Anatomy, Shoulder and Upper Limb, Metacarpophalangeal Joints
Anatomy, Shoulder and Upper Limb, Metacarpophalangeal Joints
Introduction
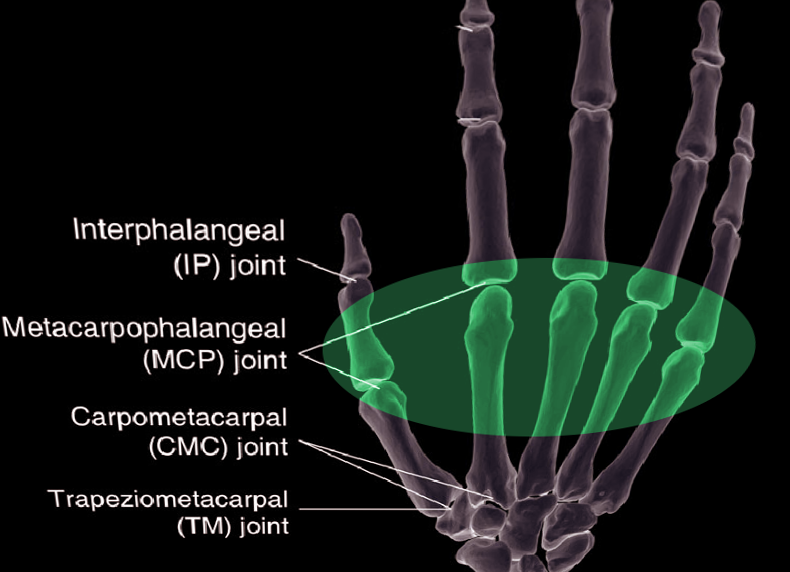
The metacarpophalangeal (MCP) joints are diarthrodial joints where the large convex heads of the distal aspect of the metacarpals articulate with the concave-shaped proximal aspect of each phalange. The articulating surface of each metacarpal head and proximal phalange is composed of hyaline cartilage. There are five separate MCP joints in each hand and these joints serve as transitions between the palm and the fingers. In layman's terms, the MCP joints are known as the “knuckles,” and the metacarpal heads are especially prominent dorsally when making a fist. These joints provide a combination of stability and flexibility which allows for the dexterity required by the hand. Similar to other joints in the body, the MCP joints are acted upon by muscles to allow for specific joint movements. These movements include flexion, extension, abduction, adduction, and limited circumduction. Clinically, arthritis involving the MCP joints is a classic and differentiating feature of rheumatoid arthritis (RA) from osteoarthritis (OA), which typically involves the distal interphalangeal (DIP) joints.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The MCP joints play a critical role in the functionality of the human hand. The MCP joint of the thumb is structurally and functionally similar to the MCP joints of the other digits; however, there are differences and these will be noted when relevant. The thumb MCP joint is a hinge joint that allows up to 80 to 90 degrees of flexion with minimal extension, adduction, or abduction.[1] The MCP joints of the 2 through 5 digits are shallow ball and socket joints which allow for flexion, extension, abduction, adduction, and limited circumduction. In addition to variations in the attachment sites of muscles, a significant difference exists in the range of motion of the MCP joint of the thumb and compared with the MCP joints of the fingers. This difference is accounted for by the shape of the metacarpal heads. In the thumb, the metacarpal head is flatter than the metacarpal heads of the 2nd through 5th MCP joints which reduces its range of motion (ROM). That being said, significant variability in thumb ROM exists because some individuals have more spherical metacarpal heads.[2] This has been found to translate to an increased MCP joint ROM in these individuals.[1]
The shape of the MCP joint provides minimal intrinsic stability. The joint is primarily stabilized by ligaments, the joint capsule, and the surrounding musculotendinous balance.[3]
The volar plate is a dense fibrocartilaginous thickening of the palmar aspect of the MCP joint capsule. The volar plate’s primary function is to prevent hyperextension of the joint.[3] It originates on the metacarpal head and inserts onto the adjacent proximal phalange. The proximal third of the palmar plate is thinner than the distal portion, and the thumb has two sesamoid bones embedded in it.[4] The sesamoids, connected via the phalangoglenoid ligament, work in conjunction with the palmar plate and A1 annular ligament to form a synovial sheath for the flexor pollicis longus tendon, thereby stabilizing it as it passes over the MCP joint. The palmar plates of digits 2 through 5 are connected by the deep transverse metacarpal ligament providing stabilization and preventing separation between metacarpal heads.[5]
