Introduction
Otic ganglion is one of the four parasympathetic ganglia within the head region. An anatomist named Arnold first described it in 1828. It was called 'otic' as it was large in long-eared mammals such as donkey, rabbit, horse, and other ruminants.[1]
The otic ganglion has parasympathetic, sympathetic, sensory, and motor roots. The otic ganglion transmits postganglionic parasympathetic secretomotor fibers to all branches of the mandibular division of the trigeminal nerve. It also sends sympathetic vasomotor fibers to the parotid gland. Innervation to tensor veli palatini, tensor tympani, and medial pterygoid muscle also occurs via a motor root of otic ganglion.[2] The neurons of otic ganglion derive from Schwann cell precursors.[3] Frey's syndrome can occur following damage to postganglionic nerve fibers from otic ganglion at the level of either auriculotemporal nerve or parotid gland.[4]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Located in the infratemporal fossa, the otic ganglion is the smallest of the four parasympathetic ganglia found in the head region. It is an oval but flat ganglion and approximately 2×1.5×0.4 mm in size. It lies inferomedial to the foramen ovale.[5] The ganglion is inferior to the greater wing of sphenoid and superior to the levator veli palatini muscle. It is related to the medial surface of the mandibular nerve laterally, and the cartilage of the auditory tube lies in its medial aspect. The medial pterygoid nerve runs anterior to the ganglion, and middle meningeal artery traverses posterior to it.[6] Even though the otic ganglion is related topographically related to the mandibular nerve, functionally, it is related to the glossopharyngeal nerve.[7]
Morphologically, the otic ganglion is seen as a yellowish-brown oval ganglionic structure bilaterally in most cases.[8] However, recent studies have shown that otic ganglion can appear as three types:
- Compact type
- Lobulated type
- Disperse type based on how the nerves enter and leave the ganglion
The compact type has a classic ganglionic shape and is the most common type. As the number of leaving branches increases, the ganglion appears less lobulated and more disperse. In the same individual, two different morphological types of a ganglion can both be present.[6]
The parasympathetic root of an otic ganglion is formed by preganglionic parasympathetic fibers that arise in the inferior salivary nucleus, located within the medulla oblongata of the brainstem. These preganglionic efferent parasympathetic fibers pass through the glossopharyngeal nerve. They then travel with its tympanic branch (Jacobson’s nerve) to form tympanic plexus in the middle ear cavity, before leaving it to form the lesser petrosal nerve.[2][9] The lesser petrosal nerve course along the floor of middle cranial fossa and exits the skull base through foramen ovale to enter the infratemporal fossa and join the otic ganglion. In some cases, the lesser petrosal nerve also exits the middle cranial fossa through foramen spinosum or sphenopetrosal fissure to joins the otic ganglion.[9] Within the otic ganglion, preganglionic parasympathetic fibers synapse with the postganglionic fibers. The postganglionic parasympathetic fibers then traverse through all branches of the mandibular division of trigeminal nerve to provide secretomotor fibers to mainly the parotid gland via the auriculotemporal nerve. It also supplies other areas of the orofacial region like the submandibular gland, sublingual gland, other salivary glands in the buccal mucosa, and blood vessels of the masticatory muscles through the other branches of the mandibular nerve.[10]
The origin of sympathetic neurons associated with the otic ganglion arises from the plexus around the middle meningeal artery. These plexus convey postganglionic fibers arising from the superior cervical ganglion. The postganglionic sympathetic fibers pass through the otic ganglion without relay and run together with the parasympathetic fibers in the auriculotemporal nerve to provide sympathetic innervation to the parotid gland blood vessels.[2]
The sensory route of the otic ganglion receives fibers from the glossopharyngeal nerve via the tympanic plexus and lesser superficial petrosal nerve.[2][8]
The motor route originates from the mandibular nerve and passes through the otic ganglion without synapsing and enters the medial pterygoid nerve to innervate the medial pterygoid muscle, tensor veli palatini, and tensor tympani muscles.[2]
Embryology
Otic ganglion, like other parasympathetic ganglia within the head, is derived from Schwann cell precursors. These precursors migrate via preganglionic axons and differentiate into peripheral neurons when they reach the site of the adult ganglionic structure into which they develop.[3][11] By 32 to 34 days of embryonic life, otic ganglia are observable in humans, and by the 20th week of intra-uterine life, it will be a well-developed structure.[6]
It has recently come to light that the otic ganglion and pterygopalatine ganglia are a single and undifferentiated cell mass till the 16th week of gestation and later get separated by growing ala temporalis. They then reconnect by secondarily-formed communicating branch, the nervus sphenopidalis.[7]
Blood Supply and Lymphatics
