Introduction
Paget Schroetter syndrome (PSS) is effort-induced thrombosis of the axillary and subclavian veins associated with compression of the subclavian vein at the thoracic outlet. It is the venous variant of thoracic outlet syndrome (TOS), the syndrome of symptoms associated with compression of the subclavian vein, subclavian artery, or brachial plexus as they pass through the thoracic outlet. The description of this entity dates back to 1875 when Sir James Paget reported a case of spontaneous thrombosis of the subclavian vein in a patient. In 1884, von Schroetter hypothesized that the condition was a consequence of injury to the vein from repetitive musculoskeletal motion.[1][2][3][4][5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
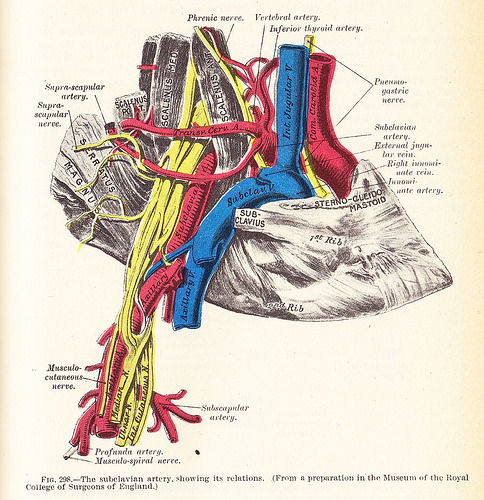
The subclavian vein travels in the proximity of the clavicle, first rib, anterior scalene, and subclavius muscles. PSS is related to the compression and subsequent thrombosis of the subclavian vein due to these structures.
Epidemiology
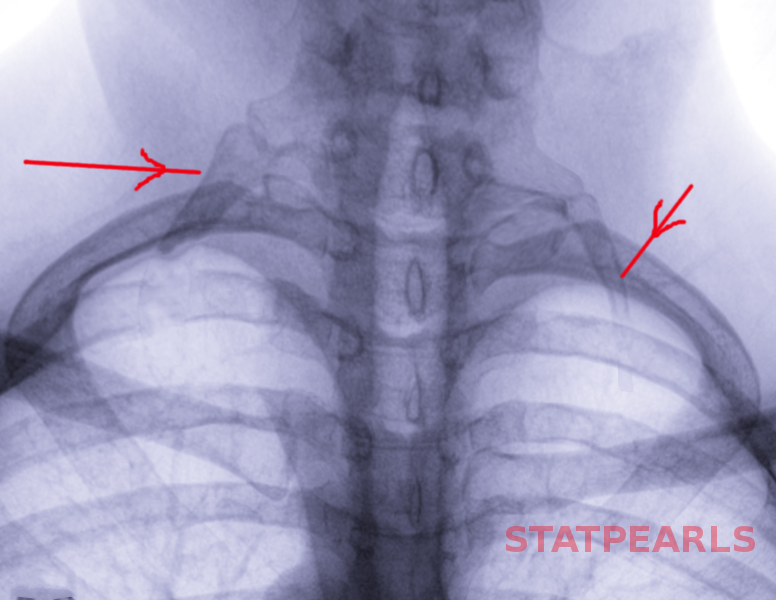
PSS is more commonly seen in younger patients (in their 20s and 30s) with a male to female ratio of 2:1. Often these patients will not have any other significant medical comorbidities. The incidence ranges from 1 to 2 per 100,000 individuals per year in various studies. It is more commonly encountered on the right side. Venous TOS is less common than neurogenic TOS but more common than arterial TOS. Often affected individuals with PSS will be athletes, specifically, those engaged in the repetitive over-the-head motion of their arms, including baseball or softball pitchers, swimmers, rowers, or weightlifters.