A collateral ligament, comprised of a proper collateral ligament and an accessory collateral ligament, is present on both the radial and ulnar aspects of each MCP joint. The proper collateral ligaments are strong cord-like structures that act as the primary stabilizers of the MCP joint. The proper collateral ligaments originate from the lateral-dorsal aspect of the metacarpal head and transverse the joint to insert onto the volar margin of the adjacent proximal phalange. The accessory collateral ligaments originate more volar and proximal than the proper collateral ligament and fan outward in an oblique direction to insert onto the distal third of the volar plate.[3] Due to the difference in orientation of these two collateral ligaments as well as the unique ovoid shape of the metacarpal head, the proper collateral ligaments are taut in joint flexion while accessory collateral ligaments are taut in joint extension.[6] Additionally, these differences result in a cam effect permitting a substantial range of motion (ROM) in the flexion-extension axis, as well as adduction-abduction.[5]
The joint capsule surrounds the MCP joint blending with the palmar plate and the collateral ligaments. It functions to stabilize the joint dorsally and is taut in joint flexion.
Sagittal bands arise from the plantar plate and wrap around the MCP joint superficially creating a “lasso” around the underlying extensor muscle tendon. This structure allows the extensor muscle to extend the MCP joint despite minimal attachment to the proximal phalanx.
Embryology
Three primary signaling centers, the apical ectodermal ridge (AER), the zone of polarizing activity (ZPA), and the nonridged ectoderm, interact in a well-coordinated manner to direct appropriate developmental axis formation for the upper extremity.[7] By the end of the fourth week of embryonic development, four limb buds arise from the ventrolateral surface of the developing embryo. The limb buds consist of somites and mesenchyme, derived from the lateral plate mesoderm, enclosed by a layer of cuboidal ectoderm.[8] The cells from the lateral plate mesoderm will eventually differentiate into the extremity’s connective tissue. Limb musculature derives from the paraxial mesoderm cells of the somites that had migrated into the limb buds. The ectoderm layer at the distal tip of the developing limb eventually enlarges to form the AER. The AER induces neighboring mesenchymal cells to remain undifferentiated and continue proliferating while more proximal limb cells further away from the AER begin to differentiate into connective tissue and muscle cells.
By the end of the sixth week of embryonic development, chondrocytes have formed a basic construct of hyaline cartilage that will eventually ossify into the bones of the upper extremity through the process of endochondral ossification. The MCP joints are formed in this cartilage when factor signaling causes chondrogenesis to cease locally, ultimately resulting in the formation of a joint cavity. Mesenchymal cells adjacent to the joint cavity subsequently differentiate into the joint capsule. By the ninth week, the diaphyses of the metacarpal and proximal phalanges are ossified; however, the epiphyses are ossified postnatally.[8]
Blood Supply and Lymphatics
Blood is supplied to the hand via the ulnar and radial arteries which anastomose in the superficial palmar and deep palmar arches. These arches have numerous branches, many of which supply the MCP joints including princeps pollicis artery, the radial artery of the index finger, common palmar digital arteries, and the dorsal and palmar metacarpal arteries.[9]
Lymphatic drainage for the hand occurs via superficial channels that run alongside the cephalic and basilic veins as well as deep channels that course with the arteries. These lymphatics drain to lymph nodes within the elbow, including the cubital and epitrochlear lymph nodes, before ultimately draining into the axillary or infraclavicular lymph nodes.
