Introduction
An anal fistula (anorectal fistula) is one of the most common colorectal issues in the U.S.[1] An anal or anorectal fistula is an inflammatory tract or connection between the anal canal and the perianal skin. Classic anal fistulas are the result of a perineal infection and abscess formation. These infections arise from the anal glands, which form a cryptoglandular abscess at the dentate line and then communicate outward to the perianal skin. The abscess or infections can spontaneously drain externally or be drained by a surgical incision and drainage procedure. After the drainage, a chronic tract can form that will intermittently drain or become infected again.
Hidradenitis suppurativa, trauma, malignancy, tuberculosis, and Crohn disease can all express as fistulas as well, although these present as atypical fistulas. Initial treatment for all perianal pain and presumed perineal infections is an exam under anesthesia and drainage of the abscess. Over time the abscess should heal, and if there is continued drainage from a punctum or nodule at the perianal skin, then a fistula is presumed. There are multiple types of fistula tracts related to the anatomy through which the fistula courses. The fistula tract can either be deep or superficial to the external anal sphincter. The superficial tracts can simply be opened or unroofed with a fistulotomy to the anal gland, and the tract will heal by secondary intention. The deeper fistulas encompass more of the external anal sphincter and cannot be unroofed as that leads to fecal incontinence. Instead, these tracts should have a Seton (elastic band or heavy suture) placed through the tract, and this allows a slow process to cut through the tract as the deeper parts heal so that incontinence is less likely. A final option for chronic fistulas is a flap closure of the tract with advancement flaps.[2]
Patients with complex fistulas pose a challenge to the surgeon. Malignant fistulas will need an interprofessional team approach to rectal and anal cancers, which will involve chemotherapy and radiation therapy.[3] Setons may be used as an adjunct to allow drainage so that abscess formation would not compromise patient care plans. Patients with Crohn disease who have fistula are a challenge. Setons would be the first line of therapy to make sure no abscess or perineal sepsis develops, then adjunct medication like steroids and Infliximab may be used chronically to assist remission of the disease and healing of the fistula tract(s).[4][5][6] Hidradenitis suppurative and tuberculosis should be treated with antibiotics, and Setons are adjuncts to make sure the fistulas do not form abscesses during treatment. In some cases, the perineal fistula disease is so severe that fecal diversion with a colostomy assists healing and control of continued perineal infections.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
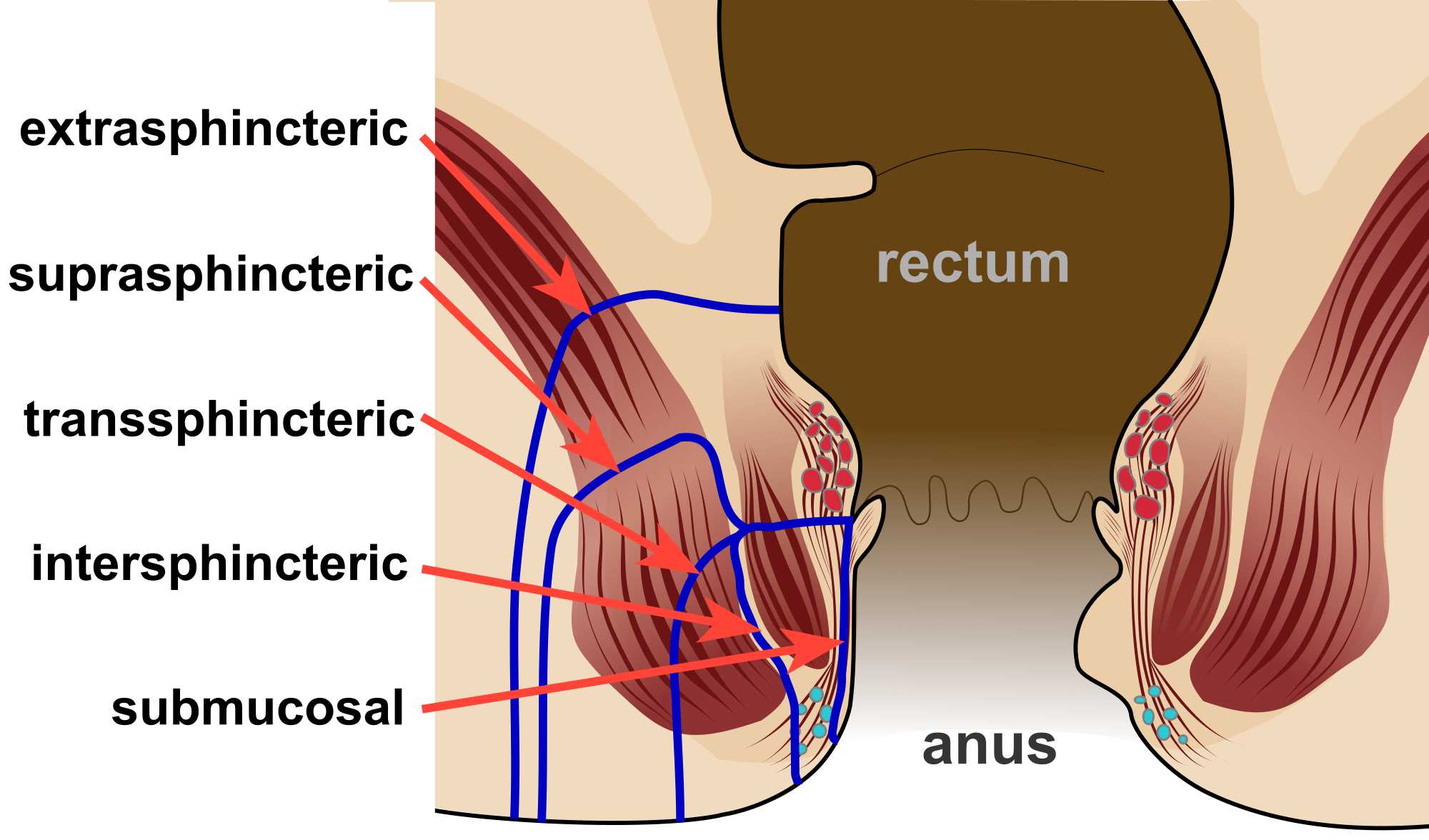
The anal sphincter complex is comprised of the internal and external anal sphincters. The external sphincter is a striated muscle complex encircling the anus and is under voluntary control. The internal sphincter is a circular muscle closer to the interior of the anal canal and is under involuntary control. There are four main types of fistula in ano.
- Intersphincteric: The most common is an intersphincteric located between the two muscles with the external opening close to the anus.
