Introduction
Sinusitis, or rhinosinusitis, is the symptomatic inflammation of the paranasal sinuses and nasal cavity mucosa. This inflammation may be caused by viruses, bacteria, fungi, and allergens, often occurring in combination or sequentially. The Rhinosinusitis Task Force established diagnostic criteria in 1997, categorizing symptoms into major and minor criteria.[1] The diagnosis of sinusitis requires the presence of either 2 major factors or 1 major and 2 minor factors. The diagnostic criteria are as follows:
Major
- Purulence on nasal examination
- Nasal obstruction/blockage
- Nasal discharge/purulence/discolored postnasal drainage
- Hyposmia/anosmia
- Fever
- Facial pain/pressure
- Facial congestion/fullness
Minor
- Ear pain/pressure/fullness
- Cough
- Dental pain
- Fatigue
- Halitosis
- Fever
- Headache
Rhinosinusitis can be classified according to the duration of symptoms. Acute rhinosinusitis lasts fewer than 4 weeks, while subacute sinusitis lasts between 4 and 12 weeks. Chronic sinusitis lasts more than 12 weeks. Recurrent acute rhinosinusitis (RARS) is defined as experiencing 4 or more episodes of acute rhinosinusitis per year, with each episode lasting at least 10 days and without persistent symptoms in between individual episodes.[2] This activity will focus primarily on RARS and detail patient presentation, diagnosis, and intervention.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
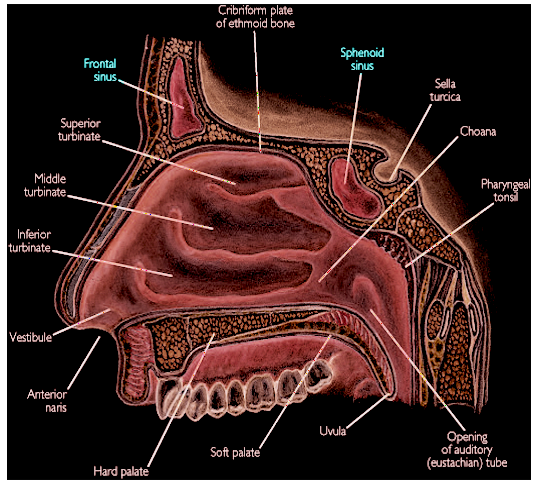