Nerves
The muscles crossing the MCP joint receive innervation via branches from the three main nerves of the forearm: median, ulnar, and radial. The MCP joints receive its innervation from the posterior interosseous nerve, the deep terminal branch of the ulnar nerve and palmar branches of the median nerve.
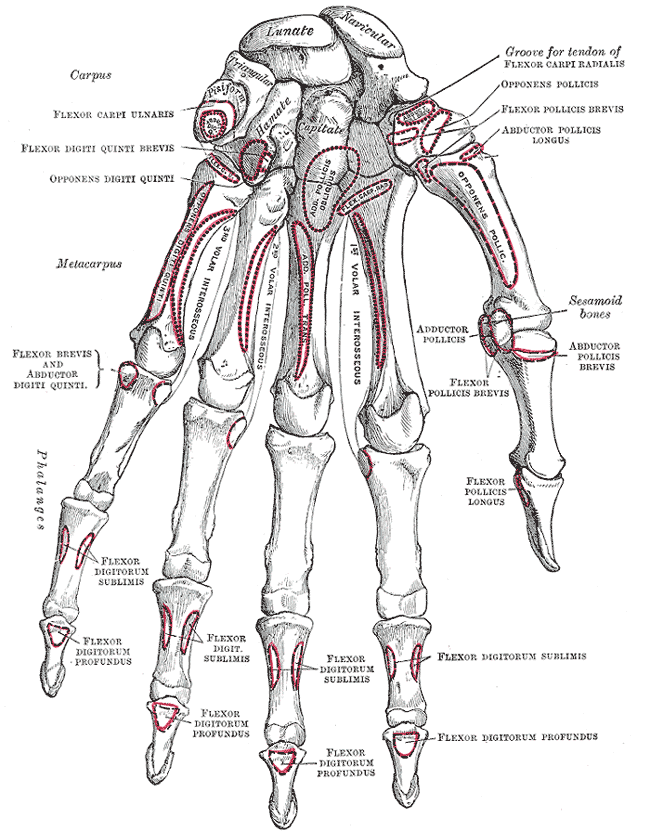
Muscles
Both intrinsic and extrinsic muscles cross the MCP joint. Intrinsic muscles are those originating within the hand while extrinsic muscles are those that the outside the hand. The MCP joint may also be grouped by their respective movement type:[10][11][12][13]
Extension
- Digits 2 to 5: Extensor digitorum, extensor indicis (second digit), extensor digiti minimi (fifth digit)
- Thumb: Extensor pollicis longus, Extensor pollicis brevis
Flexion
- Digits 2 to 5: Flexor digitorum superficialis, flexor digitorum profundus, Flexor digiti minimi brevis (fifth digit), Lumbricals*
- Thumb: Flexor pollicis longus, Flexor pollicis brevis*
Abduction
- Digits 2 to 4: Dorsal Interossei*
- Fifth digit: Abductor digiti minimi
- Thumb: Abductor pollicis longus, Abductor pollicis brevis*
Adduction
- Digits 2 to 5: Palmer interossei*
- Thumb: Adductor pollicis*
Of note, both muscles of adduction also assist in flexion of their respective MCP joints.