- Trans-sphincteric: This fistula traverses the external sphincter and is open more lateral and associated with horseshoe type abscesses.
- Suprasphincteric: This fistula passes above the puborectalis muscle tracking laterally near the levator ani.
- Extrasphincteric: The least common fistula is extrasphincteric, which traverses the ischiorectal fossa and the levator ani then into the rectal wall superior to the dentate line.
Based on the origin of the anorectal fistula development from cryptoglandular abscesses, the internal opening of most fistulas is located at the dentate line. The type of fistula is most commonly diagnosed at an anorectal examination under anesthesia, where anoscopy or flexible sigmoidoscopy can be performed at the time of fistula tract exploration. The decision of which structures the fistula connection incorporates, i.e., internal and external sphincter complex is important as only a small amount of external sphincter muscle that can be cut.[7] Up to 30% of the external sphincter muscle can be cut without compromising fecal continence. To avoid the cutting of too much external sphincter and to decrease the risk of fecal incontinence as well as to allow adequate drainage following abscess drainage, a Seton can be placed through the tract. Seton can either be utilized to slowly cut through the sphincter muscle over time, called 'cutting Seton.' Setons can also be placed into fistula tracks to allow previously undrained collections to heal around the seton slowly, called a 'non-cutting Seton.' In addition to the depth of the fistula, there are certain clues as to where the fistula tract originates from the location of the external opening. This is from Goodsall's rule, which states that if a transverse line is drawn across the anus, a fistulous external opening which is anterior to this line and will be located internally 3 cm of the anal verge, with the fistulas tract radially and directly into the anal canal. However, if the external opening is posterior to this line or outside of the 3 to 4 cm area from the anal verge, then these fistulas tend to arc around to the posterior midline anal gland. These arching fistula tracts are sometimes difficult to completely discern at the first operation, so the tract can be partially unroofed towards to anal verge being careful to avoid the destruction of the external anal sphincter. Although Goodsall's rule has been taught for years, there are some challenges to this rule recently; however, for simple fistulas, it is a good starting point.[8]
Indications
In general, most patients have a prior history of perianal abscess, which was either drained by a physician or drained spontaneously. The area in which the drainage occurred, there is chronic drainage, which remains weeks to months later. The area occasionally flares with pain and increased drainage, and the patient presents with this chronic draining sinus tract. The diagnosis is usually made with history and examination of the perineum. This is considered an elective case, and the procedure is offered to the patient as an exam under anesthesia and fistulotomy or Seton placement. It is important to pre-operatively ask about any history or family history of Crohn disease as well as fecal incontinence. In patients with Crohn disease, as well as females with an anterior fistula, they are best served with a non-cutting Seton placement and not a fistulotomy. If there is uncertainty in the depth of the tract, a Seton is also a safer option.
