscles
There are twenty muscles of the forearm, divided between the anterior (flexor) and posterior (extensor) compartments; each compartment is further divided into superficial and deep compartments.[1][3]
The superficial part of the flexor surface of the forearm contains five muscles:
- Pronator teres
- Flexor carpi radialis longus
- Palmaris longus
- Flexor carpi ulnaris
- Flexor digitorum superficialis
All of these muscles originate primarily from the medial epicondyle of the humerus, also known as the common flexor origin. The final attachment site for the pronator teres is the middle portion of the radius, forming the medial border of the cubital fossa. The flexor carpi radialis and flexor carpi ulnaris insert on the bases of the second, third, and fifth metacarpals, respectively.[4] The flexor carpi ulnaris achieves its distal insertion at the fifth metacarpal by inserting onto the pisiform bone and the neighboring pisohamate and pisometacarpal ligaments. The flexor digitorum superficialis crosses the wrist through the carpal tunnel and inserts at the proximal interphalangeal joint at the base of the middle phalanx of digits two through five. The tendon of each digit splits into two just before insertion into the anteromedial and anteromedial middle phalanx, allowing the tendon of flexor digitorum profundus to pass through and insert further distally.
The deep part of the flexor surface of the forearm contains three muscles:
- Pronator quadratus
- Flexor digitorum profundus
- Flexor pollicis longus
Flexor digitorum profundus originates on the proximal three-fourths of the ulna and from the interosseous membrane. Its tendons pass through the carpal tunnel[5] to insert into the bases of their respective distal phalanges, passing between the divided distal superficial flexor tendons. The flexor pollicis longus originates from the surface of the anterior radius above the origin of the pronator quadratus, and its tendon also passes through the carpal tunnel to insert into the base of the distal phalanx of the thumb[6]. The pronator quadratus originates on the distal anteromedial ulna and inserts into the distal anterolateral radius. It allows for pronation of the forearm.
The superficial part of the extensor compartment of the forearm contains seven muscles:
- Brachioradialis
- Extensor carpi radialis brevis
- Extensor carpi radialis longus
- Extensor carpi ulnaris
- Extensor digitorum
- Extensor digiti minimi
- Anconeus
Brachioradialis and extensor carpi radialis longus arises from the lateral supracondylar ridge of the humerus. The other muscles of the superficial extensor compartment arise from the lateral epicondyle of the humerus, otherwise known as the common extensor origin. Brachioradialis inserts distally to the flexor side of the wrist at the base of the radial styloid.[7] The extensor carpi radialis longus, radialis brevis, and ulnaris attach to the proximal portion of the second, third, and fifth metacarpals, respectively. The extensor carpi ulnaris The tendons of the extensor digitorum run under the extensor retinaculum and divide to attach to the extensor hoods of the middle and distal phalanx of each of the digits two through five. It does this by splitting into three slips. The middle slip attaches to the base of the middle phalanx of each digit, and the collateral slips converge distally and insert at the base of the distal phalanx of each digit. The extensor digiti minimi runs along with the extensor digitorum and inserts into the extensor hood of the fifth metacarpal. Finally, the anconeus is a small muscle arising from the common extensor origin and inserting onto the lateral olecranon and upper ulna.