*Intrinsic muscles
Surgical Considerations
Surgical Repair of Acute Ulnar Collateral Ligament Injury of the Thumb
Surgical repair of the UCL is indicated for an acute injury to the ligament that results in a complete tear. Injuries that have been present for greater than 3 to 6 weeks typically require surgical reconstruction; however, there is no consensus on whether surgical reconstruction or repair of the UCL ligament is preferred for either acute or chronic UCL injury of the thumb. The clinical presentation of UCL injury is discussed in further detail below. MCP joint laxity is assessed to determine if there is a complete UCL tear. This is done by applying a valgus stress to the MCP joint while holding it in mild extension. If greater than 35 degrees of radial deviation is present or there is more than a 20-degree difference from the uninjured thumb, then a complete UCL tear is highly suspected.[14]
Surgical exposure is gained from an incision on the dorsal aspect of the thumb MCP joint. The joint capsule is exposed by vertically incising the adductor aponeurosis to the extensor pollicis longus.[15] The torn UCL is identified and carefully dissected from adjacent tissue to ensure the maintenance of its metacarpal attachment. The location of the UCL reattachment at the proximal phalanx is identified and cleaned. The distal end of the UCL ligament is then attached to the proximal phalanx by either bone anchors with pre-attached suture or tunneling suture through the bone.[16] Both methods require temporary MCP joint fixation with a percutaneous, transarticular Kirschner wire (K wire).[15] Following closure, a splint is worn for 6 weeks postoperatively, and physical therapy helps to restore ROM and strength of the thumb. Full return to activity is typically achieved after 16 weeks.
Open Reduction for MCP Joint Dislocation
Open reduction is indicated for irreducible MCP joint dislocations. The clinical findings of MCP joint dislocation are discussed below. In complex dislocations, the volar plate is either entrapped between the joint surfaces or has maintained its proximal phalanx attachment and is lying on the dorsal aspect of the metacarpal shaft. Occasionally seen in complex dislocations, the metacarpal head may become buttonholed between ligaments and tendons preventing closed reduction and requiring open reduction.[15]
To perform an open reduction of the MCP joint, a dorsal, volar, or combined approach may be used to obtain proper exposure.[17] The dorsal approach is typically preferred because it is less likely to damage the sensitive digital neurovascular structures, and allows for proper exposure and fixation if metacarpal fractures are present.[17] An example of a situation where a combined approach may be needed may be for a dislocation that was not treated acutely. Following the incision on the dorsal aspect of the MCP joint, the extensor mechanism is identified and split to provide exposure of the joint capsule. Dissection and incision of remaining intact dorsal joint capsule allows for the visualization of the volar plate, metacarpal head, and displaced proximal phalanx.[17] The metacarpal head may be deep to the dorsally displaced proximal phalanx or buttonholed making it difficult to be visualized initially. The dislocation is then reduced by holding the wrist in flexion to decrease tension within the flexor tendons and then applying gentle force to the proximal phalanx in the distal and palmar direction. The volar plate may need to be vertically incised to allow for reduction.[18] Joint stability may be assessed by taking the MCP joint through a full passive range of motion.[19] Once joint stability is ensured, the dorsal capsule and extensor mechanism are repaired, and the skin is closed. A splint is used to immobilize the MCP joint in 10 degrees of flexion. Full return to activity is typically achieved after 12 weeks.
MCP Joint Arthroplasty
Several joint prostheses types are available for MCP joint arthroplasty; however, silicone implant arthroplasty is currently the gold standard. Other small joint arthroplasty options include pyocarbon implant arthroplasty and autologous small joint transfer.[20]
The primary indication for silicone implant MCP joint arthroplasty is arthritis (osteoarthritis, rheumatoid arthritis, post-traumatic type), and these surgeries can usually treat the joint deformations from these diseases. These deformities include complex joint dislocations, volar subluxation, and severe articular cartilage damage. Pyocarbon implant arthroplasty is not suggested in RA affected joints as it relies on significant soft tissue support to bolster the implant.[20]
Silicone implant arthroplasty begins with a transverse incision made on the dorsal aspect of the metacarpal neck while preserving the superficial neurovascular structures. Next, the extensor tendons are bluntly dissected to reveal the underlying joint capsule. With the joint capsule exposed, a release of the sagittal band is performed, followed by a release of the collateral ligaments, and finally a release of the joint capsule.[21] The metacarpal head is then resected. The medullary canal of the proximal phalanx is broached, followed by the associated metacarpal bone. An implant is then inserted, and the capsule is closed to keep the implant in place. The implant serves as the new MCP joint. Post-operative management consists of 12 weeks in a splint and physical therapy beginning at 6 weeks.
