Introduction
Lipemia retinalis (LR) is a retinal manifestation of chylomicronemia (hypertriglyceridemia). Ophthalmoscopic features are creamy-white discoloration of the retinal vessels, which start in the peripheral vessels in mild cases and involves central retinal vessels in established cases. In severe cases, the fundus takes salmon color. Though lipemia retinalis does not affect the visual acuity, the associated severe but easily treatable metabolic disorders merit discussion.[1] This review discusses the etiology, epidemiology, pathophysiology, histopathology, evaluation, management, and prognosis of this condition.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Heyl, in 1880 described a case of lipemia retinalis (LR) in detail.[2] Vinger and Sachs described different grades of LR in 1970.[3] There are five classes of lipid transport molecules or lipoprotein. These are chylomicrons, very-low-density lipoproteins (VLDL), intermediate-density lipoproteins (IDL), low-density lipoproteins (LDL), and high-density lipoproteins (HDL) and their sizes are 100 to 1000 nm, 34 nm, 27 nm, 22 nm, and 5 to 12 nm respectively. Smaller lipoprotein molecules do not scatter light and are transparent. Chylomicrons are the largest lipoprotein macromolecules. Most of the dietary triglyceride is transported from intestine to the systemic circulation via chylomicrons. Chylomicrons are normally rapidly removed from the plasma. It is likely the high proportion of triglycerides in chylomicrons, which leads to the association of raised triglyceride levels and lipemia retinalis. If a sample of hyperlipidemic serum is allowed to stand, chylomicrons form a hazy surface layer. Circulating blood with a high level of chylomicrons gives the appearance of lipemia retinalis due to the light scattering effect of the chylomicrons in the retinal vessels.[4] Hypertriglyceridemia (HTG) can be primary familial or secondary to other diseases. Multiple genes responsible for abnormal triglyceride metabolism, causing HTG has been identified.[1] The initial changes of LR occur in the peripheral retinal vessels, and gradually the changes progress to involve the entire fundus.[3] HTG and chylomicronemia may lead to severe diseases like acute pancreatitis. However, in chylomicronemia, the whole blood is turbid and appears milky compared to fat embolism (after fracture of long bones) where there are large colorless globules in the blood that can cause vascular blockages leading to different retinal manifestations like Purtscher-like retinopathy.[2][5]
Chylomicronemia has been noted to occur when the plasma triglyceride level is higher than 1000 mg/dl.[6] Chylomicronemia syndrome is defined by the presence of 1 or more of the following, along with chylomicronemia[6]:
- Eruptive xanthoma
- Lipemia retinalis
- Abdominal pain and/or pancreatitis
However, some authors consider a triglyceride level of 2000 mg/dl as a lower cutoff while defining chylomicronemia and chylomicronemia syndrome.[7] According to these authors (Brunzell and Bierman), features of chylomicronemia syndrome included[7]:
- Lipemia retinalis in 23%
- Flushing with alcohol in 25%
- Documented pancreatitis in 28%
- Eruptive xanthoma in 40%
- Objective dyspnea in 46%
- Abdominal pain and/or pancreatitis in 63%
- Recent memory loss in 85% of patients
Elevation of plasma triglycerides is the main etiology of LR. HTG can be familial or secondary to other diseases.