The most common etiologies for RARS mirror those of other sinusitis types. Viral upper respiratory tract infection is the most common cause of sinusitis and is typically self-limiting.[3] In these cases, viral inoculation triggers inflammation and irritation of the nasal cavity mucosa and paranasal sinuses (see Image. Anatomical Position of Sinuses). This inflammation reduces the size of the sinus ostia (outflow openings), obstructing the clearance of nasal flora, mucus, and inhaled particles from the sinuses. Inflammation also impairs ciliary movement and causes mucus stasis, predisposing the sinuses to bacterial infection. Similarly, untreated allergic rhinitis can cause chronic inflammation in the nose and paranasal sinuses, resulting in outflow tract obstruction, secretion buildup, and potential bacterial infection.
The most common bacterial pathogens causing RARS are Streptococcus pneumoniae, Haemophilus influenzae, other Streptococcus species, Moraxella catarrhalis, and Staphylococcus aureus.[4] Methicillin-resistant S aureus (MRSA) often colonizes the nares and leads to recurrent sinusitis, especially in patients who have undergone multiple courses of antibiotics.
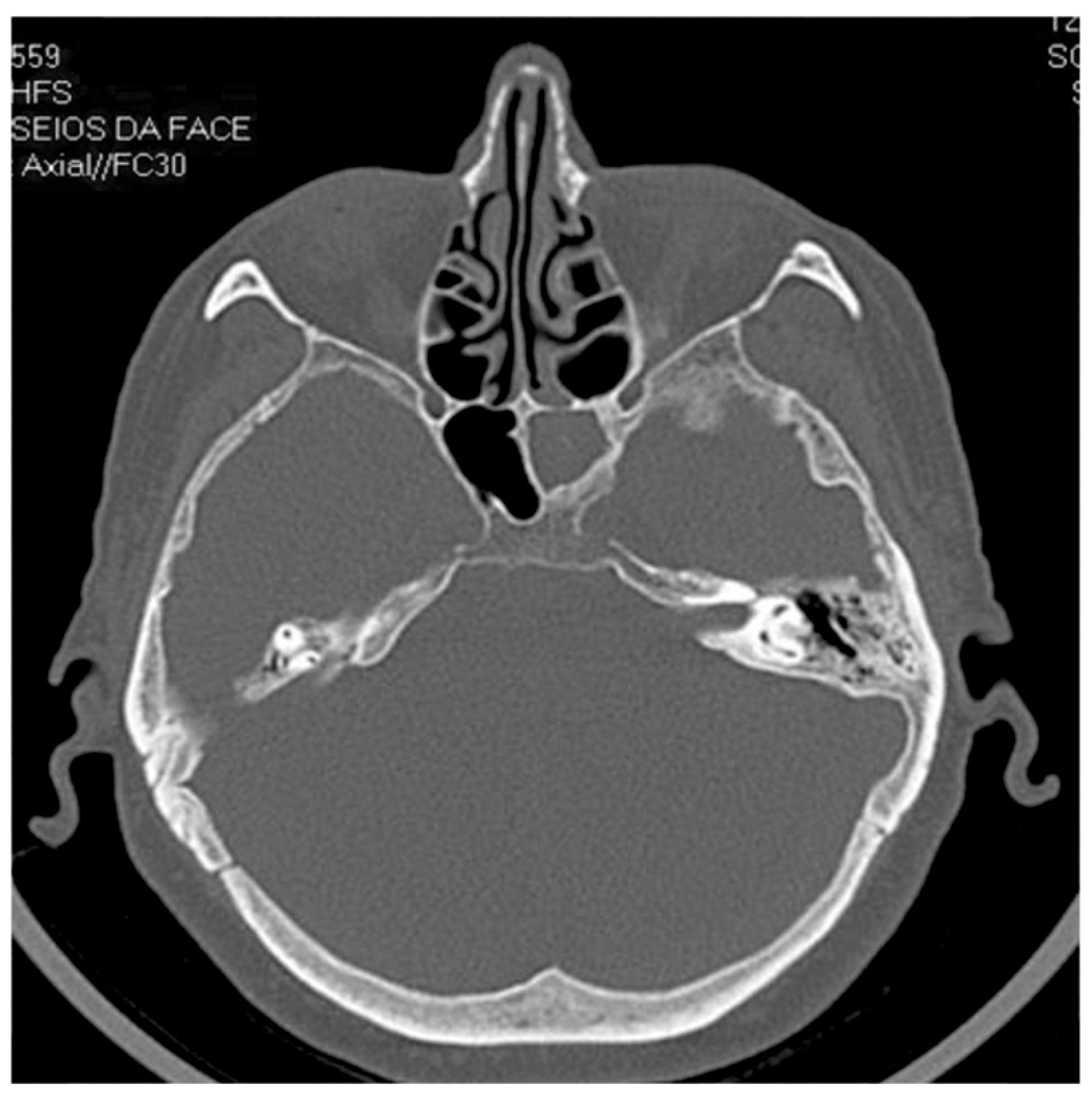
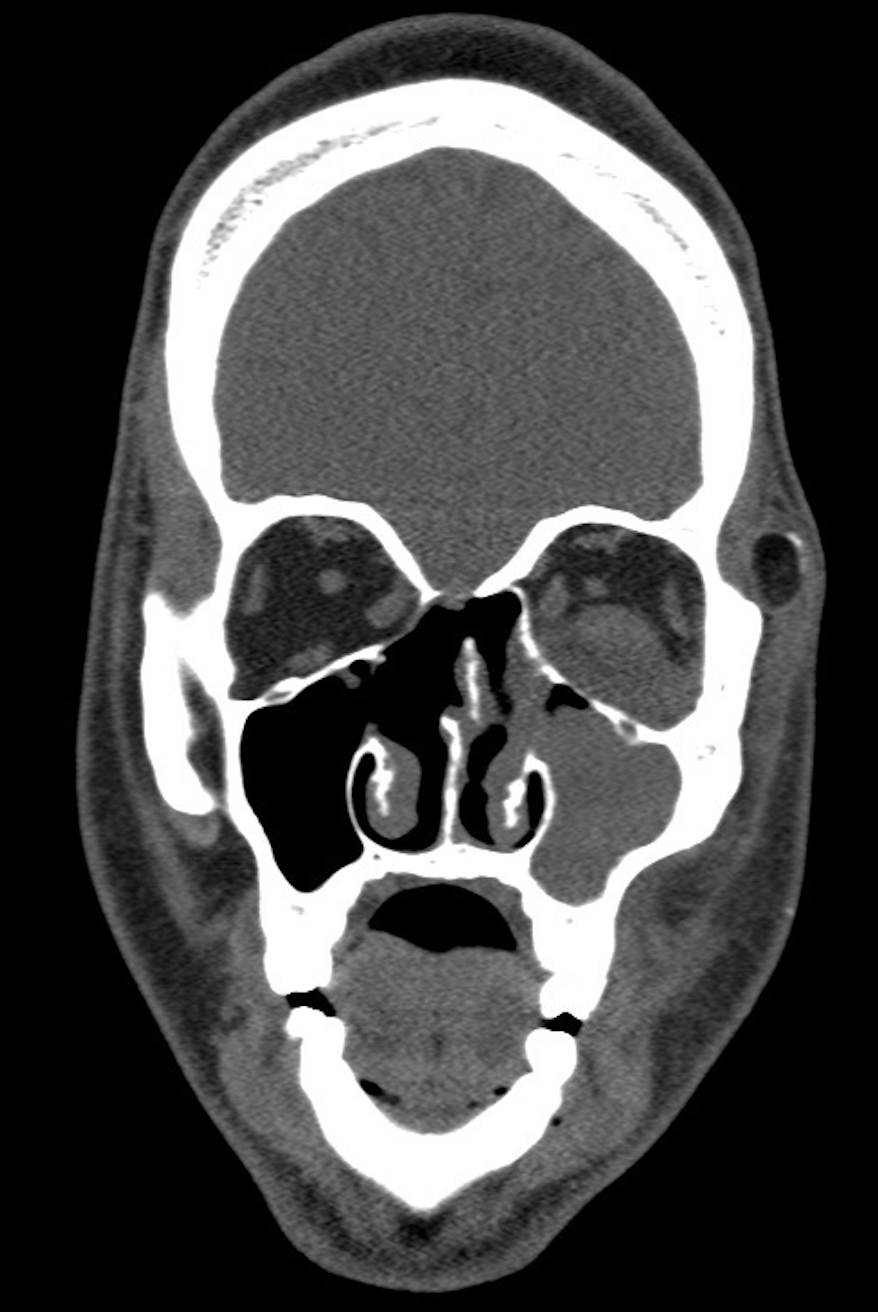
There is some etiologic overlap between RARS and chronic rhinosinusitis. Noninvasive fungal pathogens such as Aspergillus fumigatus may be isolated in these patients (see Image. Fungal Sinusitis and Image. Axial View Fungal Sinusitis). Anatomic obstructive abnormalities, including turbinate hypertrophy, conchae bullosae, stenosed sinus ostia, Haller cells (ethmoid cells within the medial orbital floor impinging the maxillary sinus drainage pathway), nasal polyposis, nasal masses, and septal spurs and deviation, can predispose the nasal cavity and sinuses to infection.[5][6] These structural abnormalities are often correctable through endoscopic surgical techniques.