Silicone implant arthroplasty typically provides significant pain relief; however, only marginal improvements are seen on MCP joint range of motion postoperatively.[22]
Clinical Significance
Rheumatoid Arthritis
While both osteoarthritis and rheumatoid arthritis can affect the MCP joint, rheumatoid arthritis (RA) is classically associated with a predilection for MCP involvement. RA is a chronic systemic autoimmune disease characterized by polyarthropathy and resultant cartilage and bone destruction.
Over time, the chronic synovitis of RA leads to the deposition of granulation tissue resulting in the formation of a pannus. Progressively, the myofibroblasts within the pannus contract, distorting the natural joint alignment. This process is classically seen in the MCP joint as an ulnar deviation and in the PIP joint as the swan neck deformity. For RA patients presenting with ulnar deviation at the MCP joint, treatment consists of several operative options including:
- Small joint synovectomy is indicated for early joint disease[23][24]
- MCP arthroplasty is indicated for advanced joint disease
- MCP joint arthrodesis is indicated if the thumb MCP joint is affected without interphalangeal joint (IP) involvement[24]
MCP Joint Dislocation
Dislocations of the MCP joint can occur on either the volar or dorsal aspect of the joint and are classified as either simple or complex. Dorsal dislocations are more common, and occur secondary to hyperextension of the joint, most commonly from a fall on an outstretched hand.[25] In comparison, volar dislocations occur from hyperflexion or hyperextension of the joint. The presence of the volar plate and strong lateral ligaments help to explain why the majority of MCP joint dislocation occurs dorsally, as opposed to lateral or volar dislocation. Simple dislocations are those that are capable of being reduced by closed reduction. Complex dislocations, however, are typically not amenable to closed reduction.[26] During hyperextension, the palmar plate tears from its point of origin on the metacarpal neck. In the case of complex dislocations, the palmar plate becomes interposed in the dislocated joint. The MCP joint of the second digit is the most commonly involved joint in both simple and complex dislocations.
Physical exam findings vary depending on whether the dislocation is volar or dorsal. For dorsal dislocations, the joint will appear somewhat hyperextended due to damage to both the palmar plate and joint capsule. Upon inspection, complex dislocations counterintuitively may appear to have less displacement because the proximal phalanx can be seen resting on the dorsal aspect of the metacarpal head.[25] Evidence of MCP joint dislocation is best viewed on a true lateral radiograph, which shows a widened joint space due to the interposition of the volar plate. Non-operative management is performed with closed reduction with anesthesia for simple dislocations, while complex dislocations are managed surgically by open reduction.
Ulnar Collateral Ligament Injury of the Thumb [27]
Injury to the ulnar collateral ligament (UCL) of the MCP joint of the thumb is commonly referred to as gamekeeper’s or skier’s thumb. Gamekeeper’s thumb is the result of chronic and repeated injuries to the UCL that results in UCL attenuation. Over time this results in chronic joint instability of the MCP of the thumb. Skier’s thumb refers to an acute UCL injury such as when a skier falls on a ski pole causing a radial deviation or hyperabduction of the thumb at the MCP joint.[28] The hyperabduction causes the separation of the UCL from the base of the first phalanx of the thumb. Commonly as the UCL tears, a portion of the adductor pollicis aponeurosis becomes caught between the avulsed ligament and its previous site of bony attachment. This is known as a Stener lesion and prevents the ligament from healing without appropriate surgical intervention.[28] Stener lesions are present in approximately 64% to 87% of complete UCL tears, which is why surgical repair is typically preferred for complete UCL tears.[28]
On physical examination of a patient with a UCL tear, the torn ligament may present as a mass on the ulnar aspect of the MCP joint. The instability of the joint may be noted by applying radially-directed pressure to the joint. If instability is noted with the thumb in a neutral position, this is indicative of damage to only the proper UCL. Upon the application of valgus stress while holding the MCP joint in extension, if greater than 35 degrees of radial deviation is present or there is more than a 20-degree difference from the uninjured thumb, then a complete UCL tear is likely.[28] Treatment for partial tears with minimal valgus and varus instability is non-surgical management with 6 weeks of immobilization.[28] Indications for operative management include acute injuries with significant joint laxity, the presence of a Stener lesion, and chronic injury. Operative management involves either ligament repair or reconstruction depending on injury severity and chronicity.
