Anatomy, Shoulder and Upper Limb, Sternoclavicular Joint
Anatomy, Shoulder and Upper Limb, Sternoclavicular Joint
Introduction
The sternoclavicular (SC) joint is a saddle-shaped, synovial joint that is the primary skeletal connection between the axial skeleton and the upper limb. A fracture of the clavicle renders the upper limb virtually useless.
The sternoclavicular joint is one of five articulations essential for the function of the upper limb. Several critical structures have an anatomical relationship to the sternoclavicular joint, including the brachiocephalic arterial trunk, internal jugular vein, and common carotid artery. Other structures include the vagus and phrenic nerves, trachea, and esophagus. Thus, in addition to its critical role in stabilizing and supporting the upper limb, the sternoclavicular joint and its component parts - the clavicle and sternum - play an essential protective role for structures entering the thorax.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
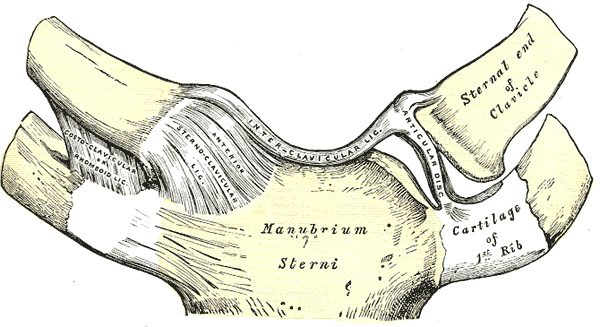
The sternoclavicular joint articulates the clavicle with the manubrium of the sternum and the superior surface of the first costal cartilage. From an anteroposterior axis, the joint is convex. Vertically, the joint is concave. Structurally, the articulating surfaces of the SC joint are separated by a fibrocartilaginous articular disc which has functional mobility in the anteroposterior and vertical axis.[1]
The posterior sternoclavicular ligament provides the primary anteroposterior stabilization of the SC joint. This ligament extends from the posterior aspect of the sternal end of the clavicle to the posterosuperior manubrium. The anterior sternoclavicular ligament also stabilizes the SC joint and prohibits excessive superior displacement. This ligament joins the medial end of the clavicle and the superior anterior edge of the manubrium.
Other ligaments contributing to the stability of the SC joint are the interclavicular ligament which facilitates medial traction of both clavicles, and the costoclavicular ligament, which mediates bilateral clavicle and anterior first rib stability. The orientation of the costoclavicular ligament to the SC joint, anchoring the inferior surface of the sternal end of the clavicle to the first rib, serves as the primary restraint for the SC joint.
The subclavius muscle also functions to provide SC joint stability. The subclavius muscle arises from the first rib and its costal cartilage. This muscle passes laterally to insert on the inferior surface of the middle third of the clavicle. The subclavius muscle helps protect the brachial plexus and vascular supply of the arm. The subclavius is innervated by the nerve to the subclavius (C5, C6) from the upper trunk of the brachial plexus. When the subclavius muscle contracts, it depresses and anchors the clavicle. [2]
The SC joint is one of five articulations that permit fluid movement of the shoulder girdle. Functionally, the joint is a diarthrodial, multiaxial joint that provides 35 degrees range of motion for movement in the horizontal and coronal planes and 70 degrees range of motion anteroposteriorly. The joint is also capable of 45 degrees of rotation along its long axis. Mechanical input from the shoulder girdle influences the movements of the SC joint.
Meaningful anatomical relationships concerning the SC joint are also worth noting. The brachiocephalic trunk, internal jugular vein, and common carotid artery lie posterior to the SC joint. Other mediastinal structures that lie posterior to the clavicle and SC joint are the vagus nerve, phrenic nerve, trachea, and esophagus. These relationships have clinical significance and will be discussed below.
Embryology
Somites develop into the sclerotomes, which are located ventromedially, and the dorsolateral dermomyotomes. The cells of the sclerotome form mesenchyme by the end of the fourth week. The sclerotomal cells form osteoblasts (which form bone), fibroblasts (which form connective tissue), and chondroblasts (which form cartilage).
