Introduction
Bedpan use in today's society is not that different from use in the 18th century. Bedpans are a way of addressing elimination concerns when the traditional toilet is not an option due to high risk of injury or debilitating illness in sick, bed-confined individuals.[1][2][3]
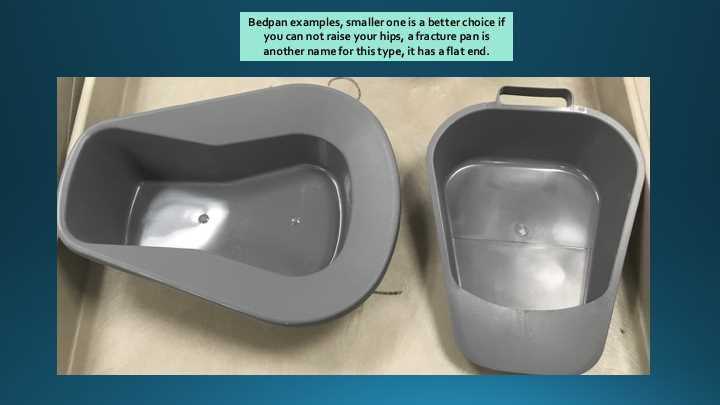
There are 2 types of bedpans: regular or fracture. The regular bedpan is larger than its fracture counterpart. The fracture pan has one flat end for ease of use with specific patient populations: i.e., hip fractures, hip replacements, or lower extremity fractures. Bariatric bedpans are available up to a 1200-pound (544-kg) capacity.[4]
Using the toilet may be a source of discomfort and embarrassment among all genders. Semi-private rooms or shared wards and hospital overcrowding are a challenge regarding patient privacy.[5][6]
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
Medical necessity may warrant the use of a bedpan, for example as with immobile patients with the following concerns:
- Fractures: hip, lower extremity
- Debilitating illness or profound fatigue
- Surgical considerations
- High fall risk and increased injury potential
- Obstetrical and gynecological
Equipment
Bedpans come in regular size or a smaller, fracture pan. Bedpans are chosen based on diagnosis, patient comfort or preference and if any contraindications exist for using the regular size such as a fracture. Gather all supplies before you start the procedure.[7][8]
Supplies
- Bedpan: Fracture or regular with bariatric considerations
- Personal protective equipment such as gloves
- Hand hygiene products, soap, a basin of water
- Incontinence pads, diapers
- Linens such as washcloths, sheets, privacy blankets
- Disposable wipes
- Privacy curtain
- Powder if advised per policy and no contraindication for use exist
- Toilet paper
- Trashcan
- Soiled linen hamper and location of the dirty/soiled utility room
- Graduated cylinder to measure output if a requirement
- Stool containers if cultures or other fecal tests are necessary
Technique or Treatment
Placing a patient on a bedpan requires a special technique and is reserved for those that are on bed rest per a health care provider order or discretion. Follow any preset institutional policies on the use of a bedpan in a clinical setting.
A patient that can assist with care by raising their hips is approached differently than a patient that cannot lift their hips due to surgical considerations, fractures, or other contraindications. In both cases, ensure the patient is pulled up as high as they can be on the stretcher or bed. If they can assist with raising their hips, then raise the head of the bed at least thirty degrees. Positioning in this Semi-Fowler's position allows for anatomical support and facilitates ease of defecation or urination by assuming a natural position for these bodily functions. According to a 2003 study, body positioning has a significant influence on intestinal gas propulsion and transit times with gastric flow being faster in the upright position than when supine [Dainese, Serra, Azpiroz & Malagelada, 2003].
Steps
- Lower the head of the bed to place the patient on the bedpan and when removing the pan, especially if in a patient that can not assist in raising their hips.
- Address the patient by their given name and introduce yourself, provide your name and title. Ensure identification of your patient with two unique identifiers.
- Explain what is about to happen and determine if the patient has any requests to facilitate task related to past experiences.
- Perform hand hygiene.
- Ensure patient privacy by pulling curtains. If in a semi-private room, consider asking any visiting family to leave the room. Bedpan use is often a source of embarrassment and discomfort for the patient; maintain patient dignity at all times [Logan, 2012].
- Put gloves on and follow any isolation precautions in place that requires gowns or other personal protective equipment (PPE).
