Obesity Surgery Indications and Contraindications
Obesity Surgery Indications and Contraindications
Introduction
Obesity affects at least one-third of adults and 17% of youth in the United States and confers an increased risk of related comorbidities such as heart disease and type 2 diabetes. After many years of failed medical treatments for obesity, a variety of successful surgical treatments have evolved. Weight loss surgery has proven to be an effective cure for obesity, as well as a treatment for the secondary comorbidities. Extensive research demonstrates the long-term benefits of obesity surgery versus other non-invasive treatments in similar populations.[1][2][3]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Understanding the anatomical alterations the gastrointestinal tract undergoes, is the key to grasping the mechanism of action of weight loss surgery. Laparoscopic sleeve gastrectomy (LSG) and laparoscopic Roux-en-Y gastric bypass (LRYGB) are the 2 main types of surgeries that are current standards of care in weight loss surgery.
With LSG the less complex; the lower portion of the stomach is divided and removed from the patient. The new smaller stomach or “sleeve,” forces the patient to eat smaller portions, and consume fewer calories. Patients become full after smaller portions than they could previously tolerate because the stomach is a fraction of the size it was before surgery. In addition to this mechanical benefit from having a smaller stomach, researchers believe that there is a hormonal benefit. Several hormones that affect satiety and hunger are produced in the removed portion of the stomach. The combined effects of mechanical and chemical changes that take place in the digestive system following LSG lead to dramatic weight loss and cure in many patients.
The second type of surgery, LRYGB is a more involved procedure where the transit of food along the gastrointestinal (GI) tract is rerouted to achieve a change in the absorptive capacity for calories. The stomach is divided into a small pouch that connects to the small intestine further down the GI tract. This effectively creates a new path for food to travel in which the proximal portion of the small intestine is skipped or “bypassed,” meaning that portion of the bowel will never come into contact with that food and hence, fewer calories are absorbed.
Other proposed mechanisms of action that contribute to weight loss after RYGB are changed in the gut microbiota, bile acids, and energy expenditure. Although these have been observed in several animal models, it is unknown exactly how these changes lead to weight loss. At this point, these are associations that have not been proven to have causality. Abundant research has been conducted to try and replicate the chemical benefits of weight loss surgery, which has been relatively unsuccessful.[4][5][6]
Indications
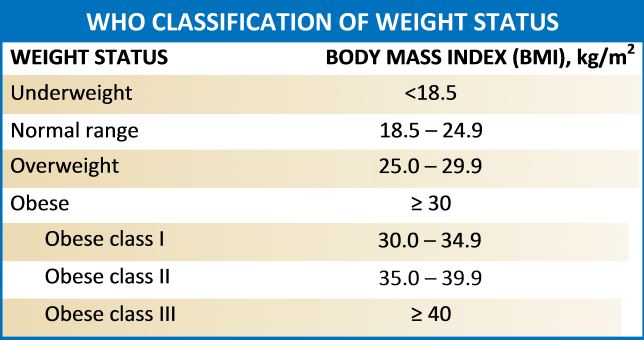
The indications to undergo bariatric surgery, are based on body mass index (BMI) as well as the presence of comorbidity. Patients with a BMI of 40 kg/m2 or greater without coexisting medical problems, and for whom bariatric surgery would not carry an excessive risk, should be candidates for one of the surgeries mentioned above.
Patients with a BMI greater than or equal to 35 kg/m2 and 1 or more severe obesity-related comorbidities, including type 2 diabetes, hypertension, hyperlipidemia, obstructive sleep apnea (OSA), non-alcoholic fatty liver disease (NAFLD), GERD, asthma, venous stasis disease, severe urinary incontinence, debilitating arthritis, or considerably impaired quality of life, would also qualify as surgical candidates. Patients with BMI OF 30 to 34.9 kg/m2 with diabetes or metabolic syndrome also may undergo weight loss surgery, although there is a lack of sufficient data to demonstrate long-term benefits in such patients.[7][8]
Contraindications
While there are no absolute contraindications to bariatric surgery, relative contraindications do exist. These include severe heart failure, unstable coronary artery disease, end-stage lung disease, active cancer treatment, portal hypertension, drug/alcohol dependency, and impaired intellectual capacity. In the case of LRYGB, Crohn’s disease is a relative contraindication. Furthermore, since these procedures are performed under general anesthesia, any contraindication to receiving general anesthesia would also be a contraindication for these surgeries.