Genetic factors affecting nasociliary motion or mucus production, like Kartagener syndrome, have also been suggested to play a role in sinus disease pathophysiology. Environmental factors, such as tobacco smoke and chronic exposure to inhaled irritants, have been implicated in the development or exacerbation of RARS. These factors impair ciliary motility and disrupt cell signaling in the innate immune system, exacerbating the condition.[7][8]
Epidemiology
Sinusitis ranks among the most common conditions prompting medical attention, with 1 in 8 adults receiving a sinusitis diagnosis at least once in their lifetime.[9] Sinusitis accounts for 20% of all antibiotic prescriptions.[10] In the United States alone, in 2015, there were 30 million diagnosed sinusitis cases, incurring a substantial treatment cost exceeding $11 billion: $3 billion allocated to acute sinusitis and $8.3 billion to chronic sinusitis.[4] A comprehensive review of a medical claims database encompassing 13.1 million people from 2003 to 2008 revealed a RARS prevalence of 1 in 3,000. Within this population, females constituted the majority (72.1%) of affected individuals, with a mean age of 43.5 years. On average, patients had 5.6 annual healthcare visits and filled 9.4 prescriptions per year, resulting in an annual direct cost burden of $1,091 per patient.[11]
Pathophysiology
The pathogenesis of rhinosinusitis likely involves a combination of viscous sinus secretions and dysfunction of the sinus ostia and ciliary apparatus. Viral upper respiratory infections and allergens cause mucosal edema, narrowing the sinus ostia and causing direct mechanical obstruction. Obstruction of the sinus may lead to the accumulation of secretions, providing an environment conducive to bacterial and fungal growth (see Image. Sinus Anatomy). Outflow blockage may also cause pressure changes within the sinus as oxygen is resorbed by the mucosa, resulting in a partial vacuum. This negative pressure can be painful and result in the transudation of more fluid into the sinus. The excess fluid, combined with inflammation and the influx of neutrophils and lymphocytes, can ultimately create excessive positive pressure, causing discomfort for patients.
In certain cases, typically chronic sinusitis, negative pressure can persist to the extent that it causes contraction of the maxillary sinus, a condition termed "silent sinus syndrome." This process may lead to the descent of the orbital floor and enophthalmos.[12]
In rhinosinusitis, altered sinus secretions exacerbate the susceptibility to persistent infection and subsequent inflammation. Normally, the mucous blanket in the respiratory tract consists of 2 distinct layers: the periciliary liquid phase, a thin, low-viscosity layer surrounding the cilia shaft allowing free ciliary movement, and the gel phase, a more viscous layer atop the periciliary liquid. In the presence of inflammation, derangements in the mucous layer separation can impair ciliary movement by disrupting the usual low-viscosity environment.[13]
Additionally, bacterial biofilms contribute to sinusitis pathogenesis, although they are more prevalent in chronic cases rather than in RARS.[14] Biofilms hinder antibiotic penetration because bacteria within this layer are not only attached firmly to one another as well as their substrate but they are also surrounded by a protective proteinaceous or polysaccharide matrix.[15] S aureus, notably, is adept at producing biofilms, which often require chemical and possibly mechanical disruption for definitive infection clearance.
History and Physical
Individuals experiencing acute sinusitis typically present with symptoms persisting for less than 4 weeks. Specific symptoms may include nasal or postnasal (nasopharyngeal) purulence, nasal obstruction, hyposmia, anosmia, fever, facial pain or pressure, maxillary dental pain, fatigue, halitosis, and headache, among other complaints[10]. Patients with RARS, by definition, will have encountered at least 4 of these episodes within the preceding year, often necessitating multiple treatment regimens involving nasal sprays, steroids, and antibiotics.