- Raise the bed to a comfortable height which ensures proper ergonomic principles are followed to prevent a back injury [OSHA, 2009].
- An incontinence pad should be placed under the patient to act as a protective barrier from soiling the linens.
- The pad gets placed on the bottom sheet, under perineal area including buttocks and upper thighs.
- Place the bedpan under the patient by assisting the patient to roll on their side with their buttocks toward the healthcare provider.
- Powder or tissue paper may be used to prevent the patients' skin from adhering to the pan. Do not use powder if any contraindications for use i.e., wounds, allergies, sensitivities. Follow any policy and procedure for the use of powder.
- The bedpan will be placed under the patient according to the contour or shape of the device. The wide area of the bedpan points towards the patients head and narrow area towards feet.
- Make sure the buttocks are firm against the bedpan, pushed in a downward motion into the stretcher or mattress pad.
- Hold the bedpan with one hand and the hip with the other and roll the patient onto the bedpan.
- Avoid patient injury by never forcibly placing the pan under the buttocks. If a bariatric bedpan is needed, multiple staff members should assist to prevent injury to staff and patients.
- Make sure the bedpan is adequately positioned, so the patient avoids missing the bedpan and soiling the linens. A privacy blanket or sheet may be used to protect the top sheet.
- Raise the head of the stretcher or bed to a semi-fowler position, minimum of thirty degrees. Position a pillow to add comfort to the lower lumbar area and as a base of support. Raising the head of the bed while the patient is using it will facilitate voiding or defecating.
- Gatch the bed or ask the patient to bend their knees if no contraindications exist to facilitate a squatting motion.
- Ask the patient to call when ready to come off by using the call light provided.
- Place toilet paper near the patient for ease of use.
- Lower head of the bed to facilitate removal of the bedpan.
- Ensure perineal area is cleaned from front to back.
- Dry the skin properly after removal. Remove incontinence pad.
- Empty bedpan contents into the toilet, hopper or graduated cylinder if measuring is required.
- Clean bedpan and graduated cylinder after use, and place in an appropriate storage area as per procedural guidelines
- The patient should be offered a damp washcloth or wipes to cleanse their hands. Hand hygiene is essential for the patient and the healthcare provider to reduce infection potential, incorporating the "5 Moments for Hand Hygiene" [WHO, 2009].
- Place any linens used in soiled linen hamper/storage area and remove trash.
- Enquire as to any requests or preferences by the patient or family that should be addressed at this time or in the future. Address comfort level during the procedure.
- Make sure the patient is never placed too close to the edge of bed due to fall potential.
- Place the bed in a low, locked position, and put the call light within reach.
- Advise them to ask for assistance.
- Ensure proper lighting and set bed alarms if required. Open any curtains that were closed as per patient wishes and condition.
- Document accurate intake and output on flowsheet/chart/electronic medical record as per job description and scope of practice.
- Document any skin issues or other concerns as per job description, hospital policy and scope of practice. Note color, consistency and if any foul odor is present.
Complications
Complications surrounding bedpan use may include constipation, embarrassment, discomfort, and loss of dignity due to inadequate patient privacy.
Privacy and Dignity
An audit conducted in 2010 addressed "Toilet Privacy in the Hospital" [Logan, 2012]. Comments from patients and staff highlighted certain critical areas of concern in regards to toileting, privacy, and confidentiality.
Areas of interest amongst patients while toileting consisted of specific vital points, for example, call light out of reach or cord too short, slow response to call light, lack of hand hygiene after toilet use for the patient, curtains that would not close properly and lack of privacy while toileting. Suggestions were made to improve patient privacy while defecating or urinating such as better signage [Logan, 2012].
Constipation
Another complication of bedpan use can be constipation. An environment that lacks appropriate privacy may force a patient to feel that it is inconvenient to use the toilet, thus resisting the urge to defecate. If defecation is discommoding, the desire to defecate prompts voluntary contraction of the external sphincter and puborectalis muscle. This urge dissipates, and the rectum accommodates to hold more stool (as cited in Sun, Read & Miner, 1990)[Rao et al., 2016].