Familial HTG occurs due to:
- The presence of endogenous circulating lipoprotein lipase ( LPL ) inhibitor
- Deficiency of LPL
- Deficiency of apoprotein of LPL i.e., APOC-II. LPL deficiency is an autosomal recessive transmission due to a number of LPL gene mutations like Asp9Asn, Gly188Glu, Pro207Leu, Asp250Asn, Asn291Ser, Ser447X, Pro214Ser, and others.[8]
Secondary causes of HTG include[9]:
- Uncontrolled type 1 or type 2 diabetes mellitus
- Endocrine disorders (obesity, metabolic syndrome, hypothyroidism, hypercortisolism)
- Medications (corticosteroids, estrogen, antipsychotics (clozapine and olanzapine), antidepressants, rosiglitazone, thiazides, beta-blockers, bile acid sequestrants, sirolimus, antiretroviral therapy,13-cis-retinoic acid, tamoxifen)
- Pregnancy
- Renal disease (nephrotic syndrome, renal failure, renal dialysis)
- Liver disease (acute hepatitis)
- Dietary intake (high in saturated fats and carbohydrates, excessive alcohol intake)
- Systemic diseases (Human immunodeficiency virus infection, acute spinal cord injury, anorexia nervosa, organ transplant, sarcoidosis, systemic lupus erythematosus, myeloma)
Epidemiology
Though the exact epidemiology of lipemia retinalis is not known, that of the associated risk factors have been mentioned. The deficiency of lipoprotein lipase results in familial HTG and high levels of chylomicrons in the serum. The incidence of LPL deficiency is less than 1 in 1 million.[10] LR may also be one of the manifestations of familial combined hyperlipidemia, which has a prevalence of 1% to 2% in the general population.[11] National Health and Nutrition Examination Survey reports from 2001 and 2006 mention that approximately 1.7% of the total U.S. population, or 3.4 million Americans, were estimated to have severe HTG (500 to 2,000 mg/dl). Individuals with severe HTG tended to be men (75.3%), non-Hispanic whites (70.1%) and aged 40 to 59 years (58.5%). Diabetes and hypertension were associated with 14% and 31.3% of cases of HTG, respectively.[12]
Pathophysiology
Hyperlipidemia without accompanying hypertriglyceridemia does not present lipemia retinalis.[13] The ocular findings result from light scatter induced by the triglyceride-laden chylomicrons in the plasma.[14] Chylomicronemia occurs when plasma triglycerides exceed more than 1000 mg/dl. Lipemia retinalis is always associated with elevated plasma triglycerides more than 2,000 mg/dL.[4][7]
At triglyceride levels of:
- 2500 to 3499 mg/dL- the peripheral vessels look creamy and thin
- 3500 to 5000 mg/dL- posterior pole vessels have a creamy color
- At levels more than 5000 mg/dL, the fundus has salmon-color. Differentiation of retinal arteries and veins may be difficult by color (both have creamy color). Though clinical differentiation of the retinal artery and vein is difficult in such cases, the caliber of the vessel may give a clue.[1]
Histopathology
The creamy appearance of the retinal vessels is due to the presence of triglyceride-laden chylomicrons in the plasma. Optical coherence tomography (OCT) scan through the retinal vessels gives evidence of the enlarged caliber of retinal vessels and back shadowing due to the presence of hyperreflective material inside the vessel lumen.[15] Extravasated lipid materials may represent as hyperreflective dots in the retinal layers.[15]
History and Physical
The patient is visually asymptomatic and lipemia retinalis is most often detected during a routine ophthalmic workup or workup of a referral case related to lipid abnormalities. Neonates and infants have been diagnosed as LR during screening and treatment for retinopathy of prematurity (ROP ).[16][17] A few case reports have described abdominal pain and gastrointestinal disorders as the presenting symptoms of hyperlipidemia in infants. These infants were found to have lipemia retinalis.[18] There may be a family history of hyperlipidemia due to various enzymatic and genetic disorders as mentioned above. Several secondary causes of HTG need to be ruled out by careful history and physical examination.
The physical examination should be done to look for evaluation of the cardiovascular system, the integumentary system, the abdomen, and the eye. Examination of the cardiovascular system includes the examination of heart sounds, carotid or renal bruits, and peripheral pulses. Characteristic skin lesions include xanthomas which are small yellowish papules, with an erythematous base, appearing predominantly on the buttocks and elbows due to deposition of large amounts of chylomicron triglycerides in cutaneous histiocytes. [19] Abdominal examination needs to be done for the assessment of hepatosplenomegally[18] and to rule out pancreatic disease. Ophthalmic evaluation should include the examination of the peri-orbital area, anterior segment, and posterior segment examinations.
- Examination of the periorbital area may reveal:
- Xanthelasma,
- Tuberous palpebral xanthomas
- Anterior segment findings, though rare, include:
- The dilated fundoscopic exam is needed for the diagnosis and staging of LR.
