Introduction
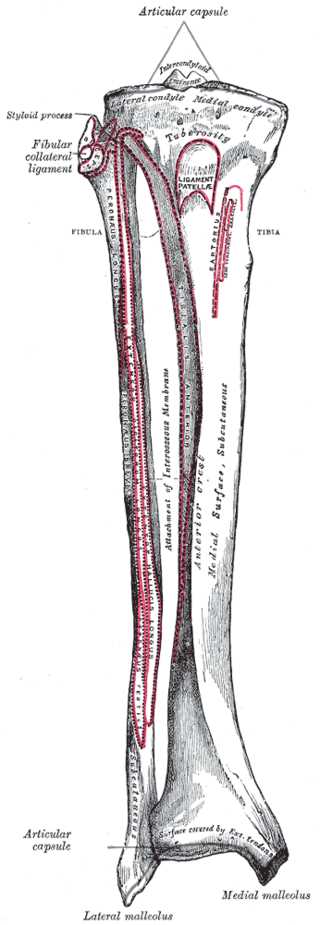
The tibia is one of two bones that comprise the leg.[1] As the weight-bearing bone, it is significantly larger and stronger than its counterpart, the fibula. The tibia forms the knee joint proximally with the femur and forms the ankle joint distally with the fibula and talus. The tibia runs medial to the fibula from just below the knee joint to the ankle joint and is connected to the fibula by the interosseous membrane.[2]
The proximal portion of the tibia consists of a medial and lateral condyle, which combine to form the inferior portion of the knee joint. Between the two condyles lies the intercondylar area, which is where the anterior collateral ligament, posterior collateral ligament, and menisci all have attachments.
The shaft of the tibia is triangular in cross-section with three borders and three surfaces. [3] The three borders as the anterior, medial, and interosseous and the three surfaces are the lateral, medial (anterior), and posterior. The anterior border divides the medial and lateral surface, the medial border divides the medial and posterior surface, and the interosseous border divides the lateral and posterior surface. While the medial surface is mostly subcutaneous, the lateral surface abuts the anterior compartment of the leg, and the posterior surface abuts the posterior compartment.
The distal portion of the tibia is shaped like a box with a distal medial protuberance that makes up the medial malleolus.[4] There are five surfaces that make up the distal tibia.
- The inferior surface provides a smooth articulation with the talus.
- The anterior surface is covered by extensor tendons and provides an area for ankle joint capsule attachment.
- The posterior surface has a groove for the tibialis posterior muscle.
- The lateral surface has a fibular notch which serves as an attachment for the interosseous membrane.
- The medial surface is a large bony prominence that makes up the medial malleolus.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
As the second-largest bone in the body, the tibia's main function in the leg is to bear weight with the medial aspect of the tibia bearing the majority of the weight load. [5]It also serves as the origin or insertion site for 11 muscles; these allow for extension and flexion at the knee joint and dorsiflexion and plantarflexion at the ankle joint.
Tibial Osteology
The Proximal Tibia:
- Lateral condyle - lateral proximal aspect of the tibia that articulates with the femur
- Medial condyle - medial proximal aspect of the tibia that articulates with the femur
- Lateral tibial plateau - the superior articular surface of the lateral condyle
- Medial tibial plateau - the superior articular surface of the medial condyle
- Intercondylar area
- Anterior area: located anteriorly between the medial and lateral condyle. The attachment point of the anterior cruciate ligament.
- Posterior area: located posteriorly between the medial and lateral condyle. The attachment point of the posterior cruciate ligament.
- Intercondyloid eminence (tibial spine): located between the articular facets and consists of a medial and lateral tubercle. The depression posterior to the intercondyloid eminence serves as attachments for the cruciate ligaments and menisci.
The Tibial Shaft:
- The shaft of the tibia is prism-shaped and has 3 surfaces (lateral, medial/anterior, and posterior) and 3 borders (anterior, medial, and interosseous).
- Anterior border: divides the medial and lateral surface
- Medial border: divides the medial and posterior surface
- Interosseous border: divides the lateral and posterior surface
- Medial/anterior surface: palpable down the lower leg, commonly referred to as the shin. It contains the tibial tuberosity.