Equipment
The equipment needed for both LSG and LRYGB includes surgical instruments and tools. These procedures are almost always performed using laparoscopy necessitating the usual laparoscopic instrumentation such as CO2 insufflation, trocars (portals to insert instruments into the abdomen through), cameras, and television monitors to see inside the abdomen.
Many laparoscopic instruments are used including needle drivers, non-traumatic bowel graspers, cautery devices, a liver retractor, a single-use specimen pouch that is designed to retrieve intra-abdominal specimens, suturing devices, shears, and various other tools designed for dissecting within the abdomen.
In addition, either the anesthesiologist or an assistant will stand at the patient’s head and introduce a bougie or an endoscope to define the borders for where to ligate stomach and bowel. This ensures that the lumen is not too narrow for food and liquid to pass through. Endoscopy also enables visualization of the GI tract from inside. This gives the team a chance to inspect the integrity of the staple/suture line and to perform a leak test in which air is insufflated into the new stomach or pouch.
After the sleeve or bypass is complete, the trocars (usually 5-6 ports) are removed, and an absorbable suture is used to close the fascia, subcutaneous tissue, and skin incisions. The skin incisions range from 5 to 12 mm, and skin glue or steri strips are used to cover the skin closure.
Personnel
The personnel required includes the usual operating room team of a nurse/circulator, a scrub tech responsible for preparing the surgical instruments, an anesthesiologist, a surgeon, and at least 1 or 2 surgical assistants such as residents, PAs, or students. Generally, one person controls the camera while the surgeon and an assistant perform the surgery.
Nursing is also required for both pre-operative care in the holding area and postoperative in the recovery area. These patients are generally admitted to the hospital following surgery for 1 to 2 days depending on the procedure they have and their post-operative condition.
Preparation
A great deal of planning is necessary to ensure a successful outcome for patients undergoing obesity surgery. A number of qualified medical professionals such as psychiatrists/psychologists, nutritionists, general practitioners, and social workers are integral to patient optimization. Patients often attend group classes designed to educate them on the lifestyle changes they will need to undergo, and what to expect before during and after surgery. The nutritional and psychological aspects of the surgery are equally as important as the technical details and physical changes the surgery entails. A 6-month process involving this interprofessional team of professionals is what patients considering obesity surgery should expect.
Technique or Treatment
While techniques for performing LRYGB and LSG have a fair amount of variation depending on surgeon preference and training, the objectives of these surgeries are relatively uniform.
Both surgeries begin by insufflating the abdomen to 12 to 15 mm Hg of CO2 to blow up the intra-abdominal space like a balloon. This can be done by either inserting a Veress needle or by direct trocar entry. This allows better visualization of the stomach and organs that need to be dissected. Next, the trocars are introduced through the patient’s abdominal wall by making 5 to 12 mm incisions with a scalpel and inserting ports, which serve as doorways to pass instruments into the abdomen through. A liver retraction device is placed through one of these holes usually sub-sternal, to expose the stomach and surrounding area. The arteries supplying the stomach are then divided using an instrument that seals and cuts tissues.
The remainder of the surgery differs between LRYGB and LSG with the former being more complex and technically difficult to perform. The next step in LRYGB is to measure a distance (generally 120 to 150 cm) from the beginning of the duodenum where the distal jejunum is divided with a stapler. The distal portion of the divided bowel is brought up to what will be a new stomach pouch (or mini stomach), and the 2 are eventually sewn together creating a new pathway for food transit such that food passes from the pouch directly into the downstream intestine. In effect, this so-called “Roux limb” bypasses all of the duodenum and intestines proximal to where the jejunum was divided and creates a shortcut for food to reach the downstream intestines.
In the next part of LRYGB, the proximal end of the divided intestine is connected further downstream (around 150 cm) to the distal jejunum so that biliary secretions and digestive enzymes can join the food and aid in digestion. This also ensures that digestive contents (which would otherwise have nowhere to go in the newly designed GI tract) travel in the right direction.