Pathophysiology
Repetitive strain from vigorous physical activity and compression of the subclavian vein from adjacent anatomic structures leads to venous injury and subsequent thrombosis. This impedes the venous return from the affected extremity leading to edema. Over time, the body forms collaterals to bypass the venous obstruction. In the chronic phase, the vein becomes fibrotic. Surrounding inflammatory changes from the thrombosis lead to scar tissue formation.[6][7][8][9]
History and Physical
Patients may present with upper extremity swelling and pain. The presentation of these symptoms can be acute, subacute, or chronic. For the onset of symptoms in PSS, a history of an antecedent strenuous exercise can usually be elicited from the patients. On examination, the upper extremity will demonstrate edema with an enlarged girth of the extremity compared to the contralateral side. The upper extremity may be tense and cyanotic. Additionally, venous collaterals may be seen on the chest and around the shoulder (Urschel’s sign).
Evaluation
A convenient non-invasive first test is ultrasonography of the upper extremities. This will demonstrate thrombus in the deep venous system. Acute thrombus will be non-compressible on ultrasound. Additionally, it will be echogenic with a distended appearance of the vein and absent spectral/color flow. A vein with chronic thrombus will have an irregular and more collapsed appearance with the development of collaterals on ultrasound. Ultrasonography will not allow for complete demonstration of the central veins. Computed tomography (CT) venography and magnetic resonance (MR) venography can demonstrate thrombus in the venous system as well. Contrast venography is a more invasive test that can demonstrate patency of the central venous system.
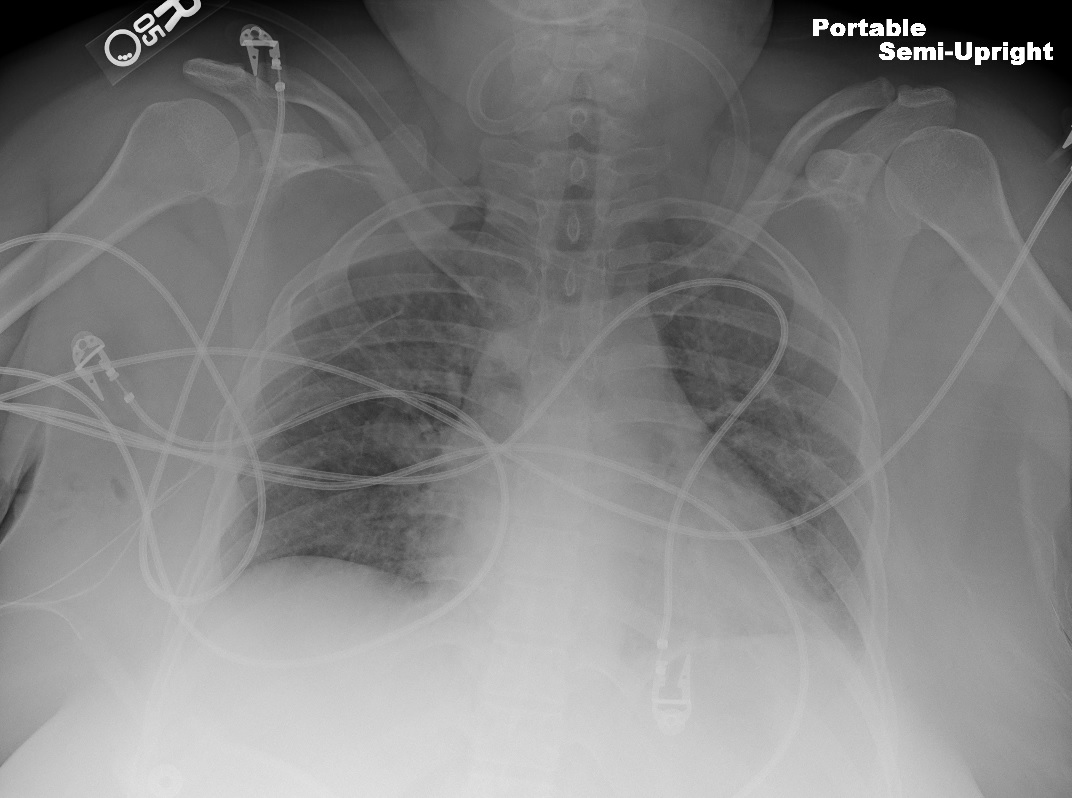
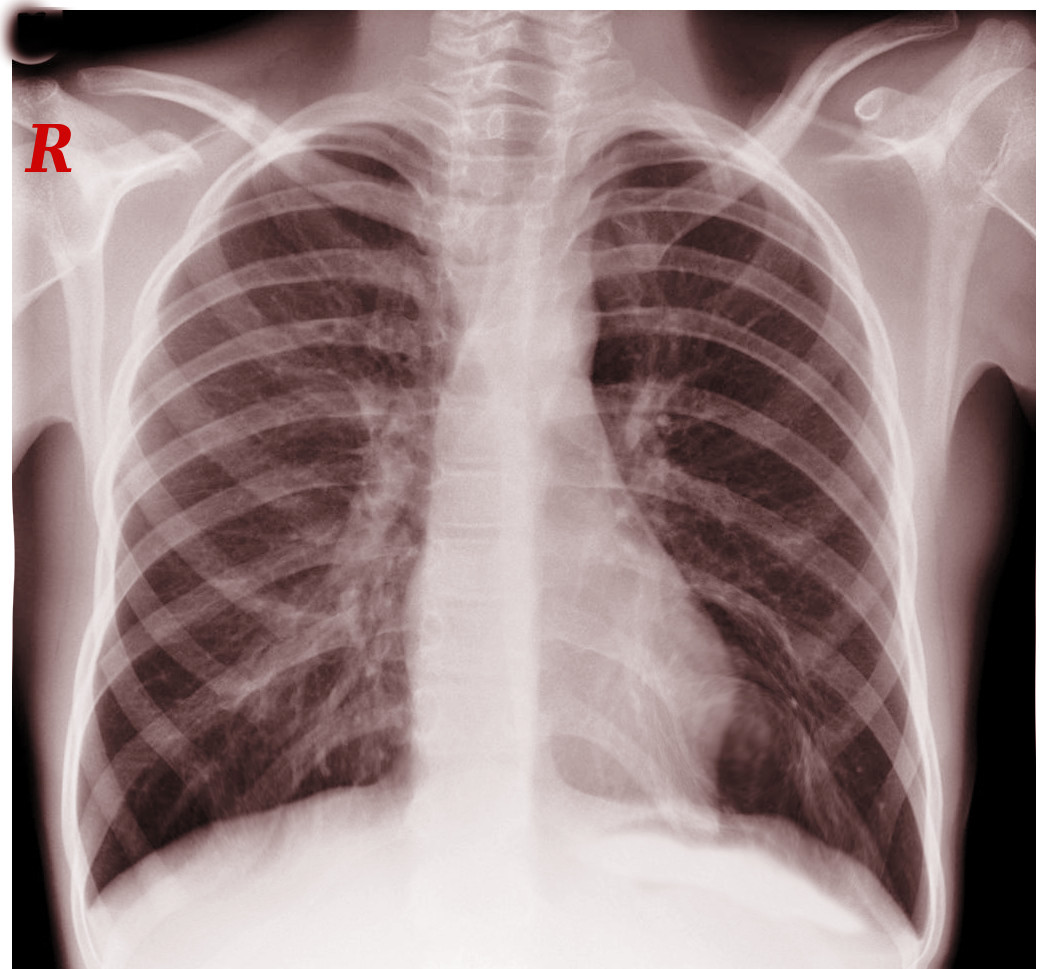
Laboratory workup includes a thrombophilia panel (protein C and S levels, antithrombin levels, prothrombin gene mutation analysis, factor V Leiden mutation testing, among others) and D-dimer levels. D-dimer levels will be elevated in a patient with deep venous thrombosis; however, this elevation can also be seen in other infectious, inflammatory, and physiologic conditions. If the patients have any symptoms concerning for a pulmonary embolism, a CT angiogram (CTA) thorax with pulmonary embolism protocol should be obtained. Alternatively, a ventilation-perfusion study can diagnose pulmonary embolism as well, but CTA thorax remains the study of choice.