Research has shown that the postganglionic fibers emerging from the otic ganglion innervate the blood vessels of the circle of Willis as opposed to the vertebrobasilar artery. The postganglionic otic fibers also terminate in the cavernous sinus via the external sphenoid nerve and form the cavernous sinus plexus with the sympathetic fibers from the internal carotid artery.[12] Research has also proven that, in rats, the middle meningeal artery and superficial temporal artery receive afferents from the otic ganglion through the auriculotemporal nerve.[6]
A recent study clearly shows that blood vessels in the lower lip exclusively receive innervation by postganglionic fibers originating from the otic ganglion, and not from the pterygopalatine ganglion.[13]
Nerves
Otic ganglion has connections to various nerves. This section describes the multiple nerves connected to the otic ganglion and the structures innervated by them. Postganglionic parasympathetic fibers of the otic ganglion pass through all the branches of the mandibular division of the trigeminal nerve, like the auriculotemporal nerve, lingual nerve, buccal nerve, inferior alveolar nerve, mylohyoid nerve, meningeal nerve, and the motor branches to deep temporalis and masseter. The otic ganglion also communicates with the Vidian nerve through the internal sphenoid nerve and cavernous sinus through the external sphenoid nerve.[6]
The auriculotemporal nerve, which connects to the otic ganglion through a communicating branch carries postganglionic parasympathetic secretomotor and sympathetic vasomotor fibers for the parotid gland.[2]
The motor fibers of the facial nerve for levator veli palatini muscle run in the cauda tympani nerve and then the otic ganglion by a communicating branch. These motor fibers pass the otic ganglion without any synaptic relay and join the Vidian nerve via the internal sphenoid nerve. Vidian nerve finally brings the motor fibers to the pterygopalatine ganglion, which eventually gives of the lesser palatine nerve to innervate the levator veli palatini muscle.[2]
The postganglionic fibers from the otic ganglion also enter the lingual nerve via a communicating branch and thereby innervates the submandibular and sublingual glands. The greater petrosal nerve is also connected to the otic ganglion by a communicating branch and transmits sensory and parasympathetic fibers to the lingual nerve. The otic ganglion also connects to the meningeal branch of the mandibular nerve through a communicating branch, and it transmits sensory fibers that form the meningeal nerve.[2]
The otic ganglion connects to the cavernous sinus through the external sphenoid nerve. The external sphenoid nerve is a small ganglion cord arising from the dorsal side of the otic ganglion. It accompanies the internal sphenoid nerve along half its course. It then traverses cranially to enter the cavernous sinus through sphenoidal emissary foramen, or through a small bony canal where a para-otic ganglion resides.[2]
Postganglionic parasympathetic fibers from the otic ganglion also run in other branches of the mandibular nerve like buccal, inferior alveolar, and mylohyoid nerve, and they innervate the small salivary glands in the buccal mucosa. The motor branches of the mandibular nerve to masseter and deep temporalis also contains postganglionic parasympathetic fibers from the otic ganglion to a small extent.[10]
Muscles
The motor route of otic ganglion innervates three muscles via the medial pterygoid nerve, namely tensor tympani, tensor veli palatine, and medial pterygoid muscles.[2]
Physiologic Variants
The otic ganglion showed a difference in the number and volume of nerve fiber bundles connected to it, which in turn resulted in three different morphological forms described above.[14][6] The otic ganglion also showed a disparity in the distance to the anterior section of the mandibular nerve, and it varied from 0 to 4 mm.[14]
Clinical Significance
Frey’s (auriculotemporal) syndrome occurs following surgery, trauma, or any pathology to the parotid gland or the auriculotemporal nerve that, in turn, damages the postganglionic parasympathetic, sympathetic and sensory nerves within them. Very rarely, Frey’s syndrome can occur following herpes infection.[15] The patients present with unilateral pain, sweating, and flushing in the cutaneous distribution of the auriculotemporal nerve following a gustatory stimulus. Many theories are in place to explain the phenomenon observed in Frey syndrome. The most accepted among them states the cause behind this phenomenon to be aberrant regeneration. Following damage to the auriculotemporal nerve, the regenerating nerve fibrils may become misdirected and join the sympathetic nerves innervating subcutaneous blood vessels and sweat glands, causing gustatory sweating and flushing.[4] Sometimes these symptoms can appear many decades after a parotidectomy surgery [16]. Confirmation of Frey syndrome is possible with a Minor starch-iodine test. Many surgical methods are available for the prevention of Frey syndrome, including the use of fascia or muscle flaps, fat grafts, or acellular dermal matrix (ADM). The different treatment options for Frey syndrome include the topical application of antiperspirants, injection of anticholinergics like scopolamine and intradermal injections of botulinum toxin A.