The deep part of the extensor compartment of the forearm contains five muscles:
- Abductor pollicis longus
- Extensor pollicis longus
- Extensor pollicis brevis
- Extensor indicis
- Supinator
Three of the muscles originate from the ulna: the abductor pollicis longus, extensor pollicis longus, and extensor indicis. These three muscles extend into the dorsum of the hand and attach to the digits. The abductor pollicis longus connects at the base of the first metacarpal and to the trapezium of the wrist. The extensor pollicis longus runs along the forearm to the wrist, where it makes a sharp turn at Lister’s tubercle and finally attaches to the distal phalanx of the thumb. Extensor indicis runs with the extensor digitorum tendon and joins the second digit at the extensor hood. Extensor pollicis brevis and the supinator originate from the radius. Extensor pollicis brevis runs with the abductor in the forearm and connects to the base of the proximal phalanx of the first digit. The supinator is unique because it starts on the lateral epicondyle of the humerus along with the radius before wrapping around the back of the arm to connect to the radius at the same location at pronator teres. This muscle allows for the supination of the forearm.[8]
Physiologic Variants
There are multiple physiological variants of these muscles. Many of them are a function of where the muscles originate or insert. Some variations include the muscles not being present, which is especially true for the palmaris longus, considered a vestigial structure as approximately 14% of the population has a unilateral or bilateral absence of this muscle.[9][10]
As with any nerve, artery, or vein, the path it takes and its specific supply is based on the growth pattern of the individual. One of the main variations in the nerves is the Martin-Gruber connection, which forms in the forearm when the median nerve sends a branch to join with the ulnar nerve as it passes deep to the flexor digitorum superficialis. This occurs in approximately 17% of the population and leads to some median nerve innervations in the intrinsic muscles of the hand.[11]
Surgical Considerations
Compartment syndrome can be a limb-threatening emergency. This syndrome occurs when swelling of the area compresses the vessels and nerves in the region. The most common cause is fractures of the bones of the forearm. Signs and symptoms of this condition are pain out of proportion to exam findings, pallor, paresthesias, pulselessness, and paralysis. The examiner should evaluate compartment pressures if compartment syndrome is on the differential. A pressure between 30 to 45 mmHg indicates compartment syndrome. If the patient has unequivocally positive findings on physical exam, surgical management before confirmation with compartment pressures may be an option. The procedure of choice to relieve compartment syndrome is a fasciotomy, a surgical procedure where the skin and fascia are cut to open all compartments of the forearm to release the tension created by the swelling.[12][13]
The space of Parona lies between the long flexor tendons and the deep pronator quadratus, limited proximally by the oblique origin of the former muscle. This space is continuous with the distal synovial sheaths of the flexor tendons and can therefore become a conduit for extending infection from the hand up the forearm. This space can be accessed surgically for drainage via radial and ulnar incisions.[14]
Clinical Significance
During a neurologic exam, the tendon of the brachioradialis is used to test C6 deep tendon reflex[15].
The anatomical snuffbox, which has as its boundaries the tendons of the extensor pollicis longus, the extensor pollicis brevis, and the abductor pollicis, is also a point of significance. If a patient falls on their outstretched hand and has tenderness over the anatomical snuffbox, it can be challenging to differentiate between a strain of the muscles/tendons and a scaphoid fracture. Even if there is no evidence of a scaphoid fracture on radiographs, these patients should be put into a thumb spica splint and followed up in two weeks for repeat X-rays[16].
The proximal-most part of the supinator muscle is tendinous in appearance and termed the arcade of Frohse. It admits the deep branch of the radial nerve to pass beneath it on its way to supply muscles in the extensor compartment further distally. It has been posited that this is the likely site of nerve compression of the deep branch of the radial nerve, causing a variety of clinical syndromes.[17][18]
Media
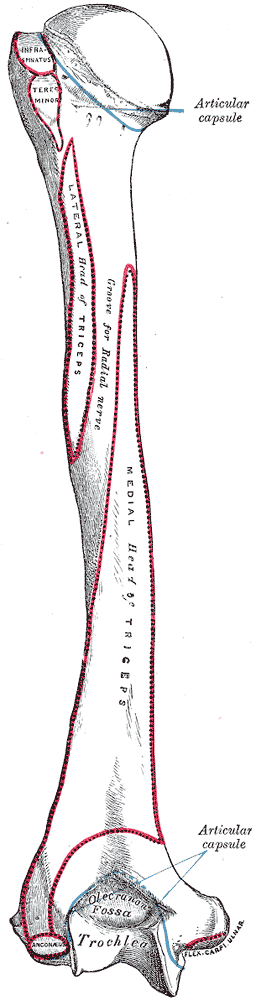
(Click Image to Enlarge)
Upper Arm Anatomy. This illustration details the humerus and various attachment sites on its surface. Shown are the head, surgical and anatomical necks, greater and lesser tubercles, crest of lesser tubercle, intertubercular groove, trochlea capitulum, radial and coronoid fossae, lateral and medial epicondyles, and attachment sites for the subscapularis, coracobrachialis, teres major, latissimus dorsi, pectoralis major, deltoid, brachialis, forearm extensors and flexors, brachioradialis, and extensor carpi radialis longus.