Treatment / Management
PSS is a deep venous thrombosis, and, as such, the first step in the management is to initiate anticoagulation therapy, typically, via an intravenous (IV) heparin drip. Patients are given an initial bolus of intravenous (IV) heparin and then kept on a maintenance IV heparin drip. The dose of the bolus and maintenance heparin drip is weight-based. The IV heparin drip is titrated according to APTT levels or factor X levels. The affected extremity should be elevated to mitigate edema. If the patient presents within 2 weeks of the onset of symptoms, it is reasonable to consider a venogram and catheter-directed thrombolysis to reduce the clot burden. Under fluoroscopic guidance, a lysis catheter is placed to drip a thrombolytic agent such as alteplase for 24 to 48 hours. Alternatively, a pharmacomechanical thrombectomy system can be used. When using alteplase, the fibrinogen levels should be monitored closely to direct the dosing and duration of the catheter-directed lysis. When using pharmacomechanical thrombectomy, one should be mindful of the risk of acute kidney injury associated with hemolysis. If the presentation is more than 2 to 4 weeks from the onset of symptoms, heparinization alone may be initiated without thrombolytic therapy as the success of thrombolytic therapy is low beyond that window of time.[10][11][12](B3)
Another option for treatment is mechanical catheter-directed thrombectomy. This must be done early in the course of the disease.[13]
Decompression of the thoracic outlet is the definitive management of PSS. This usually includes a first rib resection with some or all of the following procedures: anterior scalenectomy, resection of the subclavius muscle, resection of the costoclavicular ligament, and lysis of scar tissue/adhesions surrounding the subclavian vein. Venoplasty and/or stenting without decompression may produce favorable results but rib resection is the definitive treatment. The surgical approach can either be transaxillary or supra, infra, or para-clavicular. The timing of decompression after thrombolytic therapy is widely debated. The role of long-term anticoagulation in these patients after adequate decompression remains unclear. Some clinicians perform a venogram, often with intravascular ultrasound, 2 weeks postoperatively and decide about the duration of anticoagulation at that time. In this setting, venoplasty can be used for any residual stenosis since decompression has been achieved surgically. The use of stents is discouraged in this anatomic location due to the repetitive motion and risk of stent fracture and thrombosis.
The duration of anticoagulation in patients with underlying hypercoagulability disorders after decompression also remains unclear. In most patients, anticoagulation for 3 to 6 months following an episode of deep venous thrombosis such as PSS is reasonable. This can be achieved either via warfarin or direct oral anticoagulants (DOAC). In the case of recurrent thrombosis after decompression surgery, thrombolysis and venography are usually attempted again with the maintenance of long-term anticoagulation therapy afterward. In some patients with PSS, chronic total occlusion of the subclavian vein may persist despite adequate decompression maneuvers. Depending on the severity of the symptoms, venous reconstruction should be considered. This can be achieved with a bypass or jugular vein turndown procedure (with or without medial claviculectomy).
Differential Diagnosis
Upper extremity swelling may be present in patients with lymphatic disorders or systemic conditions such as end-stage renal disease and congestive heart failure. Upper extremity deep venous thrombosis can be seen with indwelling catheters as well.
Prognosis
A combination of thrombolysis and thoracic outlet decompression may be successful in up to 90% of the patients. Anticoagulation with decompression is less successful than thrombolysis and decompression but still yields better results than anticoagulation alone.
Complications
- Pulmonary embolism
- Post-thrombotic syndrome
- Recurrent thrombosis
Deterrence and Patient Education
Patients should be encouraged to adhere to all medication recommendations and have close follow up with all of their healthcare providers. Activity and lifestyle modification may reduce the risk of recurrent thrombosis. Patients with hypercoagulable states should be made aware that they may need long-term anticoagulation.