- Tibial tuberosity: bony protrusion of the anterior tibia where the patellar ligament inserts
- Lateral surface: serves as the border and attachment of the interosseous membrane which connects the tibia and fibula.
- Posterior surface: Contains the soleal line
- Soleal line: oblique line located on the posterior tibia and serves as the origin for the soleus, flexor digitorum longus, and tibialis posterior muscles.
- Serves as the origin or insertion point of many muscles including tibialis anterior, extensor digitorum longus, soleus, tibialis posterior, flexor digitorum longus, sartorius, gracilis, quadriceps femoris, semimembranosus, semitendinosus, and popliteus muscles. [3]
The Distal Tibia:
-
The distal portion of the tibia is shaped like a box. [4] There are five surfaces that make up the distal tibia.
- The inferior surface provides a smooth articulation with the talus.
- The anterior surface is covered by extensor tendons and provides an area for ankle joint capsule attachment.
- The posterior surface has a groove for the tibialis posterior muscle.
- The lateral surface has a fibular notch which serves as an attachment for the interosseous membrane.
- The medial surface is a large bony prominence that makes up the medial malleolus.
- Medial malleolus: distal protrusion of the tibia which articulates with the talus
- Groove for the tendon of tibialis posterior is located on the posterior aspect of the medial malleolus
- Fibular notch: location of the tibiofibular joint
Embryology
The tibia has three ossification centers: one for the diaphysis and one for each epiphysis. It begins in the shaft at around the seventh week in utero. The proximal ossification center starts at birth and closes at age 16 in females and age 18 in males.[6] The distal ossification center starts at age one and closes at age 15 in females and age 17 in males.
Blood Supply and Lymphatics
The nutrient artery and periosteal vessels supply the blood to the tibia. The nutrient artery arises from the posterior tibial artery and enters the bone posteriorly distal to the soleal line. The periosteal vessels stem from the anterior tibial artery.[7]
Nerves
The nerves that supply the tibia are all branches of the main nerves that supply adjacent compartments.[8] In the posterior compartment of the leg, the tibial nerve gives off branches that supply the posterior aspect of the tibia, and in the anterior compartment of the leg, the deep fibular nerve gives off branches that supply the anterior aspect of the tibia.
Muscles
Muscles Inserting on the Tibia
- Tensor fasciae latae inserts on the lateral tubercle of the tibia, which is known as the Gerdy tubercle
- Quadriceps femoris inserts anteriorly on the tibial tuberosity
- Sartorius, gracilis, and semitendinosus insert anteromedially on the pes anserinus
- Horizontal head of semimembranosus muscle inserts on the medial condyle
- Popliteus inserts on the soleal line of the posterior tibia
Muscles Originating at the Tibia
- Tibialis anterior originates at the upper two-thirds of the lateral tibia
- Extensor digitorum longus originates at the lateral condyle of the tibia
- Soleus and flexor digitorum longus originate at the posterior aspect of the tibia on the soleal line
Physiologic Variants
One of the physiologic variants involving the tibia is a ball and socket ankle joint as opposed to the normal hinged ankle joint. In this variant, the distal tibia is concave and articulates with a rounded superior talus.[9]
Surgical Considerations
Management of Tibial Fractures
Tibial plateau fracture: These fractures present with knee pain and effusion. They classically occur after a car hits a pedestrian's fixed knee, which is known as a "bumper fracture." They are classified using the Schatzker classification and managed by using nonsurgical or surgical methods to achieve stable alignment. Operative strategies include external fixation and open reduction internal fixation.[10]
- Schatzker Classification
- Type 1: lateral split fracture