During a physical examination, observable signs may include purulent rhinorrhea or pharyngeal drainage, turbinate hypertrophy, mucosal edema, or erythema observed on anterior rhinoscopy. External tenderness upon palpation of the frontal, ethmoid, or maxillary sinuses might be present. Patients could display fever or tachycardia due to generalized facial pain. Although rare, acute sinusitis can lead to complications such as orbital cellulitis, preseptal cellulitis, or cavernous sinus thrombosis.[16] Cranial nerve evaluation and close orbit inspection should be performed to rule out these complications.
Patients with RARS often experience symptoms similar to those of acute sinusitis. A viral origin is presumed if the patient reports symptoms lasting fewer than 10 days during an acute sinusitis episode.[1] The diagnosis of acute bacterial rhinosinusitis should be considered if symptoms last more than 7 days or worsen within 2 days after initial improvement, also known as "double worsening" or "second sickening."[10][17] Most episodes of acute sinusitis, whether viral or bacterial in etiology, resolve within 10 to 14 days.
Evaluation
History and physical examination are crucial to diagnosing RARS. In most cases, healthcare providers can accurately diagnose RARS by evaluating the duration and progression of symptoms, along with applying the major and minor diagnostic criteria set outlined by the American Academy of Otolaryngology-Head and Neck Surgery.[18] Patients exhibiting unilateral disease without septal deviation, experiencing severe and debilitating symptoms, or those whose symptoms persist despite appropriate empirical treatment should undergo nasal endoscopy for further evaluation.[1]
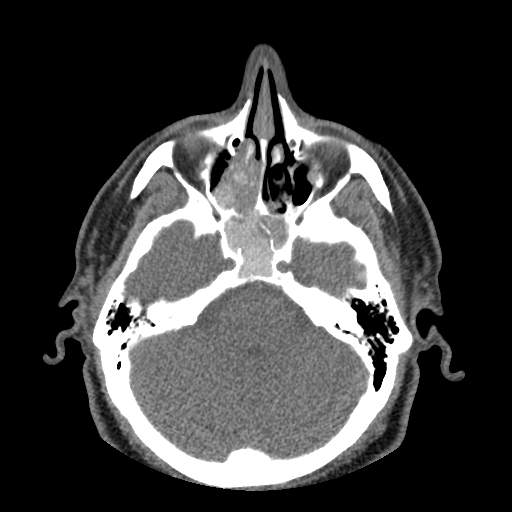
Radiological imaging is not routinely recommended to evaluate patients with presumed uncomplicated RARS. However, a noncontrast computed tomography scan of the sinuses is indicated for patients with chronic rhinosinusitis, suspected anatomical abnormalities, or possible orbital complications (see Image. Axial CT of Sphenoid Sinus). Additionally, CT scans are integral to presurgical planning for procedures like balloon sinuplasty and functional endoscopic sinus surgery (FESS).[19] Research suggests that imaging is overutilized for patients with sinusitis. According to a 2012 study published by Bhattacharyya et al, 11.4% of patients with uncomplicated RARS received a CT scan within 1 year of diagnosis; the number increased to 39.9% at 4 years.[11]
In cases of persistent or chronic sinusitis, cultures obtained from sinus aspirates or endoscopy might be necessary to identify resistant bacterial or fungal pathogens. The most common pathogens involved in RARS overlap those causing acute sinusitis, including S pneumoniae, H influenzae, other Streptococcus species, M catarrhalis, and S aureus.[4]
Treatment / Management
Medical management stands as the primary approach for treating RARS. Many patients require a combination of therapies addressing different components of the complex pathophysiology underlying RARS. These treatments are outlined below.
- Topical intranasal therapy
- Nasal saline irrigation effectively removes or reduces debris and pathogens from the nares, offering potential symptomatic relief. The efficacy of hypertonic versus isotonic saline solutions is debated, with hypertonic saline causing more adverse effects like increased nasal discharge and local discomfort. Excessive irrigation may disrupt natural protective mechanisms within the nose and paranasal sinuses by disrupting the mucus layer, reducing effectiveness.[20][21]
- Topical corticosteroid nasal sprays reduce mucosal inflammation, decreasing stenosis of sinus drainage pathways. These sprays are beneficial as preventive measures and also during acute infections.
- Topical antihistamines, such as azelastine, can help alleviate mucosal inflammation and irritation, reduce nasal passage edema, and open the sinus ostia.
- Topical decongestant sprays such as oxymetazoline and phenylephrine can reduce congestion via local vasoconstriction. Patients should be cautioned about rebound congestion, a potential side effect of prolonged use. The use of these medications should be limited to 3 to 5 consecutive days.[22]
- Antibiotics
- Bacterial sinusitis complicates only 0.5% to 2% of cases of viral sinusitis.[21] Therefore, antibiotic therapy should be started only if the symptoms persist for more than 7 days without improvement or if symptoms worsen after an initial improvement period.