- Additional rare posterior segment findings of hyperlipoproteinemia include:
Evaluation
Laboratory evaluation of the fasting lipid profile is needed to diagnose HTG. The blood specimen for laboratory evaluation is lipemic, with a creamy white lipid layer seen in a standing tube of blood.[22] Turbid serum is due to the presence of chylomicrons in the plasma.[20] Genetic evaluation can be done to look for a number of LPL gene mutations.[8] Fundoscopy is needed for the diagnosis of LR, and fundus photography is helpful in the documentation and followup of the patients. Optical coherence tomography (OCT) scan of the retina in LR can indicate the indirect presence of chylomicrons in the retinal vessels.[15] Pretreatment decrease in amplitude of photopic and scotopic a and b waves have been documented in ERG. However, post-treatment reversal of these waves has been noted.[23] Fluorescein and indocyanine angiography testing are unremarkable.
Treatment / Management
Lipemia retinalis is sometimes transient and resolves within hours.[4] However, a prompt reversal of hyperlipidemia is the key to a better prognosis. Various measures can achieve this.(B3)
Dietary Restriction and Primary Prevention
Strict adherence to a low-fat diet without breast milk supplementation may be effective in treating infants with severe lipemia retinalis associated with HTG.[24] Reduction and control of serum triglyceride levels will prevent LR from developing. Correction of the lipid levels may reverse the abnormal findings within one week.(B3)
Medical Treatment
No treatment is required for the lipemia retinalis itself. However, LR is an important ocular sign of a life-threatening but easily treatable metabolic disorder. The treatment is to reduce the serum triglyceride levels to below 500 mg/dl. This can be accomplished by a number of medical treatments for lowering triglyceride and cholesterol. Several lipid-lowering drugs are used to treat HTG. First-line triglyceride-lowering medications include fibric acid derivatives (fibrates) and n-3 polyunsaturated fatty acids (i.e., fish oil).[25] Fibrates reduce triglycerides by 50%. The use of fibrates is contraindicated in those with hepatic or renal dysfunction.[26] N-3 polyunsaturated fatty acids reduce triglycerides by 50%, with little effect on other lipid fractions.[27] Gastrointestinal symptoms are the major side effects of this class of drugs. Nicotinic acid can decrease triglyceride levels by 15% to 35%.[28] Strict glycemic control is needed in patients with LR and diabetes.[9](A1)
Surgical Treatment
Surgery is not specifically indicated for the treatment of lipemia retinalis. However, exchange transfusion has been used in the setting of severe hypertriglyceridemia to reduce triglycerides in the acute setting.[29] Ileal bypass surgery has demonstrated improvement in all lipid parameters but should be reserved for refractory cases.[30]
Differential Diagnosis
The differential for lipemia retinalis includes 1) leukemia[2], 2) advanced diabetic eye disease with sclerotic vessels, 3) intravascular calcification of retinal vessels secondary to renal failure and hyperparathyroidism[31] 4) retinal branch retinal artery or vein occlusion, 5) hypertensive retinopathy, and 6) diffuse choroidal hemangioma (tomato catsup fundus seen in patients with diffuse hemangioma may resemble salmon fundus in LR). In leukemia, the veins are reddish pale, while the arteries are pale yellow. In lipemia, arteries and veins are of the same color and can be differentiated only by caliber. The veins are of a larger caliber.[2] In intravascular calcification secondary to renal failure or hyperparathyroidism, the disordered renal parameters, and parathyroid hormone level may be helpful in the proper diagnosis. On cursory exam, retinal vasculitis may be a differential, but vasculitis is usually segmental and associated with perivascular infiltrates and evidence of intraocular inflammation.
Staging
Staging of lipemia retinalis was given by Vinger and Sachs, which is as follows[3]:
- Grade I (early LR)- White and creamy appearance of peripheral retinal vessels
- Grade II (moderate LR)- Creamy colored vessels extending towards optic disc
- Grade III (marked LR)- Salmon colored retina, all vessels having a milky color
Prognosis
Retinal changes secondary to lipemia retinalis improve once serum triglyceride levels are normalized. Visual acuity is neither or minimally affected but improves well after the correction of the HTG. Reduced photopic and scotopic responses in electroretinogram are noted to improve after the correction of HTG.[23] These patients are at increased systemic risk for coronary artery disease, myocardial infarction and stroke, and increased ophthalmic risk for retinal artery and vein occlusions and retinal ischemia. So they should be followed up and monitored regularly.