The shoulder is formed from lateral plate mesoderm. Hyaline cartilage models undergo endochondral ossification in which the cartilage forms bone shaped based on the cartilaginous model. The upper limb undergoes rotation of 90 degrees so that the extensor muscles are located posteriorly and laterally. The chondrocytes are formed by the sixth week. They establish the cartilaginous models, which undergo ossification to form the bone. By the end of the twelfth week, the ossification centers of the long bones have been developed in the osseous diaphysis.
Joints are formed in the cartilaginous portion where cell growth stops, leading to the formation of an interzone—the number of cells in the interzone increases. Cell death (apoptosis) leads to the formation of the marrow cavity.
The shaft of the bone is well ossified at birth, but the epiphyses remain cartilaginous, forming a growth center. Irregular bones may have more than one growth center.
Blood Supply and Lymphatics
The vascular supply of the sternoclavicular joint derives from the internal thoracic artery and suprascapular artery. Both arteries are branches of the subclavian artery. The internal thoracic artery is a direct branch of the subclavian artery. According to Gray's Anatomy, the suprascapular artery is a branch of the thyrocervical trunk, a branch of the subclavian artery.
Nerves
The sternoclavicular joint is directly innervated by the medial supraclavicular nerve (C3-C4) and the nerve to the subclavius (C5-C6). The nerves are involved in the various movements at the joint.
- Elevation: accomplished by the levator scapulae, upper trapezius, rhomboid major and minor muscles
- Levator scapulae: Dorsal scapular nerve (C5, C6); cervical nerves (C3, C4)
- Trapezius: Spinal accessory nerve (cranial nerve eleven XI)(motor function); pain and proprioception: cervical nerves (C3, C4)
- Rhomboid major and minor: Dorsal scapular nerve (C4, C5)
- Depression: pectoralis minor, lower trapezius, serratus anterior muscles
- Pectoralis minor: Medial pectoral nerve (C8, T1)
- Trapezius: Spinal accessory nerve (cranial nerve eleven XI)(motor function); pain and proprioception cervical nerves (C3, C4)
- Serratus anterior: Long thoracic nerve (C5, C6, C7)
- Protraction: pectoralis minor, serratus anterior muscles
- Pectoralis minor: Medial pectoral nerve (C8,T1)
- Serratus anterior: Long thoracic nerve (C5, C6, C7)
- Retraction: middle trapezius, latissimus dorsi, rhomboid major and minor muscles
- Trapezius: Spinal accessory nerve (cranial nerve eleven XI)(motor function); pain and proprioception cervical nerves (C3,C4)
- Latissimus dorsi: Thoracodorsal nerve (C6, C7, C8)
- Rhomboid major and minor: Dorsal scapular nerve (C4,C5)
- Rotation via elevation of the glenoid cavity: upper and lower trapezius, serratus anterior muscles
- Upper and lower trapezius: Spinal accessory nerve (cranial nerve eleven XI); pain and proprioception cervical nerves (C3, C4)
- Serratus anterior: Long thoracic nerve (C5, C6, C7)
- Rotation via depression of the glenoid cavity: levator scapulae, latissimus dorsi, pectoralis minor, rhomboid major and minor muscles
- Levator scapulae: Dorsal scapular nerve (C4, C5)
- Latissimus dorsi: Thoracodorsal nerve (C6, C7, C8)
- Pectoralis minor: Medial pectoral nerve (C8, T1)
- Rhomboid major and minor: Dorsal scapular nerve (C4, C5)
Muscles
While no muscles directly act on the sternoclavicular joint, clinicians must understand that the movement of the SC joint primarily depends on the motion of the scapula and the entire shoulder girdle, including the clavicle. Muscles inserting on the clavicle that influence the movement of the SC joint include the deltoid, pectoralis major, trapezius, and sternocleidomastoid muscles.
Deltoid
- Origin: Lateral third clavicle, acromion, the spine of the scapula
- insertion: Deltoid tuberosity
- Innervation: Axillary nerve (C5,C6)
- Action: Anterior part flexes and rotates the arm; the middle part: abducts the arm; the posterior part: extends and rotates the arm
Pectoralis Major
- Origin: Clavicular head: medial half of clavicle; sternocostal head: Sternum, superior six costal cartilages
- Insertion: Lateral lip intertubercular sulcus
- Nerve supply: Lateral head: lateral and medial pectoral nerves (C5,C6); medial head lateral and medial pectoral nerves (C7,C8,T1).