- Type 2: lateral split-depressed fracture
- Type 3: lateral pure depression fracture
- Type 4: medial fracture
- Type 5: bicondylar fracture
- Type 6: metaphyseal-diaphyseal disassociation
Tibial shaft fracture: Compared to most long bone fractures, tibial shaft fractures are more likely to be open because the medial surface is adjacent to the subcutaneous tissue. The fracture can have a low or high energy pattern. The low energy patterns are a result of torsional injury resulting in a spiral fracture. The high energy pattern is from a direct force that causes a wedge or oblique fracture. Nonoperative treatment is chosen for low-energy fractures that are minimally displaced while operative treatment is indicated for high-energy fractures including external fixation, intramedullary nailing, and percutaneous locking plate. These fractures can lead to extensive soft tissue injury, compartment syndrome, malunion, and bone loss. [11]
Ankle fractures involving the distal tibia: These injuries generally present with ankle pain and swelling and an inability to bear weight. They are usually the result of severe inversion or eversion of the ankle joint. The Lauge-Hansen and Danis-Weber classifications are commonly used to determine the type of fracture. There are also several specific distal tibial fractures that have their own name. The Pilon fracture involves the distal tibia and its articular surface with the ankle joint, and the Tillaux fracture involves the anterolateral distal tibial epiphysis. Distal tibial fractures are most commonly treated with open reduction and internal fixation.[12],[13]
- Lauge-Hansen Classification
- Supination-adduction
- Supination-external rotation
- Pronation-abduction
- Pronation-external rotation
- Danis-Weber classification
- Type A: fracture of lateral malleolus distal to the syndesmosis
- Type B: fracture of the fibula at the level of syndesmosis
- Type C: fracture of the fibula proximal to syndesmosis
Clinical Significance
Medial Tibial Stress Syndrome
Medial tibial stress syndrome, also known as shin splints, presents as generalized, recurrent pain in the lower part of the tibia. While the exact mechanism is unknown, it is thought to be due to biomechanical imbalances that result in too much force on the tibia. It is most commonly seen in runners and aerobic dancers, who often overload their legs with a large amount of force. It is commonly associated with the female athlete triad of amenorrhea, insufficient caloric intake, and osteoporosis. Medial tibial stress syndrome can be diagnosed by reproducing tenderness with palpation over a large area of the distal, medial tibia. The pathophysiology is traction periostitis. Treatment generally involves rest and ice until the pain improves and then gradually reintroducing activity.[14]
Apophysitis of the Tibial Tubercle
Apophysitis of the tibial tubercle, also known as Osgood-Schlatter disease, presents as pain below the knee that increases with activity and is relieved by rest. It is due to overuse of the knee and excess physical stress on where the patellar tendon inserts on the tibia; this causes repeated tension on the epiphyseal plate of the proximal tibia.[3] It is most often seen in males between the ages of 10 and 15. Diagnosis is usually made clinically, and there can be a palpable bony prominence at the tibial tuberosity, which can persist even after the pain resolves. Treatment includes rest and ice to decrease inflammation and avoidance of high impact activities like jumping. Symptoms usually resolve when the epiphyseal plates close.[15]
IO Access
Interosseous access is used in emergency care when vascular access cannot be obtained successfully. The method accesses the bone marrow of long bones which have a rich venous plexus that feeds into the systemic circulation. The tibia is commonly used as an IO access point. The proximal tibia is the most common location followed by the distal portion. Another commonly used bone is the proximal humerus. [16]