After confirming the integrity of the staple lines and ensuring that there is no leak, the CO2 is removed from the abdomen, and the ports are removed. The incisions are closed, and the patient awakes from anesthesia shortly after that.
LSG, by comparison, is a much simpler procedure. The lower portion of the stomach is divided with a stapler and is removed from the abdomen. No new routes, bypasses, or connections are created. The integrity of the staple line is inspected as with LRYGB, a leak test is performed, and the surgery is completed using all the same basic steps as previously described. The types of stapling devices used, over-sewing techniques, and methods of conducting these surgeries vary according to surgeon preference and training. The results and physiologic changes, however, are relatively uniform no matter where these surgeries are performed.[9][10]
Complications
Complications of weight loss surgery can occur during surgery, in the immediate 1 to 2 days postoperatively, or even years after surgery. Intraoperative complications are rare and include anesthesia-related events, injury to bowels, spleen, liver, or damage to a major blood vessel such as the inferior vena cava (IVC) or portal vein. Bowel ischemia can also occur if the blood supply is disrupted inadvertently during stapling, suturing, or ligation. Injuries can happen during insertion of the trocars (which are sharp) into the abdomen, can be due to a technical error, or sometimes may be due to difficult or aberrant anatomy. The body habitus of this patient population, particularly the thickness of their abdominal walls, increases the level of difficulty of these surgeries. The risks of intraoperative complication seen are similar to that of any laparoscopic abdominal surgery. The comorbidities of these patients, however, predispose them to a slightly higher risk of complication when going under general anesthesia and having surgery. Nonetheless, these complications are rare and occur approximately 1% of the time. Myocardial infarction, deep vein thrombosis (DVT), pulmonary embolism, and hemorrhage are all extremely rare during weight loss surgery, but they do happen. LRYGB is associated with slightly higher occurrences of most of these complications. Conversion to an open procedure is also noted to carry an increased risk of complication.
The most common and dreaded postoperative complication is an anastomotic leak. This happens when there is leakage at the staple or suture line of the bowel or stomach, into the abdomen. When this occurs, it is usually within the first week after surgery. The classic presentation is unexplained tachycardia more than 120 bpm that does not resolve. Fever, respiratory difficulty, and abdominal pain may also be present. If not identified and treated promptly, the anastomotic leak can progress to sepsis and even death. Upper GI series can be used to diagnose the anastomotic leak, and in many bariatric centers, this is routinely performed on postoperative day 1 before initiating a bariatric diet. These leaks must be treated with surgery to revise the anastomosis and fix the leak. Initiation of intravenous (IV) antibiotics, percutaneous or laparoscopic drain placement, and making the patient nothing by mouth (NPO) are the standards of treatment for this complication.
Surgical site infection (SSI) is another complication with approximately 1% incidence in bariatric surgery. The use of perioperative antibiotics markedly decreases this risk as with other surgeries. Pulmonary embolism is the most common cause of death in the postoperative period following bariatric surgery. Again obesity is a factor that predisposes this population to this complication. Many surgeons routinely keep their bariatric patients on chemical thromboprophylaxis after surgery for as long as 1 month to mitigate this risk.
Internal hernias and marginal ulcers are complications that can present years after bariatric surgery. An internal hernia is when bowel extends into space within the abdominal cavity created inadvertently, in this case when reconstructing the GI tract during LRYGB. This is dangerous because bowel can become strangulated, ischemic, and/or obstructed. This is a surgical emergency, and if strongly suspected, warrants at minimum laparoscopic exploration with any necessary intervention to follow subsequently.
Marginal ulcers most often occur at the margin where small intestine is joined to the stomach pouch. These ulcers irritate the gastrointestinal mucosa and eventually can perforate which again is a surgical emergency, treated similarly to an anastomotic leak. Marginal ulcers have been attributed to the type of non-absorbable suture used, and many surgeons use absorbable sutures to prevent this.
The potential complications mentioned above are serious risks that both the surgeon and patient need to be aware of when planning weight-loss surgery. Bariatric centers for excellence have evolved and are required to have minimal complication rates after these surgeries, generally less than 5%. The surgeons that direct and operate within these centers have strict regimens, surgical techniques, and patient optimization that are designed to achieve success repeatedly.