Gray's Anatomy
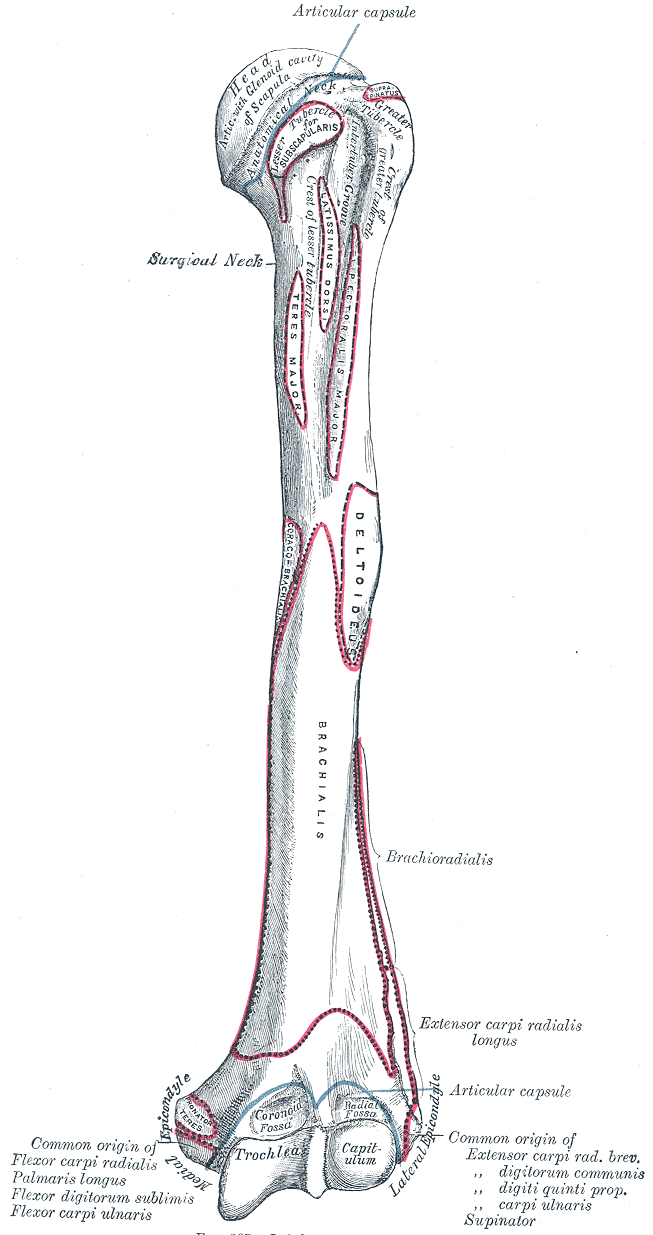
(Click Image to Enlarge)
(Click Image to Enlarge)
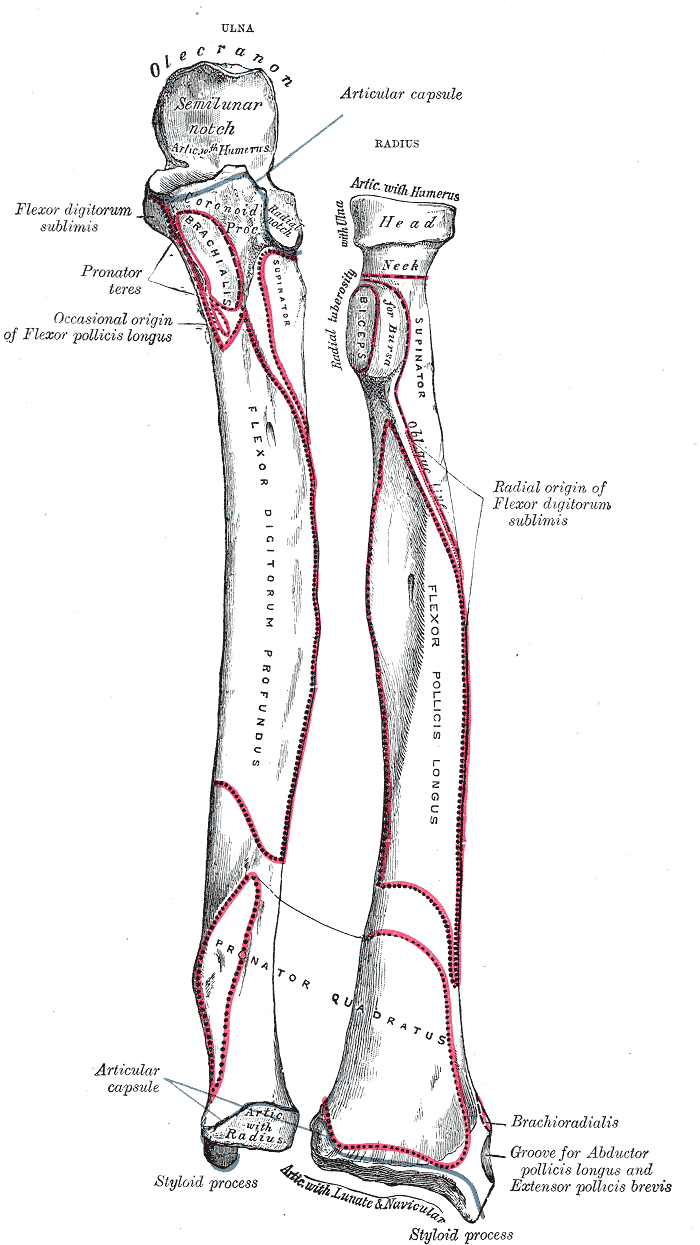
Forearm Bone Markings. Anatomy includes ulna, radius, forearm, articular capsule, olecranon, semilunar notch, flexor digitorum sublimis, flexor, digitorum, pronator teres, brachialis, flexor pollicis longus, pollicis longus, supinator, radial notch, radial tuberosity, biceps, oblique line, flexor digitorum profundus, flexor pollicis longus, radial origin, flexor digitorum sublimis, pronator quadratus, styloid process, brachioradialis, abductor, abductor pollicis longus, and extensor pollicis brevis.
Gray's Anatomy
(Click Image to Enlarge)
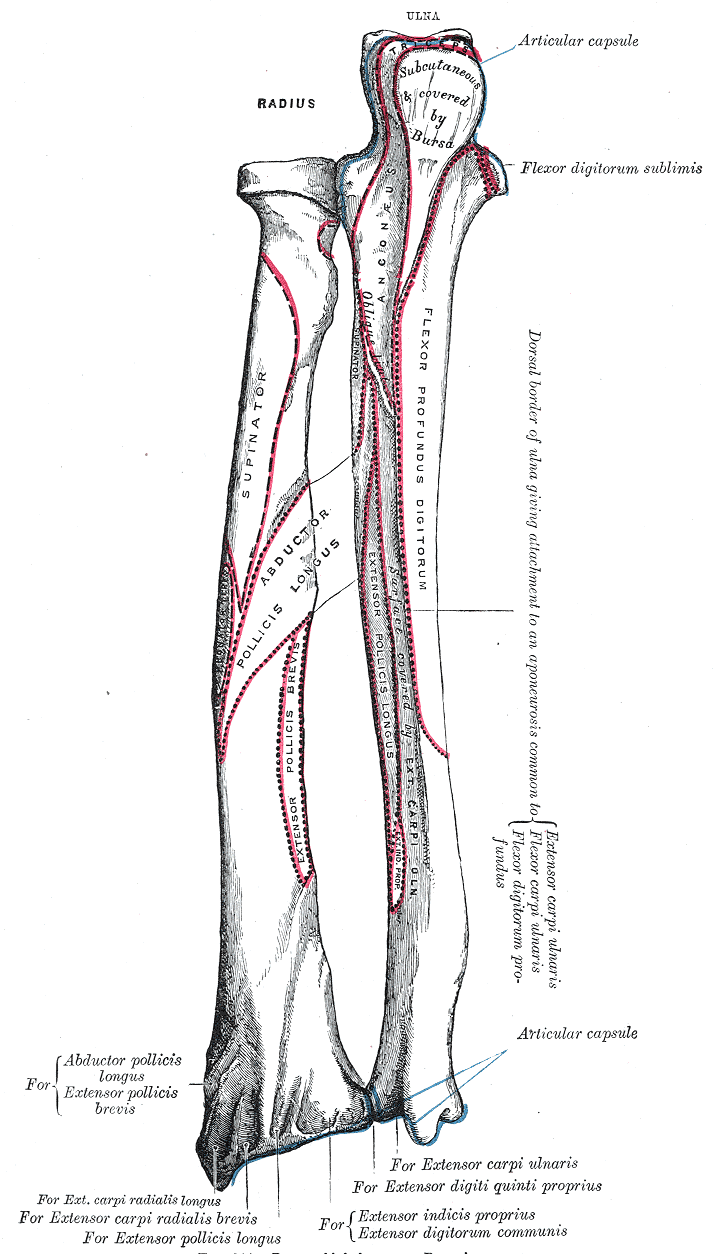
Bone Markings on the Radius and Ulna. This illustration shows the radius and ulna and the muscle attachments of the articular capsule, triceps, supinator, oblique cord, abductor pollicis longus, extensor pollicis longus and brevis, anconeus, aponeurosis, extensor and flexor carpi ulnaris, flexor digitorum profundus and sublimis, and extensor carpi radialis brevis and longus.
Gray's Anatomy
(Click Image to Enlarge)
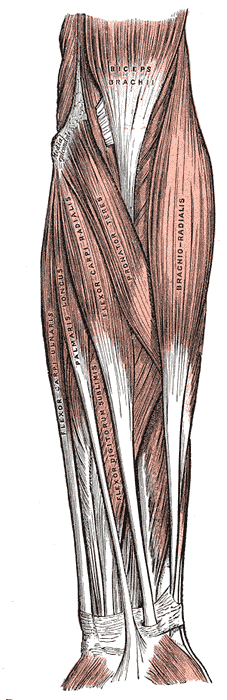
Forearm Muscles. This anterior view shows the biceps brachii, brachioradialis, pronator teres, flexor carpi radialis and ulnaris, palmaris longus, and flexor digitorum sublimis. Other structures in this illustration include the flexor retinaculum (not labeled) and medial epicondyle.
Henry Vandyke Carter, Public domain, via Wikimedia Commons