Media
(Click Image to Enlarge)
References
Yoshida R, House HO, Patterson RM, Shah MA, Viegas SF. Motion and morphology of the thumb metacarpophalangeal joint. The Journal of hand surgery. 2003 Sep:28(5):753-7 [PubMed PMID: 14507504]
Shah MA, Buford WL, Viegas SF. Effects of extensor pollicis longus transposition and extensor indicis proprius transfer to extensor pollicis longus on thumb mechanics. The Journal of hand surgery. 2003 Jul:28(4):661-8 [PubMed PMID: 12877857]
Leversedge FJ. Anatomy and pathomechanics of the thumb. Hand clinics. 2008 Aug:24(3):219-29, v. doi: 10.1016/j.hcl.2008.03.010. Epub [PubMed PMID: 18675713]
Barry K, McGee H, Curtin J. Complex dislocation of the metacarpo-phalangeal joint of the index finger: a comparison of the surgical approaches. Journal of hand surgery (Edinburgh, Scotland). 1988 Nov:13(4):466-8 [PubMed PMID: 3249153]
Level 3 (low-level) evidenceRozmaryn LM. The Collateral Ligament of the Digits of the Hand: Anatomy, Physiology, Biomechanics, Injury, and Treatment. The Journal of hand surgery. 2017 Nov:42(11):904-915. doi: 10.1016/j.jhsa.2017.08.024. Epub [PubMed PMID: 29101974]
Kataoka T, Moritomo H, Miyake J, Murase T, Yoshikawa H, Sugamoto K. Changes in shape and length of the collateral and accessory collateral ligaments of the metacarpophalangeal joint during flexion. The Journal of bone and joint surgery. American volume. 2011 Jul 20:93(14):1318-25. doi: 10.2106/JBJS.J.00733. Epub [PubMed PMID: 21792498]
Tickle C. How the embryo makes a limb: determination, polarity and identity. Journal of anatomy. 2015 Oct:227(4):418-30. doi: 10.1111/joa.12361. Epub 2015 Aug 7 [PubMed PMID: 26249743]
Cole P, Kaufman Y, Hatef DA, Hollier LH Jr. Embryology of the hand and upper extremity. The Journal of craniofacial surgery. 2009 Jul:20(4):992-5. doi: 10.1097/SCS.0b013e3181abb18e. Epub [PubMed PMID: 19553860]
Gellman H, Botte MJ, Shankwiler J, Gelberman RH. Arterial patterns of the deep and superficial palmar arches. Clinical orthopaedics and related research. 2001 Feb:(383):41-6 [PubMed PMID: 11210968]
Valenzuela M, Varacallo M. Anatomy, Shoulder and Upper Limb, Hand Lumbrical Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 30521297]
Ramage JL, Varacallo M. Anatomy, Shoulder and Upper Limb, Wrist Extensor Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 30521226]
Valenzuela M, Varacallo M. Anatomy, Shoulder and Upper Limb, Hand Interossei Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 30521193]
Raszewski JA, Black AC, Varacallo M. Anatomy, Shoulder and Upper Limb, Hand Compartments. StatPearls. 2023 Jan:(): [PubMed PMID: 30422537]
Fricker R, Hintermann B. Skier's thumb. Treatment, prevention and recommendations. Sports medicine (Auckland, N.Z.). 1995 Jan:19(1):73-9 [PubMed PMID: 7740248]
Haddock NT, Beasley RW, Sharma S. Thumb metacarpophalangeal joint ulnar collateral ligament repair with condylar shaving. Techniques in hand & upper extremity surgery. 2009 Dec:13(4):199-201. doi: 10.1097/BTH.0b013e3181c3f14e. Epub [PubMed PMID: 19956046]