- Actions: Adducts and medially rotates humerus; moves scapula anteriorly and inferiorly
Trapezius
- Origin: Nuchal line, external occipital protuberance, ligamentum nuchae; spinous processes C7-T12
- Insertion: Lateral third clavicle; acromion, the spine of the scapula
- Innervation: Spinal accessory nerve (cranial nerve eleven XI)(motor function); cervical nerves (C3,C4) - pain and proprioception
- Action: complex - see Nerves section above
Sternocleidomastoid
- Origin: Manubrium of the sternum; the medial third of the clavicle
- Insertion: Mastoid process; superior nuchal line
- Innervation: Spinal accessory nerve (cranial nerve XI – motor); C2,C3 (pain and proprioception)
- Action: Tilts head to the ipsilateral side; rotates head so face pointed towards the contralateral side
Physiologic Variants
There are not many anatomical or physiological variations concerning the sternoclavicular joint. However, some patients may have more prominent attachments of the ligaments supporting the SC joint than others, especially the costoclavicular ligament. This should not be viewed as pathological.
Surgical Considerations
Traumatic dislocation of the sternoclavicular joint can result in chronic instability of the joint or in arthritic changes that can limit the activities of athletes and those with an active lifestyle.[3] Options that can be offered to such patients include sternoclavicular joint reconstruction or medial clavicular resection. For athletic injuries in athletes who intend to continue playing sports, an approach in which the tissues of the tendon(s) are woven in a figure-eight pattern into drill holes has been shown to produce superior results.[4]
Clinical Significance
Trauma
Traumatic injury to the sternoclavicular joint is rare, accounting for only 3% to 5% of shoulder girdle injuries.[5] Given the robust stability and reinforcement of the joint, a significant force or a specific vector is often required to damage its structural and functional integrity, such as a motor vehicle collision or a direct blow from a contact sport or fall. Often, an indirect blow to the shoulder is the cause of trauma that damages the SC joint; direct blows to the medial clavicle are also frequent. If strong enough to disrupt the joint space, such blunt force trauma will lead to SC joint dislocation.
Patients with direct trauma to the SC joint often present with pain localizable to the joint itself. They may complain of shoulder pain or pain in the anterior chest. Frequently, the patient will have a prior history of trauma, but this is not always the case, as some SC joint injuries may be insidious in presentation. Physical exam may likely reveal swelling, a bony prominence of the sternum or clavicle, pain and tenderness, ecchymosis, severe pain, and reduced shoulder joint range of motion.[6]
- Dislocation: SC joint dislocations comprise 1% to 3% of all dislocations. Depending on the direction of the injuring force, SC joint dislocations can either be anterior or posterior in orientation.
- Anterior dislocations result from blows in an anterolateral direction. They are more common than posterior dislocations.
- Posterior dislocations are the result of blows in a posterolateral direction. Posterior SC joint dislocations put mediastinal structures at risk. The clinician should note any sign of dysphagia, stridor, dyspnea, paresthesia, diminished extremity pulses, or cyanosis. Potential complications of posterior SC joint dislocations include pneumothorax, brachial plexus injury, vascular injury, dysphagia, and hoarseness.[7][8][9][10]
- Sprain: no joint laxity or instability.
- Subluxation: tearing of sternoclavicular ligaments, but costoclavicular ligaments intact.
SC joint injuries are classified on the following basis depending on the extent of the injury.[5]
- Type 1: SC joint sprain without laxity or pain.
- Type 2: SC joint ligaments rupture, costoclavicular ligaments intact; joint subluxation.
- Type 3: SC joint ligaments and costoclavicular ligaments ruptured; joint dislocation.
Treatment of SC joint injuries is conservative if atraumatic. In anterior dislocations, conservative management is recommended. Acute posterior dislocations without evidence of mediastinal injury require management with closed reduction. However, if there are signs of mediastinal injury, emergent open reduction, and internal fixation are warranted.
Osteoarthritis
Osteoarthritis, a condition seen predominately in patients over 60 years of age, is relatively common in the SC joint, with one study showing a prevalence of 89% in patients above age 50.[11] Pain associated with osteoarthritis is produced by forward flexion or abduction of the arm. Radiographically, osteoarthritis demonstrates features such as subchondral cysts, joint space narrowing, osteophytes, and subchondral sclerosis.[12] Treatment is primarily conservative.