Preganglionic parasympathetic fibers projecting to the otic ganglion may be damaged by traumatic injury or inflammation involving foramen ovale, causing dysfunction of the parotid gland and other areas in which the postganglionic parasympathetic fibers innervate.[2]
Recent studies have shown the presence of neuropeptide, pituitary adenylate cyclase-activating peptide (PAC-AP) in the otic ganglion, which plays a significant role in primary headache.[6]
Media
(Click Image to Enlarge)
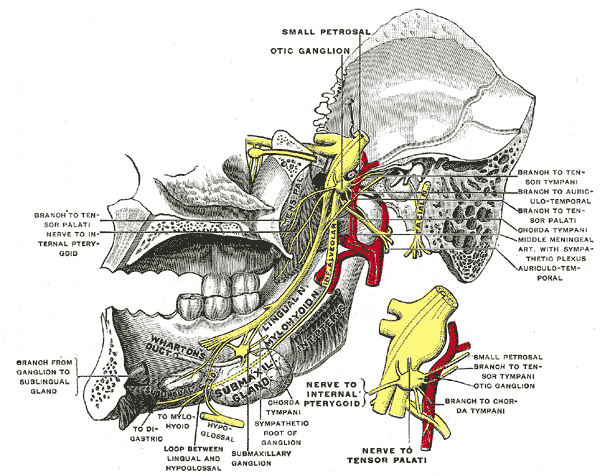
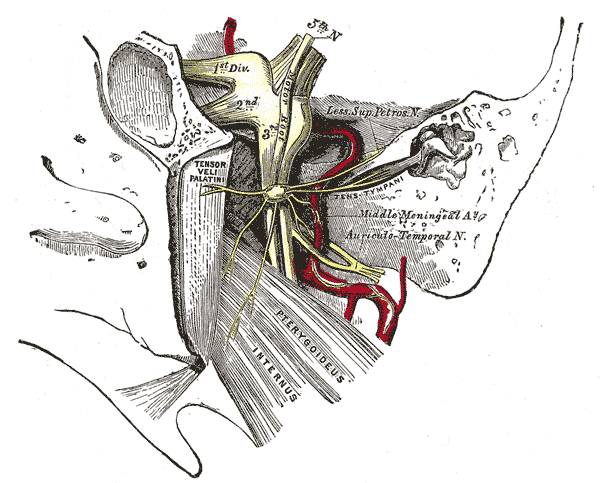
The Trigeminal Nerve. Mandibular division of trifacial nerve is seen from the middle line.The small figure is an enlarged view of the otic ganglion.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Tylee WS. Anatomical and Physiological Description of the Otic Ganglion. Edinburgh medical and surgical journal. 1833 Jul 1:40(116):21-31 [PubMed PMID: 30331732]
Senger M, Stoffels HJ, Angelov DN. Topography, syntopy and morphology of the human otic ganglion: a cadaver study. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2014 Sep:196(5):327-35. doi: 10.1016/j.aanat.2014.05.039. Epub 2014 Jun 10 [PubMed PMID: 24973995]
Espinosa-Medina I, Outin E, Picard CA, Chettouh Z, Dymecki S, Consalez GG, Coppola E, Brunet JF. Neurodevelopment. Parasympathetic ganglia derive from Schwann cell precursors. Science (New York, N.Y.). 2014 Jul 4:345(6192):87-90. doi: 10.1126/science.1253286. Epub 2014 Jun 12 [PubMed PMID: 24925912]
Level 3 (low-level) evidenceHarper KE, Spielvogel RL. Frey's syndrome. International journal of dermatology. 1986 Oct:25(8):524-6 [PubMed PMID: 3771053]
Level 3 (low-level) evidenceFerreira JN, Hoffman MP. Interactions between developing nerves and salivary glands. Organogenesis. 2013 Jul-Sep:9(3):199-205. doi: 10.4161/org.25224. Epub 2013 Jun 6 [PubMed PMID: 23974175]
Level 3 (low-level) evidenceBandke D, Ebauer K, Ebauer A, Weis S. Pre- and postnatal development of the otic ganglion in humans. Journal of anatomy. 2019 Jan:234(1):33-42. doi: 10.1111/joa.12898. Epub 2018 Nov 8 [PubMed PMID: 30411352]