Complications
Systemic complications of lipidemia retinalis due to hyperlipidemia include cardiovascular diseases, systemic hypertension, acute myocardial infarction, and stroke. Chylomicronemia may be associated with acute pancreatitis, abdominal pain, hepatosplenomegaly, dyspnea, and recent memory loss.
Ophthalmic complications are less frequently reported. These include retinovascular occlusions, retinal ischemia, causing neovascularization and vitreous hemorrhage.
Enhancing Healthcare Team Outcomes
The diagnosis and management of lipemia retinalis are not only important from an ophthalmological point of view but serious underlying genetic and metabolic disorders. The prompt diagnosis and management of hyperlipidemia results in the reversal of most of the symptoms and can prevent life-threatening complications like acute pancreatitis. The detection of a mutation of the LPL gene can help in genetic counseling of the parents of the affected child. Secondary causes like diabetes, hypothyroidism, obesity, chronic alcoholism, etc. need to be diagnosed and promptly treated. This management is possible only if there are proper communication and referral of the case between physicians, pediatricians, geneticists, endocrinologists, and ophthalmologists. The team can also include optometrists, laboratory technicians, and ophthalmology nurses. The laboratory technicians identify the unprocessed sample of blood in the test tube for any abnormal discoloration. The nurses participate in patient education and follow up, informing the ophthalmologist of any issues.
Media
(Click Image to Enlarge)
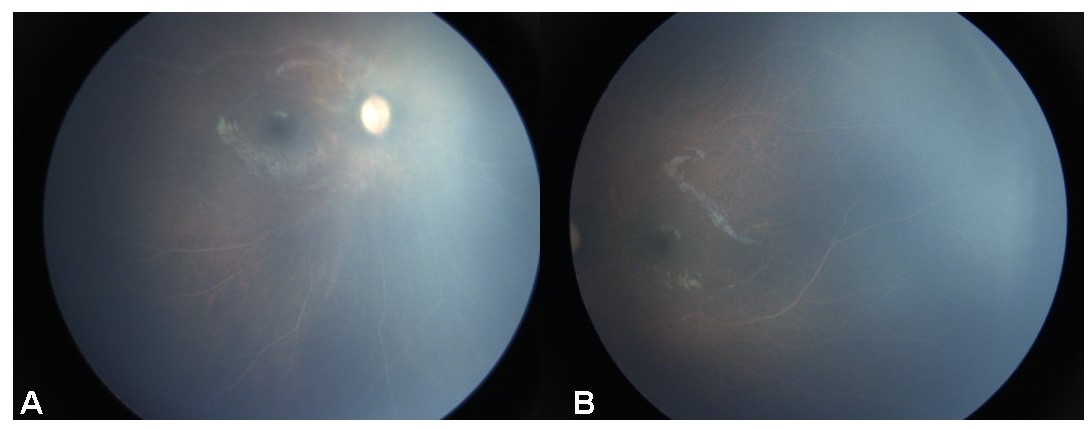
Figure 1 : Fundus photo of right eye ( Figure 1, A ) and left eye ( Figure 2, B ) of a 15 month old male child showing whitish creamy retinal vessels suggestive of lipemia retinalis. The child was born at 32 weeks and had a birth weight of 1100 grams. The child was referred by the paediatrician for screening of retinopathy of prematurity. However, the parents delayed the presentation of the child to the ophthalmologist. The parents were counselled in the ophthalmology clinic about the need of laboratory evaluation of lipid profile and the child was referred back to the paediatrician. Contributed by Dr. Chitaranjan Mishra, DNB, FICO, MRCS Ed ( Ophthal ), Aravind Eye Hospital, Madurai, Tamil Nadu, India, 625020.