Clinical Significance
Obesity is now regarded as a full-fledged disease and has reached epidemic proportions, which seem to be increasing. The evolution of bariatric surgery and the technologic innovation that has revolutionized this field offer a potential cure to these patients. Both LSG and LRYGB are options that have been proven to get consistent results for the right patients. Not every obese patient is a good candidate for these surgeries, and a variety of factors as mentioned above should be considered before electing to proceed with weight-loss surgery. While the risk of complication does exist, the overwhelming majority of these patients do very well, and often beat the disease and its associated comorbidities. Candidates for this surgery should be educated on this subject and should be made aware by their physicians that this option exists. Overall, the progress that this area of surgery has made over the past couple of decades is encouraging.
Enhancing Healthcare Team Outcomes
To achieve good results and avoid the complications, bariatric surgery needs an interprofessional team approach that consists of a surgeon, bariatric nurse, pharmacist, physiotherapist, dietitian, social worker, and a gastroenterologist. After the surgery, these patients need to have DVT prophylaxis and ambulation. At the same time, the nurse should monitor the patient was wound infection, respiratory difficulties, and ileus. A dietary consult is required to ensure that they consume the right foods to prevent mineral and vitamin deficiencies. All patients should be educated about the importance of lifestyle changes and participating in a regular exercise program. Pharmacists can consult on post-operative infection and pain control with the surgeon and nurse. In the follow-up period, the patients need to be assessed for flabby skin, pendulous breasts, or overhanging abdominal skin. These features can have a negative impact on cosmesis and hence, a referral to a plastic surgeon should be made.[11][12][13] (Level V)
Evidence-based Outcomes
There is no longer any question that bariatric surgery is effective and does help people lose weight. More important there is evidence showing that bariatric surgery can lower the risk of adverse cardiac events, diabetes, and stroke. Several studies have also shown that bariatric surgery can lower the risk of endometrial cancer in obese women undergoing weight loss surgery. In addition, bariatric surgery by reducing weight can decrease the intensity of low back pain and significantly improve the quality of life. Finally, there is evidence that in the long run bariatric surgery can help lower the cost of health care by lowering blood pressure, diabetes, hypercholesterolemia, and musculoskeletal disease compared to non-surgical methods of weight loss. Unfortunately, there are not many long-term studies that have determined if the benefits of bariatric surgery are sustained or if the patients regain the weight. Anecdotal reports indicate that some patients who do not change their lifestyle quickly regain weight. Finally, it should not be forgotten that bariatric surgery is also associated with several post-surgical complications that cannot only prolong hospital stay but can also increase mortality. In institutions that specialize in bariatric surgery, mortality rates of less than 3% have been stated, but in hospitals where the procedures are not frequently done, the mortality rates are slightly higher.[14][15][16] (Level V)
Media
(Click Image to Enlarge)
References
Herrera MF, García-García E, Arellano-Ramos JF, Madero MA, Aldrete-Velasco JA, Corvalá JAL. Metabolic Surgery for the Treatment of Diabetes Mellitus Positioning of Leading Medical Associations in Mexico. Obesity surgery. 2018 Nov:28(11):3474-3483. doi: 10.1007/s11695-018-3357-y. Epub [PubMed PMID: 29915971]
Liang H, Lin S, Guan W. [Choice of bariatric and metabolic surgical procedures]. Zhonghua wei chang wai ke za zhi = Chinese journal of gastrointestinal surgery. 2017 Apr 25:20(4):388-392 [PubMed PMID: 28440518]