Yamamoto M, Ho Cho K, Murakami G, Abe S, Rodríguez-Vázquez JF. Early Fetal Development of the Otic and Pterygopalatine Ganglia with Special Reference to the Topographical Relationship with the Developing Sphenoid Bone. Anatomical record (Hoboken, N.J. : 2007). 2018 Aug:301(8):1442-1453. doi: 10.1002/ar.23833. Epub 2018 May 4 [PubMed PMID: 29669195]
Roitman R, Talmi YP, Finkelstein Y, Sadov R, Zohar Y. Anatomic study of the otic ganglion in humans. Head & neck. 1990 Nov-Dec:12(6):503-6 [PubMed PMID: 2258290]
Kakizawa Y, Abe H, Fukushima Y, Hongo K, El-Khouly H, Rhoton AL Jr. The course of the lesser petrosal nerve on the middle cranial fossa. Neurosurgery. 2007 Sep:61(3 Suppl):15-23; discussion 23 [PubMed PMID: 17876229]
Segade LA, Suarez Quintanilla D, Suarez Nuñez JM. The postganglionic parasympathetic fibers originating in the otic ganglion are distributed in several branches of the trigeminal mandibular nerve: an HRP study in the guinea pig. Brain research. 1987 May 19:411(2):386-90 [PubMed PMID: 3607441]
Level 3 (low-level) evidenceDyachuk V, Furlan A, Shahidi MK, Giovenco M, Kaukua N, Konstantinidou C, Pachnis V, Memic F, Marklund U, Müller T, Birchmeier C, Fried K, Ernfors P, Adameyko I. Neurodevelopment. Parasympathetic neurons originate from nerve-associated peripheral glial progenitors. Science (New York, N.Y.). 2014 Jul 4:345(6192):82-7. doi: 10.1126/science.1253281. Epub 2014 Jun 12 [PubMed PMID: 24925909]
Level 3 (low-level) evidenceSuzuki N, Hardebo JE. The pathway of parasympathetic nerve fibers to cerebral vessels from the otic ganglion in the rat. Journal of the autonomic nervous system. 1991 Oct:36(1):39-46 [PubMed PMID: 1753063]
Level 3 (low-level) evidenceIzumi H. Reflex parasympathetic vasodilatation in facial skin. General pharmacology. 1995 Mar:26(2):237-44 [PubMed PMID: 7590072]
Level 3 (low-level) evidenceSiéssere S, Vitti M, Sousa LG, Semprini M, Iyomasa MM, Regalo SC. Anatomic variation of cranial parasympathetic ganglia. Brazilian oral research. 2008 Apr-Jun:22(2):101-5 [PubMed PMID: 18622477]
Shah JS, Asrani VK. Post Herpetic Frey's Syndrome. Annals of maxillofacial surgery. 2017 Jul-Dec:7(2):278-281. doi: 10.4103/ams.ams_86_17. Epub [PubMed PMID: 29264298]
Chamisa I. Frey's syndrome--unusually long delayed clinical onset post-parotidectomy: a case report. The Pan African medical journal. 2010 Apr 7:5():1 [PubMed PMID: 21120000]
Level 3 (low-level) evidence