References
Zahavi A, Snir M, Kella YR. Lipemia retinalis: case report and review of the literature. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2013 Feb:17(1):110-1. doi: 10.1016/j.jaapos.2012.10.010. Epub 2013 Jan 18 [PubMed PMID: 23337350]
Level 3 (low-level) evidenceHeyl AG, Intra-Ocular Lipæmia. Transactions of the American Ophthalmological Society. 1880; [PubMed PMID: 25258848]
Vinger PF, Sachs BA. Ocular manifestations of hyperlipoproteinemia. American journal of ophthalmology. 1970 Oct:70(4):563-73 [PubMed PMID: 5505473]
Rayner S, Lee N, Leslie D, Thompson G. Lipaemia retinalis: a question of chylomicrons? Eye (London, England). 1996:10 ( Pt 5)():603-8 [PubMed PMID: 8977790]
Level 3 (low-level) evidenceTripathy K, Patel BC. Purtscher Retinopathy. StatPearls. 2024 Jan:(): [PubMed PMID: 31194324]
Uysal E, Acar YA, Gökmen E, Kutur A, Doğan H. Hypertriglyceridemia induced pancreatitis (chylomicronemia syndrome) treated with supportive care. Case reports in critical care. 2014:2014():767831. doi: 10.1155/2014/767831. Epub 2014 Nov 23 [PubMed PMID: 25506434]
Level 3 (low-level) evidenceBrunzell JD, Bierman EL. Chylomicronemia syndrome. Interaction of genetic and acquired hypertriglyceridemia. The Medical clinics of North America. 1982 Mar:66(2):455-68 [PubMed PMID: 7040847]
Gehrisch S. Common mutations of the lipoprotein lipase gene and their clinical significance. Current atherosclerosis reports. 1999 Jul:1(1):70-8 [PubMed PMID: 11122694]
Leaf DA. Chylomicronemia and the chylomicronemia syndrome: a practical approach to management. The American journal of medicine. 2008 Jan:121(1):10-2. doi: 10.1016/j.amjmed.2007.10.004. Epub [PubMed PMID: 18187065]
Cypel M, Manzano R, Dos Reis FA, Ishida N, Ayhara T. Lipemia retinalis in a 35-day-old infant with hyperlipoproteinemia: case report. Arquivos brasileiros de oftalmologia. 2008 Mar-Apr:71(2):254-6 [PubMed PMID: 18516428]
Level 3 (low-level) evidenceSriram CS, Gulati S, Chopra V, Vashist S, Menon PS. Familial combined hyperlipidemia in a North Indian kindred. Indian journal of pediatrics. 2005 Nov:72(11):987-9 [PubMed PMID: 16391457]
Level 3 (low-level) evidenceChristian JB, Bourgeois N, Snipes R, Lowe KA. Prevalence of severe (500 to 2,000 mg/dl) hypertriglyceridemia in United States adults. The American journal of cardiology. 2011 Mar 15:107(6):891-7. doi: 10.1016/j.amjcard.2010.11.008. Epub 2011 Jan 19 [PubMed PMID: 21247544]
Horton M, Thompson K. Lipemia retinalis preceding acute pancreatitis. Optometry (St. Louis, Mo.). 2011 Aug:82(8):475-80. doi: 10.1016/j.optm.2011.01.011. Epub 2011 May 12 [PubMed PMID: 21570360]
Level 3 (low-level) evidenceNagra PK, Ho AC, Dugan JD Jr. Lipemia retinalis associated with branch retinal vein occlusion. American journal of ophthalmology. 2003 Apr:135(4):539-42 [PubMed PMID: 12654375]
Level 3 (low-level) evidenceÖzturk BT, Bozkurt B, Meşen A, Gonul S, İpekci SH. Spectral-Domain Optical Coherence Tomography Findings in Lipemia Retinalis. Ophthalmic surgery, lasers & imaging retina. 2016 Jun 1:47(6):589-92. doi: 10.3928/23258160-20160601-13. Epub [PubMed PMID: 27327291]
Jain A, Mochi TB, Braganza SD, Agrawal S, Shetty BK, Pachiyappan B. Lipemia retinalis in an infant treated for retinopathy of prematurity. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2017 Jun:21(3):254-257. doi: 10.1016/j.jaapos.2017.05.021. Epub 2017 May 27 [PubMed PMID: 28558973]
Shinkre ND, Usgaonkar UPS. Lipemia retinalis in a 27 day old neonate: A case report. Indian journal of ophthalmology. 2019 Jun:67(6):954-957. doi: 10.4103/ijo.IJO_1310_18. Epub [PubMed PMID: 31124530]
