Introduction
Giant cell arteritis, formerly known as temporal arteritis, is an inflammatory vasculopathy that affects medium- and large-sized arteries, with a predilection for the branches of the carotid artery. The disease process is not limited to the temporal artery. Symptoms of giant cell arteritis include temporal headaches and tenderness, scalp pain, jaw claudication, and visual changes that may ultimately result in blindness. Giant cell arteritis is frequently associated with polymyalgia rheumatica.
Giant cell arteritis is a granulomatous arteritis with mononuclear cell infiltrates and giant cell formation within the vessel wall. In biopsy specimens of the superficial temporal artery, this histologic finding is pathognomonic for giant cell arteritis.[1][2][3][4]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Understanding the anatomy of the superficial temporal fascia, superficial temporal artery, temporal branch of the facial nerve, and the safe and dangerous zones occupied by these structures is crucial to perform a temporal artery biopsy safely.
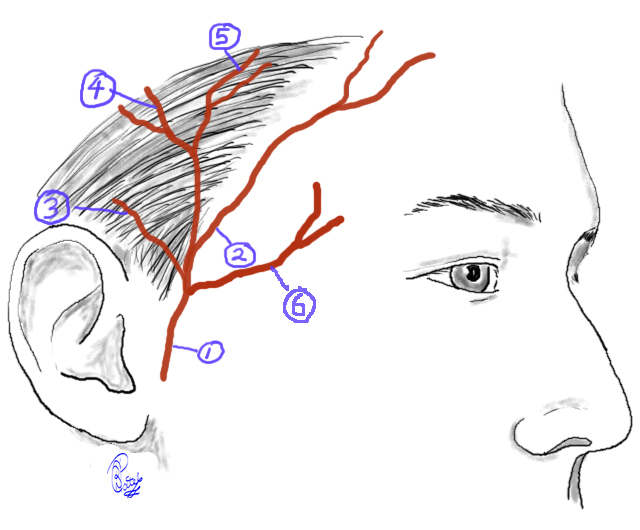
Superficial Temporal Artery (Figures 1 & 2)
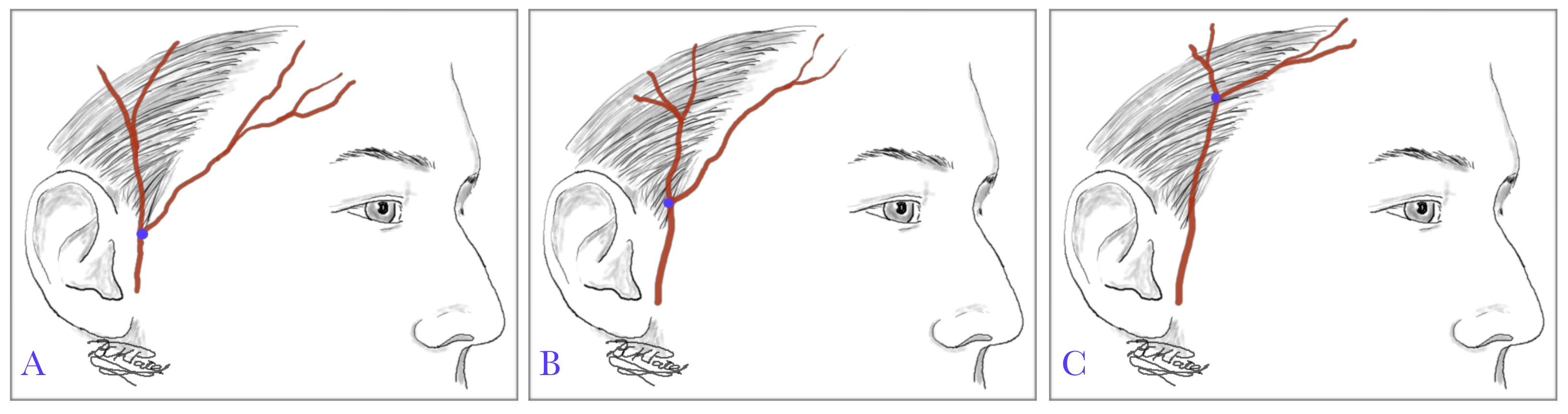
The superficial temporal artery, one of the terminal branches of the external carotid artery, arises within the parotid gland. The superficial temporal artery courses superiorly in front of the tragus, immediately giving off an anterior branch, the middle temporal artery. The anterior auricular branch courses posteriorly and arises at the superior root of the helix; it then divides into the frontal and parietal branches, each of which has multiple secondary branches. The bifurcation of the anterior auricular artery into the frontal and parietal branches is anomalous; it is high in 73% of patients, intermediate or just below the apex of the helix in 20%, and low or just above the tragus in another 7%. This anomaly is of clinical importance as the risk of injury to the temporal branch of the facial nerve is higher in patients with a low bifurcation; the artery is closer to the nerve.