Infection
Infection of the SC joint is rare and presents insidiously with a low-grade fever, erythema, mild shoulder discomfort, and joint swelling. The primary organisms responsible for infection of the SC joint are Staphylococcus aureus and Pseudomonas aeruginosa. Diagnosis involves arthrocentesis and MRI to assess joint integrity. Treatment is surgical debridement, en-bloc resection, and antibiotic therapy.[13]
Gout
While uncommon, gout is known to affect the SC joint. Joint aspirate will reveal negatively birefringent crystals under polarized light.
Rheumatoid Arthritis
In patients with rheumatoid arthritis, especially females, involvement of the SC joint is common.[14]
Seronegative Spondyloarthropathies
Conditions including psoriatic arthritis, ankylosing spondylitis, and reactive arthritis, notably seen in patients who are HLA-B27 positive, may involve the SC joint. SC joint involvement is much more common in psoriatic arthritis, with an incidence of 90% in severe cases. Treatment of these conditions revolves around non-steroidal anti-inflammatory drugs (NSAIDs) and disease-modifying agents.[15]
Synovitis-Acne-Pustulosis-Hyperostosis-Osteitis (SAPHO) Syndrome
In patients with SAPHO syndrome, the SC joint is the most common location of skeletal involvement. Radiographic imaging of the SC joint in patients with SAPHO syndrome will show evidence of inflammatory hyperostosis on a CT scan and a "bull's horn" appearance on a bone scan. This condition is treated primarily with NSAIDs, steroids, bisphosphonates, and sulfasalazine.[16]
Condensing Osteitis
Condensing osteitis is a rare condition that presents with a painful and swollen SC joint. Abduction of the arm may exacerbate the pain. Radiographic evaluation reveals sclerosis of the inferomedial end of the clavicle without signs of bone damage. Histological examination of affected bone reveals reinforcement of cancellous bone and destruction of marrow spaces, and radionucleotide scanning will show increased uptake. NSAIDs are the mainstay of treatment.[17]
Friedreich Disease
Friedreich disease involves avascular necrosis of the medial end of the clavicle. This condition can present with symptoms similar to those of condensing osteitis. A key differentiating factor between the two conditions is the duration of symptoms. Friedreich disease typically presents with a shorter duration of clinical symptoms. Additionally, Friedreich disease is predominantly seen in adolescent and pediatric patients. Histological examination of bone in a patient with this condition will reveal bone necrosis, marrow, and Haversian canal fibrosis with empty lacunae. Both Friedreich disease and condensing osteitis are treated with NSAIDs.[17]
Other Issues
Imaging Considerations
The sternoclavicular joint is best imaged utilizing computed tomography (CT) scanning for three-dimensional analysis. This technique is appropriate since it is based on a very sophisticated approach to x-ray technology; this makes it very good for visualizing the anatomy and pathology of bones. Magnetic resonance imaging (MRI) may also be used to analyze the articulating surfaces, fibrocartilaginous articulate disc, and supporting ligaments of the SC joint.
The presence of a musculus interclavicularis anticus digastricus has been reported.[18] This muscle variant originates from the manubrium of the sternum and inserts onto both clavicles. Both muscle bellies were attached by a tendon. The muscle receives innervation from the lateral pectoral nerve. The incidence of occurrence of this muscular variant is unknown at this time. This muscle is vulnerable to injury when inserting a catheter in the subclavian vein. Fractures of the clavicle could also damage such a muscle.