Enhancing Healthcare Team Outcomes
The diagnosis and management of PSS are best accomplished with an interprofessional team that consists of a primary care provider, sports medicine clinician, vascular surgeon, and radiologist. Patients with venous obstruction do need treatment or the arm will remain swollen and painful. After anticoagulation, decompression of the thoracic outlet is often required. Most patients do have a good outcome with treatment but depending on the state of the subclavian vein, some degree of arm swelling may persist. Today, for some cases of PSS, endovascular therapy is available.[14]
Media
(Click Image to Enlarge)
References
Sayın A,Güngör H,Bilgin M,Ertürk U, Paget-von Schrötter syndrome: upper extremity deep vein thrombosis after heavy exercise. Turk Kardiyoloji Dernegi arsivi : Turk Kardiyoloji Derneginin yayin organidir. 2012 Jun; [PubMed PMID: 22951853]
Level 3 (low-level) evidenceLewandowski A,Syska-Sumińska J,Dłuzniewski M, [Pulmonary embolism suspicion in a young female patient with the Paget-von Schrötter syndrome]. Kardiologia polska. 2008 Sep; [PubMed PMID: 18924025]
Level 3 (low-level) evidenceZell L,Sommerfeld A,Buchter A, [The Paget-von Schroetter syndrome. On the centenary of the death of Sir James Paget and on the 50th anniversary of the naming of the syndrome]. Deutsche medizinische Wochenschrift (1946). 1999 Aug 6; [PubMed PMID: 10480017]
Cires-Drouet R,Sharma J,McDonald T,Sorkin JD,Lal BK, Variability in the management of line-related upper extremity deep vein thrombosis. Phlebology. 2019 Jan 31; [PubMed PMID: 30704347]
Weaver LA,Kanter CR,Costantino TG, Effort Thrombosis Provoked by Saxophone Performance. The Journal of emergency medicine. 2019 Jan 8; [PubMed PMID: 30638648]
Thiyagarajah K,Ellingwood L,Endres K,Hegazi A,Radford J,Iansavitchene A,Lazo-Langner A, Post-thrombotic syndrome and recurrent thromboembolism in patients with upper extremity deep vein thrombosis: A systematic review and meta-analysis. Thrombosis research. 2019 Feb; [PubMed PMID: 30553163]
Level 1 (high-level) evidenceKumar R,Harsh K,Saini S,O'Brien SH,Stanek J,Warren P,Giver J,Go MR,Kerlin BA, Treatment-Related Outcomes in Paget-Schroetter Syndrome-A Cross-Sectional Investigation. The Journal of pediatrics. 2018 Dec 7; [PubMed PMID: 30528572]
Level 2 (mid-level) evidenceChen AWY,Oraii Yazdani K,Candilio L, Upper Limb Deep Vein Thrombosis: A Case Report of an Increasingly Common Condition. The journal of Tehran Heart Center. 2018 Apr; [PubMed PMID: 30483316]
Level 3 (low-level) evidenceLim W,Le Gal G,Bates SM,Righini M,Haramati LB,Lang E,Kline JA,Chasteen S,Snyder M,Patel P,Bhatt M,Patel P,Braun C,Begum H,Wiercioch W,Schünemann HJ,Mustafa RA, American Society of Hematology 2018 guidelines for management of venous thromboembolism: diagnosis of venous thromboembolism. Blood advances. 2018 Nov 27; [PubMed PMID: 30482764]
Level 3 (low-level) evidenceWooster M,Fernandez B,Summers KL,Illig KA, Surgical and endovascular central venous reconstruction combined with thoracic outlet decompression in highly symptomatic patients. Journal of vascular surgery. Venous and lymphatic disorders. 2019 Jan; [PubMed PMID: 30442583]
Fenando A,Mujer M,Rai MP,Alratroot A, Paget-Schroetter syndrome. BMJ case reports. 2018 Nov 8; [PubMed PMID: 30413468]
Level 3 (low-level) evidenceGwozdz AM,Silickas J,Smith A,Saha P,Black SA, Endovascular Therapy for Central Venous Thrombosis. Methodist DeBakey cardiovascular journal. 2018 Jul-Sep; [PubMed PMID: 30410652]
Kärkkäinen JM,Nuutinen H,Riekkinen T,Sihvo E,Turtiainen J,Saari P,Mäkinen K,Manninen H, Pharmacomechanical Thrombectomy in Paget-Schroetter Syndrome. Cardiovascular and interventional radiology. 2016 Sep; [PubMed PMID: 27230515]
Garg V,Poon G,Tan A,Poon KB, Paget-Schroetter syndrome as a result of 1st rib stress fracture due to gym activity presenting with Urschel's sign - A case report and review of literature. International journal of surgery case reports. 2018; [PubMed PMID: 29966955]
Level 3 (low-level) evidence