References
Rodrigues J, Santos-Faria D, Silva J, Azevedo S, Tavares-Costa J, Teixeira F. Sonoanatomy of anterior forearm muscles. Journal of ultrasound. 2019 Sep:22(3):401-405. doi: 10.1007/s40477-019-00388-z. Epub 2019 Jun 10 [PubMed PMID: 31183837]
Revol MP, Lantieri L, Loy S, Guérin-Surville H. Vascular anatomy of the forearm muscles: a study of 50 dissections. Plastic and reconstructive surgery. 1991 Dec:88(6):1026-33 [PubMed PMID: 1946753]
Klausmeyer MA, Mudgal C. Exposure of the forearm and distal radius. Hand clinics. 2014 Nov:30(4):427-33, v. doi: 10.1016/j.hcl.2014.07.002. Epub 2014 Aug 23 [PubMed PMID: 25440071]
Lung BE, Siwiec RM. Anatomy, Shoulder and Upper Limb, Forearm Flexor Carpi Ulnaris Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30252307]
Gervasio A, Stelitano C, Bollani P, Giardini A, Vanzetti E, Ferrari M. Carpal tunnel sonography. Journal of ultrasound. 2020 Sep:23(3):337-347. doi: 10.1007/s40477-020-00460-z. Epub 2020 Apr 22 [PubMed PMID: 32323256]
Lung BE, Burns B. Anatomy, Shoulder and Upper Limb, Hand Flexor Digitorum Profundus Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30252302]
Lung BE, Ekblad J, Bisogno M. Anatomy, Shoulder and Upper Limb, Forearm Brachioradialis Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30252366]
Kerkhof FD, van Leeuwen T, Vereecke EE. The digital human forearm and hand. Journal of anatomy. 2018 Nov:233(5):557-566. doi: 10.1111/joa.12877. Epub 2018 Sep 17 [PubMed PMID: 30225930]