- For RARS, the recommended initial antibiotic therapy is amoxicillin with or without clavulanate for 5 to 10 days. A 2021 study published by Rovelsky et al indicates that amoxicillin is as effective as amoxicillin-clavulanate in treating acute sinusitis but causes fewer adverse gastrointestinal symptoms.[23] Alternatives for penicillin-allergic patients or resistant infections include doxycycline and respiratory fluoroquinolones (levofloxacin, moxifloxacin). Other options include third-generation cephalosporins with or without clindamycin, depending on the clinical situation.[4]
- Intravenous antibiotics are the mainstay of treatment for patients with orbital cellulitis or moderate-to-severe preseptal cellulitis. Recommended antibiotics include vancomycin and ampicillin-sulbactam, clindamycin, third-generation cephalosporins, or piperacillin-tazobactam.[24]
- Decongestants
- Oral decongestants provide symptomatic relief by reducing inflammation and secretions in the nasal, sinus, and respiratory tract mucosa. They may also help maintain patency of the nasal ostia, leading to a reduction of sinus pressure.
- Oral antihistamines
- Oral antihistamines disrupt the biological histamine pathway, preventing mucosal edema and inflammation triggered by inhaled allergens in sensitized patients. They can benefit patients whose sinusitis is suspected to be precipitated or exacerbated by allergic rhinitis.[25]
- Oral steroids
- Oral steroids are not recommended as a monotherapy for acute rhinosinusitis. Limited evidence supports the use of oral steroids as an adjunct treatment alongside antimicrobial therapy for acute sinusitis.[26]
- Oral leukotriene modifiers
- Leukotriene modifiers, such as montelukast, are effective treatments for allergic rhinitis and nasal polyposis. They can be particularly beneficial for patients with rhinosinusitis who have asthma, allergic rhinitis, or nasal polyposis.[27]
Surgical intervention for recurrent acute rhinosinusitis can be considered for patients who do not respond to medical management, particularly if they have documented anatomic abnormalities that correlate with their symptoms. Surgery has been shown to decrease symptoms and improve the quality of life for appropriately selected patients.[9][28][29] Surgical intervention is also often required for patients with sinusitis-related complications such as subperiosteal abscess, orbital abscess, or cavernous sinus thrombosis. Specific surgical approaches are detailed below.(A1)
Functional endoscopic sinus surgery can correct anatomic abnormalities that prevent optimal sinus drainage. Various procedures, including maxillary antrostomy, uncinate process resection, ethmoidectomy, and Draf I-III frontal sinusotomies can be performed depending on the location and severity of the individual patient’s pathology. Before surgical intervention, a noncontrast CT of the sinuses should be performed to confirm the diagnosis and localize the pathology for surgical planning.[19] Preoperative CT imaging can also aid intraoperative navigation, improving outcomes and reducing complication rates, particularly in revision cases.[30][31](B2)
Balloon sinuplasty is a tissue-sparing procedure designed to permanently dilate the sinus ostia and drainage pathways through localized microfracturing via balloon insufflation. This procedure enhances mucus drainage and reduces negative pressure within the sinus cavities. Balloon sinuplasty treats patients with RARS and chronic rhinosinusitis without nasal polyposis (CRSsNP).[28] This minimally invasive procedure may be performed in an operating room or office setting. (A1)
Septoplasty is a surgical option for patients with obstructive nasal septal deviations. The procedure reduces impingement of the sinus ostia, improves airflow, and facilitates proper mucociliary clearance.
Turbinate reduction may alleviate nasal obstruction and allow further anterior drainage of nasal and sinus contents in patients with hypertrophy of the inferior turbinates.
Differential Diagnosis
Several disease processes share overlapping symptoms with RARS, necessitating careful consideration of differential diagnoses. Before confirming the diagnosis, other diseases and conditions that should be ruled out include:
- Allergic rhinosinusitis
- Acute rhinosinusitis
- Chronic rhinosinusitis with nasal polyposis (CRSwNP)
- Chronic rhinosinusitis without nasal polyposis (CRSsNP)
- Subacute rhinosinusitis
- Viral rhinosinusitis (upper respiratory tract infection)
- Noninvasive fungal rhinosinusitis
- Invasive fungal rhinosinusitis
- Adenoiditis
- Cerebrospinal fluid (CSF) rhinorrhea
- Vasomotor rhinitis
- Laryngopharyngeal/gastroesophageal reflux disease
Prognosis
The prognosis for recurrent acute rhinosinusitis is generally good. Most patients respond well to medical management, including topical nasal sprays and oral antibiotics. Patients rarely develop complications requiring hospitalization for immediate surgical intervention or intravenous antibiotics. Appropriately selected patients who undergo surgery typically experience symptomatic relief and appreciable improvement in quality of life.[28][29][32]
Complications
Although rare, complications of recurrent acute rhinosinusitis include but are not limited to the following:
- Persistent hyposmia/anosmia
- Preseptal cellulitis
- Orbital cellulitis
- Subperiosteal abscess
- Orbital abscess
- Cavernous sinus thrombosis
Consultations
Consultation with an ophthalmologist may be necessary for additional evaluation and management of orbital complications. Patients who require revision endoscopic sinus surgery may be better served by a subspecialist, such as a rhinologist, rather than a general otolaryngologist-head and neck surgeon.