Media
(Click Image to Enlarge)
References
Cowan PT, Mudreac A, Varacallo M. Anatomy, Back, Scapula. StatPearls. 2023 Jan:(): [PubMed PMID: 30285370]
Kawagishi K, Tokumine J, Lefor AK. The Relationship of the Subclavius Muscle with Relevance to Venous Cannulation below the Clavicle. Anesthesiology research and practice. 2016:2016():6249483. doi: 10.1155/2016/6249483. Epub 2016 Feb 7 [PubMed PMID: 26966432]
Provencher MT, Bernholt DL, Peebles LA, Millett PJ. Sternoclavicular Joint Instability and Reconstruction. The Journal of the American Academy of Orthopaedic Surgeons. 2022 Aug 15:30(16):e1076-e1083. doi: 10.5435/JAAOS-D-19-00611. Epub 2022 May 2 [PubMed PMID: 35502995]
Thut D, Hergan D, Dukas A, Day M, Sherman OH. Sternoclavicular joint reconstruction--a systematic review. Bulletin of the NYU hospital for joint diseases. 2011:69(2):128-35 [PubMed PMID: 22035392]
Level 1 (high-level) evidenceKiel J, Ponnarasu S, Kaiser K. Sternoclavicular Joint Injury. StatPearls. 2023 Jan:(): [PubMed PMID: 29939671]
Hellwinkel JE, McCarty EC, Khodaee M. Sports-related sternoclavicular joint injuries. The Physician and sportsmedicine. 2019 Sep:47(3):253-261. doi: 10.1080/00913847.2019.1568771. Epub 2019 Jan 21 [PubMed PMID: 30644802]
Worman LW, Leagus C. Intrathoracic injury following retrosternal dislocation of the clavicle. The Journal of trauma. 1967 May:7(3):416-23 [PubMed PMID: 5337310]
Jain S, Monbaliu D, Thompson JF. Thoracic outlet syndrome caused by chronic retrosternal dislocation of the clavicle. Successful treatment by transaxillary resection of the first rib. The Journal of bone and joint surgery. British volume. 2002 Jan:84(1):116-8 [PubMed PMID: 11838442]
Level 3 (low-level) evidenceNakayama E, Tanaka T, Noguchi T, Yasuda J, Terada Y. Tracheal stenosis caused by retrosternal dislocation of the right clavicle. The Annals of thoracic surgery. 2007 Feb:83(2):685-7 [PubMed PMID: 17258018]
Level 3 (low-level) evidenceGardner MA, Bidstrup BP. Intrathoracic great vessel injury resulting from blunt chest trauma associated with posterior dislocation of the sternoclavicular joint. The Australian and New Zealand journal of surgery. 1983 Oct:53(5):427-30 [PubMed PMID: 6357176]
Level 3 (low-level) evidenceLawrence CR, East B, Rashid A, Tytherleigh-Strong GM. The prevalence of osteoarthritis of the sternoclavicular joint on computed tomography. Journal of shoulder and elbow surgery. 2017 Jan:26(1):e18-e22. doi: 10.1016/j.jse.2016.04.029. Epub 2016 Jul 14 [PubMed PMID: 27424249]
Dobson M, Waldron T. SCJ osteoarthritis: The significance of joint surface location for diagnosis. International journal of paleopathology. 2019 Mar:24():48-51. doi: 10.1016/j.ijpp.2018.08.010. Epub 2018 Oct 1 [PubMed PMID: 30278426]
Schipper P, Tieu BH. Acute Chest Wall Infections: Surgical Site Infections, Necrotizing Soft Tissue Infections, and Sternoclavicular Joint Infection. Thoracic surgery clinics. 2017 May:27(2):73-86. doi: 10.1016/j.thorsurg.2017.01.001. Epub [PubMed PMID: 28363376]
Nakamura H, Shibata Y, Takeda T. Sternoclavicular Joint Swelling in a Patient with Rheumatoid Arthritis. The Journal of rheumatology. 2016 Nov:43(11):2074-2075 [PubMed PMID: 27803344]
Emery RJ, Ho EK, Leong JC. The shoulder girdle in ankylosing spondylitis. The Journal of bone and joint surgery. American volume. 1991 Dec:73(10):1526-31 [PubMed PMID: 1748701]
Henriques CC, Sousa M, Panarra A, Riso N. The dark side of SAPHO syndrome. BMJ case reports. 2011 Dec 21:2011():. doi: 10.1136/bcr.11.2011.5197. Epub 2011 Dec 21 [PubMed PMID: 22670011]
Level 3 (low-level) evidenceGreenspan A, Gerscovich E, Szabo RM, Matthews JG 2nd. Condensing osteitis of the clavicle: a rare but frequently misdiagnosed condition. AJR. American journal of roentgenology. 1991 May:156(5):1011-5 [PubMed PMID: 2017922]
Roesler MK, Schmeisser MJ, Schumann S. Interclavicularis anticus digastricus muscle in a female body donor: a case report. Surgical and radiologic anatomy : SRA. 2022 Jan:44(1):93-97. doi: 10.1007/s00276-021-02848-w. Epub 2021 Oct 9 [PubMed PMID: 34626203]
Level 3 (low-level) evidence