Georgiev GP, Iliev AA, Dimitrova IN, Kotov GN, Malinova LG, Landzhov BV. Palmaris Longus Muscle Variations: Clinical Significance and Proposal of New Classifications. Folia medica. 2017 Sep 1:59(3):289-297. doi: 10.1515/folmed-2017-0035. Epub [PubMed PMID: 28976893]
Ioannis D, Anastasios K, Konstantinos N, Lazaros K, Georgios N. Palmaris Longus Muscle's Prevalence in Different Nations and Interesting Anatomical Variations: Review of the Literature. Journal of clinical medicine research. 2015 Nov:7(11):825-30. doi: 10.14740/jocmr2243w. Epub 2015 Sep 25 [PubMed PMID: 26491493]
Lazo Velásquez JC, Barreto Montalvo J, Atoche Jasaui DR. Connections between the median and ulnar nerves evidenced by electromyography in Lima, Peru, 2016. Revista espanola de cirugia ortopedica y traumatologia (English ed.). 2018 Nov-Dec:62(6):415-420. doi: 10.1016/j.recot.2018.04.002. Epub 2018 Jul 25 [PubMed PMID: 30055949]
Kistler JM, Ilyas AM, Thoder JJ. Forearm Compartment Syndrome: Evaluation and Management. Hand clinics. 2018 Feb:34(1):53-60. doi: 10.1016/j.hcl.2017.09.006. Epub [PubMed PMID: 29169597]
Ortiz-Miguel S, Miguel-Pérez M, Navarro J, Möller I, Pérez-Bellmunt A, Agullo JL, Ortiz-Sagristà J, Blasi J, Martinoli C. Compartments of the antebrachial fascia of the forearm: clinically relevant ultrasound, anatomical and histological findings. Surgical and radiologic anatomy : SRA. 2021 Oct:43(10):1569-1579. doi: 10.1007/s00276-021-02736-3. Epub 2021 Apr 5 [PubMed PMID: 33818623]