Laing P, Pham T, Taylor LJ, Fang J. Filling the Void: A Review of Intragastric Balloons for Obesity. Digestive diseases and sciences. 2017 Jun:62(6):1399-1408. doi: 10.1007/s10620-017-4566-2. Epub 2017 Apr 18 [PubMed PMID: 28421456]
Abu Dayyeh BK, Edmundowicz S, Thompson CC. Clinical Practice Update: Expert Review on Endoscopic Bariatric Therapies. Gastroenterology. 2017 Mar:152(4):716-729. doi: 10.1053/j.gastro.2017.01.035. Epub 2017 Jan 29 [PubMed PMID: 28147221]
Gagner M, Hutchinson C, Rosenthal R. Fifth International Consensus Conference: current status of sleeve gastrectomy. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2016 May:12(4):750-756. doi: 10.1016/j.soard.2016.01.022. Epub 2016 Jan 25 [PubMed PMID: 27178618]
Level 3 (low-level) evidenceZheng CZ, Zhuo GZ. [Understanding of International Sleeve Gastroectomy Expert Panel Consensus Statement and our experience]. Zhonghua wei chang wai ke za zhi = Chinese journal of gastrointestinal surgery. 2012 Nov:15(11):1099-101 [PubMed PMID: 23323292]
Level 3 (low-level) evidenceDimitrov DV, Ivanov V, Atanasova M. Advantages of bariatric medicine for individualized prevention and treatments: multidisciplinary approach in body culture and prevention of obesity and diabetes. The EPMA journal. 2011 Sep:2(3):271-6. doi: 10.1007/s13167-011-0099-5. Epub 2011 Jul 14 [PubMed PMID: 23199162]
Mancini MC. Bariatric surgery--an update for the endocrinologist. Arquivos brasileiros de endocrinologia e metabologia. 2014 Dec:58(9):875-88. doi: 10.1590/0004-2730000003413. Epub [PubMed PMID: 25627042]
Runkel N, Colombo-Benkmann M, Hüttl TP, Tigges H, Mann O, Flade-Kuthe R, Shang E, Susewind M, Wolff S, Wunder R, Wirth A, Winckler K, Weimann A, de Zwaan M, Sauerland S. Evidence-based German guidelines for surgery for obesity. International journal of colorectal disease. 2011 Apr:26(4):397-404. doi: 10.1007/s00384-011-1136-5. Epub 2011 Feb 12 [PubMed PMID: 21318299]
Scheiwiller A, Sykora M. [Obesity surgery--useful knowledge in indication and follow up]. Praxis. 2009 Oct 7:98(20):1155-60. doi: 10.1024/1661-8157.98.20.1155. Epub [PubMed PMID: 19809979]
Silva JN, Vasconcelos H, Figueiredo-Braga M, Carneiro S. How is Bariatric Surgery Improving the Quality of Life of Obese Patients: A Portuguese Cross-Sectional Study. Acta medica portuguesa. 2018 Aug 31:31(7-8):391-398. doi: 10.20344/amp.9133. Epub 2018 Aug 31 [PubMed PMID: 30189167]
Level 2 (mid-level) evidenceWilding J, Zourikian N, Di Minno M, Khair K, Marquardt N, Benson G, Ozelo M, Hermans C. Obesity in the global haemophilia population: prevalence, implications and expert opinions for weight management. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2018 Nov:19(11):1569-1584. doi: 10.1111/obr.12746. Epub 2018 Sep 6 [PubMed PMID: 30188610]
Level 3 (low-level) evidenceGrandone A, Di Sessa A, Umano GR, Toraldo R, Miraglia Del Giudice E. New treatment modalities for obesity. Best practice & research. Clinical endocrinology & metabolism. 2018 Aug:32(4):535-549. doi: 10.1016/j.beem.2018.06.007. Epub 2018 Jun 25 [PubMed PMID: 30086873]
Faria SL, Faria OP, de Gouvêa HR, Amato AA. Supplementation Adherence and Outcomes Among Pregnant Women After Bariatric Surgery. Obesity surgery. 2019 Jan:29(1):178-182. doi: 10.1007/s11695-018-3499-y. Epub [PubMed PMID: 30218196]
Yeo D, Yeo C, Low TY, Ahmed S, Phua S, Oo AM, Rao J, Koura A, Venkataraman K, Kaushal S. Outcomes After Metabolic Surgery in Asians-a Meta-analysis. Obesity surgery. 2019 Jan:29(1):114-126. doi: 10.1007/s11695-018-3484-5. Epub [PubMed PMID: 30196357]
Level 1 (high-level) evidencePanagiotou OA, Markozannes G, Adam GP, Kowalski R, Gazula A, Di M, Bond DS, Ryder BA, Trikalinos TA. Comparative Effectiveness and Safety of Bariatric Procedures in Medicare-Eligible Patients: A Systematic Review. JAMA surgery. 2018 Nov 1:153(11):e183326. doi: 10.1001/jamasurg.2018.3326. Epub 2018 Nov 21 [PubMed PMID: 30193303]
Level 2 (mid-level) evidence