Contraindications
There are few contraindications to the Seton placement. Active infection and abscess should be drained at the initial procedure, and if the tract identified, then a Seton may also be placed. If the internal opening if found to be cancer, then this scenario would mandate an oncologic treatment for the patient and further workup and management. Both acute and chronic fistula tracts may be treated with a Seton regardless of additional pathology found. Superficial fistula tracts are most expeditiously treated with a simple fistulotomy if the tract involves the posterior area and small amount of sphincter muscle. Anterior fistula tracts, especially in females, those in patients with prior fecal incontinence and those with Crohn disease should not undergo fistulotomy as incontinence rates are high. For this group of patients, following Seton placement, follow-up with colorectal specialists for more complex surgical therapies is recommended.
Equipment
The procedure is performed in the operating room, under general anesthesia or adequate sedation. The patient is placed either in a prone or lithotomy position depending on the anticipated tract and its source anterior or posterior in the anus. The surgeons will require an anal retractor set. For the Seton, a vessel loop, heavy nylon suture, or rubber band can be utilized. To locate the tract, the surgeon will need an anal probe such as a lacrimal duct probe and possibly a small 10 cc syringe with some hydrogen peroxide with an angiocatheter on it to inject into the fistula tract. The surgeon may use a local analgesia injection at the end of the case to help with postoperative pain control. The perineal dressing to aid with the management of post-surgical drainage will be applied at the end of the case.
Personnel
The procedure is usually performed with one surgeon and an assistant. The assistant holds the anal retractor to be able to see in the internal opening and to hold the Seton for suturing the two ends together.
Preparation
The Seton procedure requires essentially no patient preparation though some prefer a single enema the morning of the procedure to clean stool from the rectal vault. The rest of the preparation is with positioning in the operating room and making sure the instruments are present, and the Seton material of choice is present. Perioperative prophylactic antibiotics to cover the coliforms may be considered.
Technique or Treatment
The procedure is performed in the operating room, with anesthesia providing sedation, and some surgeons may prefer general anesthesia. The patient is placed either in a prone or lithotomy position depending on the anticipated tract and its source anterior or posterior in the anus. If the anticipated tract is anterior in the anus, then prone is preferred and the lithotomy position for the posterior midline tracts. This positioning makes the internal opening more visible for the surgeon and the tract more accessible. The fistula probe (lacrimal duct probes) are usually required to explore the tract and its trajector, and most of the time, with chronic fistulas, the probe can be used to find the internal opening easily. If the tract is difficult to locate, then hydrogen peroxide can be injected gently in the external opening (utilizing the syringe with angiocatheter to enter the external opening), and with an anal retractor, the peroxide can be seen bubbling from the internal opening. This maneuver allows the surgeon to demonstrate where the tract would be using the probe.[9] Once the tract has the probe through it, then a vessel loop, a heavy 1 nylon suture, or a thick rubber band can be attached to the probe and brought through the tract. Both ends of the Seton are sewn together in a couple of areas close together, so the loop to prevent it from falling out. If a cutting seton is selected, then the Seton is gradually tightened externally over weeks. If a non-cutting seton is utilized, the Seton is usually fashioned from a vessel loop or other smooth non-reactive product and left loose. If the tract cannot be located, the surgeon should not force a tract at the risk of creating a false tract. If the tract cannot be located, the surgeon may work to unroof the external opening as close to the anal verge as possible and make plans for a repeat anorectal examination under anesthesia in the operating room in the following weeks. In the meantime, the surgeon may opt for a CT scan or MRI of the pelvis with rectal contrast to see if the tract can be identified. The surgeon may use local anesthesia for postoperative pain management. Perineal dressings are then applied. The surgeon should dictate a meticulous operative note as to the depth of the tract, the site of internal and external openings as well as the plan for the Seton.[10]
Complications
The procedure has a few complications. Specific to this procedure is the failure to locate and drainage an abscess or to locate the fistula tract. There is also the risk of creating a false fistula tract. There is some leakage of stool with the Seton, and instructions for cleaning should be given. There may be some bleeding from the raw tract, and this should be minor. Infections are uncommon, but if they occur, this should prompt either another exam under anesthesia or oral antibiotics if not severe, or IV antibiotics and exploration if severe such as a perineal necrotizing infection. Incontinence is rare with the Seton placement. If the internal opening is not identified, then a recurrence of the fistula in a more complex form may occur.