Sharma KS, Rao K, Hobson MI. Space of Parona infections: experience in management and outcomes in a regional hand centre. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2013 Jul:66(7):968-72. doi: 10.1016/j.bjps.2013.03.020. Epub 2013 Apr 6 [PubMed PMID: 23571016]
Level 2 (mid-level) evidenceLin-Wei O, Xian LLS, Shen VTW, Chuan CY, Halim SA, Ghani ARI, Idris Z, Abdullah JM. Deep Tendon Reflex: The Tools and Techniques. What Surgical Neurology Residents Should Know. The Malaysian journal of medical sciences : MJMS. 2021 Apr:28(2):48-62. doi: 10.21315/mjms2021.28.2.5. Epub 2021 Apr 21 [PubMed PMID: 33958960]
Tada K, Ikeda K, Okamoto S, Hachinota A, Yamamoto D, Tsuchiya H. Scaphoid Fracture--Overview and Conservative Treatment. Hand surgery : an international journal devoted to hand and upper limb surgery and related research : journal of the Asia-Pacific Federation of Societies for Surgery of the Hand. 2015:20(2):204-9 [PubMed PMID: 26051761]
Level 3 (low-level) evidenceBerton C, Wavreille G, Lecomte F, Miletic B, Kim HJ, Fontaine C. The supinator muscle: anatomical bases for deep branch of the radial nerve entrapment. Surgical and radiologic anatomy : SRA. 2013 Apr:35(3):217-24. doi: 10.1007/s00276-012-1024-x. Epub 2012 Oct 7 [PubMed PMID: 23053118]
Benes M, Kachlik D, Kunc V, Kunc V. The arcade of Frohse: a systematic review and meta-analysis. Surgical and radiologic anatomy : SRA. 2021 May:43(5):703-711. doi: 10.1007/s00276-021-02718-5. Epub 2021 Mar 6 [PubMed PMID: 33677682]
Level 1 (high-level) evidence