A study conducted between 2003 and 2004 on stroke patients found that (55.2%) developed new-onset constipation within a month after the first stroke [Su et al.,2009]. The study went on to conclude that patients with moderate severity of stroke (NIHSS 4 -11) on arrival had a higher incidence of bedpan use, thus poor outcomes at 3 months post-stroke as a result of the added complication of constipation. The study recommended a suitable environment for defecation for stroke patients to curb new-onset constipation and improve patient outcomes [Su et al., 2009].
A study sponsored by the Italian Space Agency analyzed ten healthy men for the effects extended bedrest had on the body as it related to new onset constipation. The men were studied for 35 days in a controlled environment on strict bedrest with bedpan use for defecation in a lying, head down position. At the end of the study, 60% had new onset functional constipation [Iovino et al., 2013].
Clinical Significance
Patients in need of toileting with the use of a bedpan can impose specific inherent risks, thus should be used with the knowledge of the emotional and physical implications in a clinical setting. This task should not be used for provider convenience, but with certain criteria for client selection to meet the standard of care. Staffing challenges may lead to delays in answering call lights and providing toileting assistance. These delays of care may place a patient at risk for falls and incontinence, thus contributing to emotional and physical duress. Missed care opportunities lead to a decrease in patient satisfaction and overall perception of care. Therefore reimbursement of care may be affected by a trickle-down effect with negative patient satisfaction scores.[9][10]
Enhancing Healthcare Team Outcomes
The bedpan is a useful medical equipment that is used frequently in hospitals. The nurses are primarily involved in the management of the bedpan with assistance from the therapists. The important features of bedpan are not only to provide a functional use for the patient, but comfort and privacy. If a bed pan is to be used, it should be for a short duration. there are countless cases of pressure sores, ulcers and neuropathy from patients being left too long on the bed pan. Unfortunately, managing the bed pan is not easy for the nurse when patients are obese and have limitations in movement; plus spillage of the contents is a major problem.
Media
(Click Image to Enlarge)
References
Kozak A, Freitag S, Nienhaus A. Evaluation of a Training Program to Reduce Stressful Trunk Postures in the Nursing Professions: A Pilot Study. Annals of work exposures and health. 2017 Jan 1:61(1):22-32. doi: 10.1093/annweh/wxw002. Epub [PubMed PMID: 28395308]
Level 3 (low-level) evidenceFarrington N, Hill T, Fader M, Richardson A. Supporting women with toileting in palliative care: use of the female urinal for bladder management. International journal of palliative nursing. 2016 Nov 2:22(11):524-533 [PubMed PMID: 27885906]
Inauen P, Wittwer Y, Saxer S. [Research report: urination tubes instead of bedpan]. Krankenpflege. Soins infirmiers. 2011:104(10):22-3 [PubMed PMID: 21991769]
Saxer S, Gattinger HA, Dopler R, Scheffel S, Werner B. [Frequency of using the bedpan in acute care]. Pflege. 2011 Oct:24(5):297-302. doi: 10.1024/1012-5302/a000142. Epub [PubMed PMID: 21964933]
Level 2 (mid-level) evidencePellatt GC. Anatomy and physiology of urinary elimination. Part 1. British journal of nursing (Mark Allen Publishing). 2007 Apr 12-25:16(7):406-10 [PubMed PMID: 17505362]
Bekhøj L, Eltzholtz AB. [Hygiene nurse--when bedpan boilers break down]. Sygeplejersken. 1997 Aug 22:97(34):26-7 [PubMed PMID: 9386588]
Sonoda T, Masumoto T. [Innovation in nursing equipment. A bathroom for the orthopedic department]. [Kango gijutsu] : [Nursing technique]. 1980 Oct:26(14):1934-5 [PubMed PMID: 6904593]
BRANSON HK. THE BEDPAN RECONSIDERED. Hospital management. 1964 Jul:98():78 PASSIM [PubMed PMID: 14154394]
Guay M, Dubois MF, Desrosiers J. Can home health aids using the clinical algorithm Algo choose the right bath seat for clients having a straightforward problem? Clinical rehabilitation. 2014 Feb:28(2):172-82. doi: 10.1177/0269215513494027. Epub 2013 Jul 29 [PubMed PMID: 23897948]
Putre L. Lifting spirits with bedpan shuffleboard. Hospitals & health networks. 2013 Jan:87(1):63 [PubMed PMID: 23413624]