Level 3 (low-level) evidenceSamanta R, Katoch D. Lipemia retinalis in an infant. Indian journal of ophthalmology. 2019 Jun:67(6):953. doi: 10.4103/ijo.IJO_225_19. Epub [PubMed PMID: 31124529]
Parker F, Bagdade JD, Odland GF, Bierman EL. Evidence for the chylomicron origin of lipids accumulating in diabetic eruptive xanthomas: a correlative lipid biochemical, histochemical, and electron microscopic study. The Journal of clinical investigation. 1970 Dec:49(12):2172-87 [PubMed PMID: 5480845]
Gopal L, Sunder KS, Rao SK, Soni M, Sharma S, Ramakrishnan S. Hyperlipidemia in a poorly controlled diabetic presenting with lipemic aqueous and lipemia retinalis. Retina (Philadelphia, Pa.). 2004 Apr:24(2):312-5 [PubMed PMID: 15097900]
Level 3 (low-level) evidenceWilson WS, Lee JH. Letter: Retinal xanthoma. Lancet (London, England). 1974 Jan 5:1(7845):34 [PubMed PMID: 4129022]
Level 3 (low-level) evidenceJain S, Goyal A, Kumar V. Lipaemia retinalis in familial chylomicronaemia syndrome. Lancet (London, England). 2018 Aug 25:392(10148):e7. doi: 10.1016/S0140-6736(18)31796-3. Epub [PubMed PMID: 30152345]
Fu V, Scanga HL, Medsinge A, Nischal KK. Improved visual function with dietary intervention in a child with lipemia retinalis. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2014 Oct:18(5):488-90. doi: 10.1016/j.jaapos.2014.05.004. Epub 2014 Oct 21 [PubMed PMID: 25439305]
Level 3 (low-level) evidenceYin HY, Warman R, Suh EH, Cheng AM. Exceptionally elevated triglyceride in severe lipemia retinalis. International medical case reports journal. 2016:9():333-336 [PubMed PMID: 27799830]
Level 3 (low-level) evidenceStalenhoef AF, de Graaf J, Wittekoek ME, Bredie SJ, Demacker PN, Kastelein JJ. The effect of concentrated n-3 fatty acids versus gemfibrozil on plasma lipoproteins, low density lipoprotein heterogeneity and oxidizability in patients with hypertriglyceridemia. Atherosclerosis. 2000 Nov:153(1):129-38 [PubMed PMID: 11058707]
Level 1 (high-level) evidenceChapman MJ. Fibrates in 2003: therapeutic action in atherogenic dyslipidaemia and future perspectives. Atherosclerosis. 2003 Nov:171(1):1-13 [PubMed PMID: 14642400]
Level 3 (low-level) evidenceHarris WS, Pottala JV, Thiselton DL, A Varvel S, Baedke AM, Dayspring TD, Warnick GR, McConnell JP. Does APOE genotype modify the relations between serum lipid and erythrocyte omega-3 fatty acid levels? Journal of cardiovascular translational research. 2014 Jul:7(5):526-32. doi: 10.1007/s12265-014-9554-8. Epub 2014 Mar 5 [PubMed PMID: 24595593]
Level 2 (mid-level) evidenceMcKenney J. New perspectives on the use of niacin in the treatment of lipid disorders. Archives of internal medicine. 2004 Apr 12:164(7):697-705 [PubMed PMID: 15078639]
Level 3 (low-level) evidenceCapitena CE, Wagoner HJ, Ruzas CM, Bennett TD, Baker PR 2nd, Jung JL, Weisfeld-Adams JD. Rapid resolution of infantile lipemia retinalis following exchange transfusion. Journal of inherited metabolic disease. 2016 Nov:39(6):889-890 [PubMed PMID: 27518769]
Schaap-Fogler M, Schurr D, Schaap T, Leitersdorf E, Rund D. Long-term plasma exchange for severe refractory hypertriglyceridemia: a decade of experience demonstrates safety and efficacy. Journal of clinical apheresis. 2009:24(6):254-8. doi: 10.1002/jca.20224. Epub [PubMed PMID: 19927362]
Patel DV, Snead MP, Satchi K. Retinal arteriolar calcification in a patient with chronic renal failure. The British journal of ophthalmology. 2002 Sep:86(9):1063 [PubMed PMID: 12185140]
Level 3 (low-level) evidence