Other Issues
One of the most serious complications of a tibial fracture is compartment syndrome, which can lead to necrosis of the leg if not treated with urgent surgery.[17]
Media
(Click Image to Enlarge)
References
Hadeed MM, Post M, Werner BC. Partial Fibular Head Resection Technique for Snapping Biceps Femoris. Arthroscopy techniques. 2018 Aug:7(8):e859-e862. doi: 10.1016/j.eats.2018.04.008. Epub 2018 Jul 23 [PubMed PMID: 30167365]
Gupton M, Munjal A, Kang M. Anatomy, Bony Pelvis and Lower Limb: Fibula. StatPearls. 2023 Jan:(): [PubMed PMID: 29261984]
Puzzitiello RN, Agarwalla A, Zuke WA, Garcia GH, Forsythe B. Imaging Diagnosis of Injury to the Anterolateral Ligament in Patients With Anterior Cruciate Ligaments: Association of Anterolateral Ligament Injury With Other Types of Knee Pathology and Grade of Pivot-Shift Examination: A Systematic Review. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2018 Sep:34(9):2728-2738. doi: 10.1016/j.arthro.2018.04.025. Epub 2018 Jul 20 [PubMed PMID: 30037574]
Level 1 (high-level) evidenceJuneja P, Hubbard JB. Anatomy, Bony Pelvis and Lower Limb: Tibialis Anterior Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 30020676]
Bandovic I, Holme MR, Black AC, Futterman B. Anatomy, Bone Markings. StatPearls. 2023 Jan:(): [PubMed PMID: 30020631]
Hsu H, Siwiec RM. Knee Arthroplasty. StatPearls. 2023 Jan:(): [PubMed PMID: 29939691]
NELSON GE Jr, KELLY PJ, PETERSON LF, JANES JM. Blood supply of the human tibia. The Journal of bone and joint surgery. American volume. 1960 Jun:42-A():625-36 [PubMed PMID: 13854090]
Guerra-Pinto F, Côrte-Real N, Mota Gomes T, Silva MD, Consciência JG, Monzo M, Oliva XM. Rotational Instability after Anterior Talofibular and Calcaneofibular Ligament Section: The Experimental Basis for the Ankle Pivot Test. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2018 Nov-Dec:57(6):1087-1091. doi: 10.1053/j.jfas.2018.03.038. Epub 2018 Aug 23 [PubMed PMID: 30146335]
Jastifer JR, Gustafson PA, Labomascus A, Snoap T. Ball and Socket Ankle: Mechanism and Computational Evidence of Concept. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2017 Jul-Aug:56(4):773-775. doi: 10.1053/j.jfas.2017.02.019. Epub [PubMed PMID: 28633775]
Zeltser DW, Leopold SS. Classifications in brief: Schatzker classification of tibial plateau fractures. Clinical orthopaedics and related research. 2013 Feb:471(2):371-4. doi: 10.1007/s11999-012-2451-z. Epub [PubMed PMID: 22744206]
Grütter R, Cordey J, Bühler M, Johner R, Regazzoni P. The epidemiology of diaphyseal fractures of the tibia. Injury. 2000 Sep:31 Suppl 3():C64-7 [PubMed PMID: 11052384]
Hunter TB, Peltier LF, Lund PJ. Radiologic history exhibit. Musculoskeletal eponyms: who are those guys? Radiographics : a review publication of the Radiological Society of North America, Inc. 2000 May-Jun:20(3):819-36 [PubMed PMID: 10835130]
Russo A, Reginelli A, Zappia M, Rossi C, Fabozzi G, Cerrato M, Macarini L, Coppolino F. Ankle fracture: radiographic approach according to the Lauge-Hansen classification. Musculoskeletal surgery. 2013 Aug:97 Suppl 2():S155-60. doi: 10.1007/s12306-013-0284-x. Epub 2013 Aug 15 [PubMed PMID: 23949937]
Galbraith RM, Lavallee ME. Medial tibial stress syndrome: conservative treatment options. Current reviews in musculoskeletal medicine. 2009 Oct 7:2(3):127-33. doi: 10.1007/s12178-009-9055-6. Epub 2009 Oct 7 [PubMed PMID: 19809896]
Whitmore A. Osgood-Schlatter disease. JAAPA : official journal of the American Academy of Physician Assistants. 2013 Oct:26(10):51-2. doi: 10.1097/01.JAA.0000435006.47717.41. Epub [PubMed PMID: 24201924]
Tan BK, Chong S, Koh ZX, Ong ME. EZ-IO in the ED: an observational, prospective study comparing flow rates with proximal and distal tibia intraosseous access in adults. The American journal of emergency medicine. 2012 Oct:30(8):1602-6. doi: 10.1016/j.ajem.2011.10.025. Epub 2012 Jan 12 [PubMed PMID: 22244227]
Kiel J, Kaiser K. Tibial Anterior Compartment Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 30085512]