Clinical Significance
Fistula in ano is usually a consequence of a prior perianal abscess, which either spontaneously drained or required surgical drainage. De novo fistula in ano, often portend another cause like Crohn disease or hidradenitis or even perineal cancer and should be examined and questioned thoroughly. Females with anterior fistula sites that may occur with childbirth. They should anticipate a Seton placement. General surgeons may treat simple fistulas; however, the more complex fistulas should seek colorectal surgeon referral for optimal care.[11]
Enhancing Healthcare Team Outcomes
Fistula in ano is a sequella of perianal abscess that appears to be a simple diagnosis and requires surgical treatment. There is no role for antibiotics for a fistula if the abscess is drained. Surgical exploration is required to delineate the fistula tract and to drain any undrained abscesses associated with the formation of the tract. Treatment can be either with fistulotomy or Seton placement (cutting vs. non-cutting) and is best assessed by an experienced surgeon or colorectal surgeon. They are best served with an interprofessional approach with gastrointestinal physicians experienced in Crohn disease, gynecologists, plastic surgeons, surgical oncologists, and colorectal surgeons who can evaluate the whole perineum of the patient, and make sure systemic therapy or oncologic therapies are employed.
Media
(Click Image to Enlarge)
References
Cariati A. Fistulotomy or seton in anal fistula: a decisional algorithm. Updates in surgery. 2013 Sep:65(3):201-5. doi: 10.1007/s13304-013-0216-1. Epub 2013 Jun 2 [PubMed PMID: 23729353]
Level 2 (mid-level) evidenceTurner JS, Okonkwo A, Chase A, Clark CE. Early outcomes of fluorescence angiography in the setting of endorectal mucosa advancement flaps. Techniques in coloproctology. 2018 Jan:22(1):25-30. doi: 10.1007/s10151-017-1732-7. Epub 2017 Dec 18 [PubMed PMID: 29256139]
Au J, Hulme-Moir FM, Herd A, Kozman MA. Extensive Resection for Treatment of Locally Advanced Primary Mucinous Adenocarcinoma Arising From Fistula-in-Ano. Annals of coloproctology. 2021 Jul:37(Suppl 1):S7-S10. doi: 10.3393/ac.2019.11.19. Epub 2019 Nov 26 [PubMed PMID: 32054254]
Papaconstantinou I, Kontis E, Koutoulidis V, Mantzaris G, Vassiliou I. Surgical Management of Fistula-in-ano Among Patients With Crohn's Disease: Analysis of Outcomes After Fistulotomy or Seton Placement-Single-Center Experience. Scandinavian journal of surgery : SJS : official organ for the Finnish Surgical Society and the Scandinavian Surgical Society. 2017 Sep:106(3):211-215. doi: 10.1177/1457496916665763. Epub 2016 Aug 22 [PubMed PMID: 27550245]
Banasiewicz T, Eder P, Rydzewska G, Reguła J, Dobrowolska A, Durlik M, Wallner G. Statement of the expert group on the current practice and prospects for the treatment of complex perirectal fistulas in the course of Crohn's disease. Polski przeglad chirurgiczny. 2019 Feb 25:91(1):38-46. doi: 10.5604/01.3001.0013.0593. Epub [PubMed PMID: 30919811]
Hyder SA, Travis SP, Jewell DP, McC Mortensen NJ, George BD. Fistulating anal Crohn's disease: results of combined surgical and infliximab treatment. Diseases of the colon and rectum. 2006 Dec:49(12):1837-41 [PubMed PMID: 17041753]
Vogel JD, Johnson EK, Morris AM, Paquette IM, Saclarides TJ, Feingold DL, Steele SR. Clinical Practice Guideline for the Management of Anorectal Abscess, Fistula-in-Ano, and Rectovaginal Fistula. Diseases of the colon and rectum. 2016 Dec:59(12):1117-1133 [PubMed PMID: 27824697]
Level 1 (high-level) evidenceJayarajah U, Samarasekera DN. Predictive accuracy of Goodsall’s rule for fistula-in-ano. The Ceylon medical journal. 2017 Jun 30:62(2):97-99 [PubMed PMID: 28697591]
Gunawardhana PA, Deen KI. Comparison of hydrogen peroxide instillation with Goodsall's rule for fistula-in-ano. ANZ journal of surgery. 2001 Aug:71(8):472-4 [PubMed PMID: 11504291]
Gonzalez-Ruiz C, Kaiser AM, Vukasin P, Beart RW Jr, Ortega AE. Intraoperative physical diagnosis in the management of anal fistula. The American surgeon. 2006 Jan:72(1):11-5 [PubMed PMID: 16494174]
Holzheimer RG, Siebeck M. Treatment procedures for anal fistulous cryptoglandular abscess--how to get the best results. European journal of medical research. 2006 Dec 14:11(12):501-15 [PubMed PMID: 17182363]
Level 1 (high-level) evidence