Weiland AJ, Berner SH, Hotchkiss RN, McCormack RR Jr, Gerwin M. Repair of acute ulnar collateral ligament injuries of the thumb metacarpophalangeal joint with an intraosseous suture anchor. The Journal of hand surgery. 1997 Jul:22(4):585-91 [PubMed PMID: 9260611]
Level 3 (low-level) evidenceBecton JL, Christian JD Jr, Goodwin HN, Jackson JG 3rd. A simplified technique for treating the complex dislocation of the index metacarpophalangeal joint. The Journal of bone and joint surgery. American volume. 1975 Jul:57(5):698-700 [PubMed PMID: 1150718]
Afifi AM, Medoro A, Salas C, Taha MR, Cheema T. A cadaver model that investigates irreducible metacarpophalangeal joint dislocation. The Journal of hand surgery. 2009 Oct:34(8):1506-11. doi: 10.1016/j.jhsa.2009.06.001. Epub 2009 Aug 22 [PubMed PMID: 19703736]
Schubiner JM, Mass DP. Operation for collateral ligament ruptures of the metacarpophalangeal joints of the fingers. The Journal of bone and joint surgery. British volume. 1989 May:71(3):388-9 [PubMed PMID: 2722926]
Adkinson JM, Chung KC. Advances in small joint arthroplasty of the hand. Plastic and reconstructive surgery. 2014 Dec:134(6):1260-1268. doi: 10.1097/PRS.0000000000000733. Epub [PubMed PMID: 25415093]
Level 3 (low-level) evidenceSwanson AB, Herndon JH. Flexible (silicone) implant arthroplasty of the metacarpophalangeal joint of the thumb. The Journal of bone and joint surgery. American volume. 1977 Apr:59(3):362-8 [PubMed PMID: 849948]
Waljee JF, Chung KC. Objective functional outcomes and patient satisfaction after silicone metacarpophalangeal arthroplasty for rheumatoid arthritis. The Journal of hand surgery. 2012 Jan:37(1):47-54. doi: 10.1016/j.jhsa.2011.09.042. Epub [PubMed PMID: 22196292]
Level 2 (mid-level) evidenceKozlow JH, Chung KC. Current concepts in the surgical management of rheumatoid and osteoarthritic hands and wrists. Hand clinics. 2011 Feb:27(1):31-41. doi: 10.1016/j.hcl.2010.09.003. Epub 2010 Nov 20 [PubMed PMID: 21176798]
Alderman AK, Ubel PA, Kim HM, Fox DA, Chung KC. Surgical management of the rheumatoid hand: consensus and controversy among rheumatologists and hand surgeons. The Journal of rheumatology. 2003 Jul:30(7):1464-72 [PubMed PMID: 12858442]
Level 2 (mid-level) evidenceKAPLAN EB. Dorsal dislocation of the metacarpophalangeal joint of the index finger. The Journal of bone and joint surgery. American volume. 1957 Oct:39-A(5):1081-6 [PubMed PMID: 13475407]
Sumarriva G, Cook B, Godoy G, Waldron S. Pediatric Complex Metacarpophalangeal Joint Dislocation of the Index Finger. The Ochsner journal. 2018 Winter:18(4):398-401. doi: 10.31486/toj.18.0032. Epub [PubMed PMID: 30559627]
Acosta JR, Graefe SB, Varacallo M. Anatomy, Shoulder and Upper Limb, Hand Adductor Pollicis. StatPearls. 2023 Jan:(): [PubMed PMID: 30252315]
Mahajan M, Rhemrev SJ. Rupture of the ulnar collateral ligament of the thumb - a review. International journal of emergency medicine. 2013 Aug 12:6(1):31. doi: 10.1186/1865-1380-6-31. Epub 2013 Aug 12 [PubMed PMID: 23938194]