Relationship of the Superficial Temporal Artery to the Temporal Facial Nerve (Figures 3 & 4)
The superficial temporal fascia, also known as the temporoparietal fascia, lies just deep to the subcutaneous adipose tissue of the scalp. This fascia is contiguous with the superficial musculoaponeurotic system (SMAS) of the face inferiorly and the occipitofrontalis-galea aponeurotica complex superiorly. Coursing through the superficial temporal fascia, the superficial temporal artery travels cephalad within the preauricular cheek before bifurcating into the frontal and parietal branches. The temporal branch of the facial nerve exits the parotid gland, travels over the middle third of the zygoma, then within the superficial temporal fascia in the temple region to reach the frontalis, corrugator supercilii, procerus, and orbicularis oculi muscles, which it innervates. Its course is approximated by the Pitanguy line, which runs from 0.5 cm inferior to the tragus to 1.5 cm superior to the lateral brow.[5] The distal rami of the temporal branch of the facial nerve always travel deep to the muscles they innervate. The superficial temporal artery lies within the superficial temporal fascia, while the temporal branch of the facial nerve runs slightly deeper but also within or on the deep surface of this tissue.
Safe Zone (Video 1)
The anterior temporal hairline is lateral to the frontalis muscle; therefore, dissecting superior or posterior to the anterior hairline during a temporal artery biopsy is unlikely to injure the temporal branch of the facial nerve. However, because there are no muscles of facial expression in the temple region, only the thin superficial temporal fascia, the temporal branch of the facial nerve is particularly susceptible to injury over the zygoma and within the temple region.
Some authors define the danger zone for the temporal branch of the facial nerve by outlining a region bounded inferiorly by a line from the earlobe to the lateral eyebrow and superiorly by a line from the intertragal notch or earlobe to the lateral edge of the highest forehead crease. Other authors define up to 1.5 cm posterior to the lateral orbital rim and up to 1 cm anterior to the attachment of the helix along the level of the zygoma as safe zones to avoid nerve injury.[6][7][8][9] See the video for an example of how to mark the safe zone preoperatively, based on cadaver studies by Shin et al.[10]
Biopsy Site
Some authors recommend obtaining the biopsy specimen from the trunk of the superficial temporal artery, proximal to the division into frontal and parietal branches.[11] Others feel that this technique sacrifices an unacceptably large arterial zone. Branches of the superficial temporal artery are useful for perfusing local and regional craniofacial reconstruction flaps and transferring free flaps to repair large facial defects. For this reason, it may be more prudent to limit the extent of superficial temporal artery sacrifice to an anterior branch.
Other surgeons have suggested performing the biopsy on the parietal branch of the superficial temporal artery to eliminate the chance of injury to the temporal branch of the facial nerve.[12] The parietal branch of the artery travels subperiosteally after separating from the main trunk of the superficial temporal artery. The sensitivity and specificity of parietal branch specimens are not known. However, the parietal branch of the superficial temporal artery provides collateral circulation to the brain, which may warrant preservation.
Indications
Patients with giant cell arteritis may develop acute visual disturbances, including temporary or permanent blindness; prompt diagnosis is warranted. While several clinical changes such as head or neck pain, jaw or tongue claudication, polymyalgia, temple tenderness on palpation, and elevated serum inflammatory markers may suggest the diagnosis, no single sign or symptom demonstrates a sensitivity or specificity that approaches temporal artery biopsy (TAB).