Deterrence and Patient Education
Educating patients about the expected progression of symptoms, home management strategies, and circumstances warranting medical attention is crucial. This anticipatory guidance empowers patients to recognize and treat their symptoms earlier in the course of illness. Effective early symptom management can decrease symptom escalation, reducing the necessity for more aggressive and costly therapies. In cases where additional treatment is necessary, providing education about medication regimens, common adverse effects, and expected outcomes can increase patient satisfaction and understanding.
Pearls and Other Issues
Key points to remember regarding the diagnosis and treatment of RARS include:
- Recurrent sinusitis is a clinical diagnosis defined by 4 or more distinct episodes of sinusitis per year, with symptom-free intervals between episodes.
- Routine diagnostic imaging is not recommended for uncomplicated RARS; however, a noncontrast CT scan may demonstrate anatomical obstructions and provide valuable information for surgical planning.
- Symptomatic treatment with a trial of a decongestant nasal spray, daily intranasal irrigation, and a corticosteroid nasal spray is the mainstay of treatment during the first 7 days of symptoms.
- A variety of antibiotics may be used to treat suspected bacterial sinusitis. The specific choice of medication should be based on local antibiograms, patient risk factors, allergies, and comorbidities. Drug resistance should be considered in refractory cases, and cultures should be obtained to inform targeted therapy.
- While medical therapy is the mainstay of treatment for most patients, research indicates that surgical intervention benefits a subset of patients with RARS. Outcomes are similar to those seen in patients surgically treated for chronic rhinosinusitis.
- Endoscopic surgical techniques benefit patients with proven turbinate hypertrophy, conchae bullosa, stenosed sinus ostia, frontal sinus cells, Haller cells, and septal spurs.
- Balloon sinus dilation is a minimally invasive endoscopic approach that effectively treats RARS and CRSsNP.
- Orbital complications of RARS, such as preseptal cellulitis, orbital cellulitis, and cavernous sinus thrombosis, necessitate vigilant monitoring for the development of cranial nerve deficits or other signs of orbital involvement, ensuring immediate treatment when indicated.
Enhancing Healthcare Team Outcomes
RARS can pose significant challenges for patients and clinicians due to its recurring nature. Establishing a medical home, where primary care providers can monitor patients over time and coordinate their care, proves beneficial. Collaborating with interprofessional team members, including general otolaryngologists, rhinologists, pharmacists, nurses, and, in some cases, ophthalmologists, is essential. Tailoring management to each patient’s needs is crucial, as responses to specific treatments vary.
Primary and specialty care providers are pivotal in diagnosing and formulating evidence-based treatment plans. Pharmacists are instrumental in ensuring appropriate medication selection and dosing, considering patient allergies and comorbidities. Nurses provide direct patient care, offer education, and often facilitate communication between patients and physicians. Otolaryngologists, rhinologists, and ophthalmologists are usually required to manage complications or perform surgical procedures when medical management fails. Effective collaboration among these professionals is critical for comprehensive and successful management.
Media
(Click Image to Enlarge)
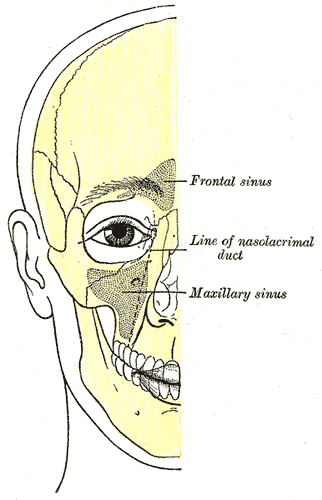
Anatomical Positioning of Sinuses. Illustrated image depicting the facial bone outline, highlighting the positions of air sinuses, including the frontal sinus, line of the nasolacrimal duct, and the maxillary sinus.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Brook I, Ashok Kumar K, Kramper M, Orlandi RR, Palmer JN, Patel ZM, Peters A, Walsh SA, Corrigan MD. Clinical practice guideline (update): adult sinusitis. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2015 Apr:152(2 Suppl):S1-S39. doi: 10.1177/0194599815572097. Epub [PubMed PMID: 25832968]
Level 1 (high-level) evidenceMeltzer EO, Hamilos DL, Hadley JA, Lanza DC, Marple BF, Nicklas RA, Bachert C, Baraniuk J, Baroody FM, Benninger MS, Brook I, Chowdhury BA, Druce HM, Durham S, Ferguson B, Gwaltney JM, Kaliner M, Kennedy DW, Lund V, Naclerio R, Pawankar R, Piccirillo JF, Rohane P, Simon R, Slavin RG, Togias A, Wald ER, Zinreich SJ, American Academy of Allergy, Asthma and Immunology (AAAAI), American Academy of Otolaryngic Allergy (AAOA), American Academy of Otolaryngology--Head and Neck Surgery (AAO-HNS), American College of Allergy, Asthma and Immunology (ACAAI), American Rhinologic Society (ARS). Rhinosinusitis: establishing definitions for clinical research and patient care. The Journal of allergy and clinical immunology. 2004 Dec:114(6 Suppl):155-212 [PubMed PMID: 15577865]
Meltzer EO, Hamilos DL, Hadley JA, Lanza DC, Marple BF, Nicklas RA, Bachert C, Baraniuk J, Baroody FM, Benninger MS, Brook I, Chowdhury BA, Druce HM, Durham S, Ferguson B, Gwaltney JM Jr, Kaliner M, Kennedy DW, Lund V, Naclerio R, Pawankar R, Piccirillo JF, Rohane P, Simon R, Slavin RG, Togias A, Wald ER, Zinreich SJ, American Academy of Allergy, Asthma and Immunology, American Academy of Otolaryngic Allergy, American Academy of Otolaryngology-Head and Neck Surgery, American College of Allergy, Asthma and Immunology, American Rhinologic Society. Rhinosinusitis: Establishing definitions for clinical research and patient care. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2004 Dec:131(6 Suppl):S1-62 [PubMed PMID: 15577816]
Anon JB, Jacobs MR, Poole MD, Ambrose PG, Benninger MS, Hadley JA, Craig WA, Sinus And Allergy Health Partnership. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2004 Jan:130(1 Suppl):1-45 [PubMed PMID: 14726904]
Level 1 (high-level) evidencePapadopoulou AM, Chrysikos D, Samolis A, Tsakotos G, Troupis T. Anatomical Variations of the Nasal Cavities and Paranasal Sinuses: A Systematic Review. Cureus. 2021 Jan 15:13(1):e12727. doi: 10.7759/cureus.12727. Epub 2021 Jan 15 [PubMed PMID: 33614330]
Level 1 (high-level) evidenceJorissen M, Hermans R, Bertrand B, Eloy P. Anatomical variations and sinusitis. Acta oto-rhino-laryngologica Belgica. 1997:51(4):219-26 [PubMed PMID: 9444370]
Benninger MS. The impact of cigarette smoking and environmental tobacco smoke on nasal and sinus disease: a review of the literature. American journal of rhinology. 1999 Nov-Dec:13(6):435-8 [PubMed PMID: 10631398]
Frieri M, Kumar K, Boutin A. Review: Immunology of sinusitis, trauma, asthma, and sepsis. Allergy & rhinology (Providence, R.I.). 2015 Jan:6(3):205-14. doi: 10.2500/ar.2015.6.0140. Epub [PubMed PMID: 26686215]
Saltagi MZ, Comer BT, Hughes S, Ting JY, Higgins TS. Management of Recurrent Acute Rhinosinusitis: A Systematic Review. American journal of rhinology & allergy. 2021 Nov:35(6):902-909. doi: 10.1177/1945892421994999. Epub 2021 Feb 23 [PubMed PMID: 33622038]
Level 1 (high-level) evidenceAring AM, Chan MM. Current Concepts in Adult Acute Rhinosinusitis. American family physician. 2016 Jul 15:94(2):97-105 [PubMed PMID: 27419326]
Bhattacharyya N, Grebner J, Martinson NG. Recurrent acute rhinosinusitis: epidemiology and health care cost burden. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2012 Feb:146(2):307-12. doi: 10.1177/0194599811426089. Epub 2011 Oct 25 [PubMed PMID: 22027867]
Level 2 (mid-level) evidenceSheikhi M,Jalalian F, The silent sinus syndrome. Dental research journal. 2013 Mar; [PubMed PMID: 23946747]
Level 3 (low-level) evidenceBeule AG. Physiology and pathophysiology of respiratory mucosa of the nose and the paranasal sinuses. GMS current topics in otorhinolaryngology, head and neck surgery. 2010:9():Doc07. doi: 10.3205/cto000071. Epub 2011 Apr 27 [PubMed PMID: 22073111]
Karunasagar A, Garag SS, Appannavar SB, Kulkarni RD, Naik AS. Bacterial Biofilms in Chronic Rhinosinusitis and Their Implications for Clinical Management. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2018 Mar:70(1):43-48. doi: 10.1007/s12070-017-1208-0. Epub 2017 Sep 25 [PubMed PMID: 29456942]
Vestby LK, Grønseth T, Simm R, Nesse LL. Bacterial Biofilm and its Role in the Pathogenesis of Disease. Antibiotics (Basel, Switzerland). 2020 Feb 3:9(2):. doi: 10.3390/antibiotics9020059. Epub 2020 Feb 3 [PubMed PMID: 32028684]
Chang YS, Chen PL, Hung JH, Chen HY, Lai CC, Ou CY, Chang CM, Wang CK, Cheng HC, Tseng SH. Orbital complications of paranasal sinusitis in Taiwan, 1988 through 2015: Acute ophthalmological manifestations, diagnosis, and management. PloS one. 2017:12(10):e0184477. doi: 10.1371/journal.pone.0184477. Epub 2017 Oct 3 [PubMed PMID: 28972988]
Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Brook I, Kumar KA, Kramper M, Orlandi RR, Palmer JN, Patel ZM, Peters A, Walsh SA, Corrigan MD. Clinical practice guideline (update): Adult Sinusitis Executive Summary. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2015 Apr:152(4):598-609. doi: 10.1177/0194599815574247. Epub [PubMed PMID: 25833927]
Level 1 (high-level) evidenceMeltzer EO, Hamilos DL. Rhinosinusitis diagnosis and management for the clinician: a synopsis of recent consensus guidelines. Mayo Clinic proceedings. 2011 May:86(5):427-43. doi: 10.4065/mcp.2010.0392. Epub 2011 Apr 13 [PubMed PMID: 21490181]
Level 3 (low-level) evidenceCashman EC, Macmahon PJ, Smyth D. Computed tomography scans of paranasal sinuses before functional endoscopic sinus surgery. World journal of radiology. 2011 Aug 28:3(8):199-204. doi: 10.4329/wjr.v3.i8.199. Epub [PubMed PMID: 22022638]
Kanjanawasee D, Seresirikachorn K, Chitsuthipakorn W, Snidvongs K. Hypertonic Saline Versus Isotonic Saline Nasal Irrigation: Systematic Review and Meta-analysis. American journal of rhinology & allergy. 2018 Jul:32(4):269-279. doi: 10.1177/1945892418773566. Epub 2018 May 18 [PubMed PMID: 29774747]
Level 1 (high-level) evidencePark DY, Choi JH, Kim DK, Jung YG, Mun SJ, Min HJ, Park SK, Shin JM, Yang HC, Hong SN, Mo JH. Clinical Practice Guideline: Nasal Irrigation for Chronic Rhinosinusitis in Adults. Clinical and experimental otorhinolaryngology. 2022 Feb:15(1):5-23. doi: 10.21053/ceo.2021.00654. Epub 2022 Feb 15 [PubMed PMID: 35158420]
Level 1 (high-level) evidenceMortuaire G, de Gabory L, François M, Massé G, Bloch F, Brion N, Jankowski R, Serrano E. Rebound congestion and rhinitis medicamentosa: nasal decongestants in clinical practice. Critical review of the literature by a medical panel. European annals of otorhinolaryngology, head and neck diseases. 2013 Jun:130(3):137-44. doi: 10.1016/j.anorl.2012.09.005. Epub 2013 Feb 1 [PubMed PMID: 23375990]
Level 3 (low-level) evidenceRovelsky SA, Remington RE, Nevers M, Pontefract B, Hersh AL, Samore M, Madaras-Kelly K. Comparative effectiveness of amoxicillin versus amoxicillin-clavulanate among adults with acute sinusitis in emergency department and urgent care settings. Journal of the American College of Emergency Physicians open. 2021 Jun:2(3):e12465. doi: 10.1002/emp2.12465. Epub 2021 Jun 16 [PubMed PMID: 34179886]
Level 2 (mid-level) evidenceLee S, Yen MT. Management of preseptal and orbital cellulitis. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2011 Jan:25(1):21-9. doi: 10.1016/j.sjopt.2010.10.004. Epub 2010 Dec 10 [PubMed PMID: 23960899]
Seresirikachorn K, Khattiyawittayakun L, Chitsuthipakorn W, Snidvongs K. Antihistamines for treating rhinosinusitis: systematic review and meta-analysis of randomised controlled studies. The Journal of laryngology and otology. 2018 Feb:132(2):105-110. doi: 10.1017/S002221511700192X. Epub 2017 Sep 13 [PubMed PMID: 28901282]
Level 1 (high-level) evidenceVenekamp RP, Thompson MJ, Hayward G, Heneghan CJ, Del Mar CB, Perera R, Glasziou PP, Rovers MM. Systemic corticosteroids for acute sinusitis. The Cochrane database of systematic reviews. 2014 Mar 25:(3):CD008115. doi: 10.1002/14651858.CD008115.pub3. Epub 2014 Mar 25 [PubMed PMID: 24664368]
Level 1 (high-level) evidenceParnes SM. The role of leukotriene inhibitors in patients with paranasal sinus disease. Current opinion in otolaryngology & head and neck surgery. 2003 Jun:11(3):184-91 [PubMed PMID: 12923360]
Level 3 (low-level) evidenceSikand A, Ehmer DR Jr, Stolovitzky JP, McDuffie CM, Mehendale N, Albritton FD 4th. In-office balloon sinus dilation versus medical therapy for recurrent acute rhinosinusitis: a randomized, placebo-controlled study. International forum of allergy & rhinology. 2019 Feb:9(2):140-148. doi: 10.1002/alr.22248. Epub 2018 Nov 19 [PubMed PMID: 30452127]
Level 1 (high-level) evidenceCosta ML, Psaltis AJ, Nayak JV, Hwang PH. Medical therapy vs surgery for recurrent acute rhinosinusitis. International forum of allergy & rhinology. 2015 Aug:5(8):667-73. doi: 10.1002/alr.21533. Epub 2015 May 7 [PubMed PMID: 25950995]
Galletti B, Gazia F, Freni F, Sireci F, Galletti F. Endoscopic sinus surgery with and without computer assisted navigation: A retrospective study. Auris, nasus, larynx. 2019 Aug:46(4):520-525. doi: 10.1016/j.anl.2018.11.004. Epub 2018 Dec 6 [PubMed PMID: 30528105]
Level 2 (mid-level) evidenceKacker A, Tabaee A, Anand V. Computer-assisted surgical navigation in revision endoscopic sinus surgery. Otolaryngologic clinics of North America. 2005 Jun:38(3):473-82, vi [PubMed PMID: 15907896]
Becker DG. Sinusitis. Journal of long-term effects of medical implants. 2003:13(3):175-94 [PubMed PMID: 14516184]