Given its greater than 90% positive predictive value, TAB is the gold standard test for diagnosing giant cell arteritis and should be considered in anyone with suspicion of the disease. It is important to note that treatment with systemic corticosteroids should not be delayed until after TAB, as up to 10 days of steroid therapy does not significantly reduce the sensitivity of the biopsy, and early steroid administration reduces morbidity.[13]
The clinician should have a high suspicion of giant cell arteritis in any patient aged 50 years or older with elevated inflammatory markers (C-reactive protein ≥25 mg/L or erythrocyte sedimentation rate ≥50 mm/h) and 1 of the following clinical findings:
- New or atypical headache
- New visual changes
- Jaw or tongue claudication
Contraindications
Relative contraindications to temporal artery biopsy (TAB) are few.
Authors disagree on the value of performing a biopsy after prolonged corticosteroid therapy. Some reports indicate that corticosteroid therapy does not significantly affect the sensitivity of the biopsy. In contrast, others claim that 2 to 4 weeks of therapy may substantially affect biopsy results.[14][15][16]
A prior TAB performed correctly and yielded a negative result for giant cell arteritis may be a contraindication to a contralateral TAB; in this circumstance, the contralateral TAB is positive in only 2% to 3% of patients.[17]
Equipment
The required equipment for a temporal artery biopsy includes the following:
- Nonsterile preparation stand
- Doppler ultrasound and water-based lubricating gel
- Marking pen
- 4 x 4 gauze
- Liposomal 4% lidocaine cream
- Lidocaine 1% with 1:200,000 epinephrine
- Bupivacaine 0.5% with 1:200,000 epinephrine
- Hypodermic needle, 18-gauge
- Hypodermic needle, 27-gauge (1 1/4 inch)
- Syringe, 10 mL, with 3-ring control
- Electric hair clipper
- Specimen container with formalin
- Benzalkonium chloride
- Sterile Mayo stand
- Scalpel, No. 15 blade
- Single skin hook
- Adson-Brown forceps
- Bishop-Harmon forceps
- Tenotomy scissors
- Metzenbaum scissors
- Suture scissors
- Frazier suction tip, 10 French
- Hemostat clamps
- Castroviejo needle holder
- Webster needle holder
- Weitlaner self-retaining retractors, small
- Ruler
- Towel clamps
- Monopoar or bipolar cautery
- 4-0 or 5-0 polyglactin 910 suture
- 5-0 poliglecaprone suture
- 5-0 fast-absorbing gut suture
- 3-0 silk ties
- Dressing:
- Petrolatum ointment
- Silk tape
- Cotton gauze roll
Personnel
A temporal artery biopsy is performed by a surgeon trained and proficient with the procedure. This is typically an ophthalmologist accompanied by a nurse for intraoperative assistance and post-procedure monitoring.
Preparation
Appropriate biopsy site selection is critical to confirm the diagnosis of giant cell arteritis. Clinical symptoms such as visual disturbances, headache, or a painful vessel assist the surgeon in selecting laterality for the temporal artery biopsy, even though the physical examination poorly correlates with biopsy results.
After choosing which temporal artery to biopsy, Doppler ultrasound is employed to identify a peripheral segment of the frontal branch of the temporal artery in the anatomic safe zone. This branch is often located just posterior to the anterior hairline, a location that facilitates cosmesis and scar camouflage.
The patient is placed in a reclined position. The surgeon makes two marks: at least a 5-centimeter length of the artery and a 3- to 4-centimeter incision. This length of the artery is necessary due to the potential for segmental manifestations of the underlying disease process. (Video 2)
Technique or Treatment
Trim the hair as necessary and scrub and drape the skin in the normal fashion. Anesthetize the intended area with 5 to 10 mL of lidocaine with epinephrine; extend the area to 1 cm lateral to the artery on either side. Using the No. 15 scalpel blade, incise the dermis directly over the artery such that the thin subcutaneous tissue is barely visible. Separate the edges of the incision using blunt-tipped dissecting scissors and skin hooks; dissect to uncover the superficial temporal fascia. Grasp this fascia with forceps a few millimeters lateral to the artery. Incise the fascia sharply with scissors and enlarge the fascial incision to expose the artery. Palpation of the arterial pulse may facilitate identifying the vessel.
Gently harvest approximately 5 centimeters of the vessel. Use suture or indirect electrocoagulation via forceps to ligate any small branches of the temporal artery prior to transection; this promotes a relatively bloodless surgical field. Ligate the proximal and distal portions of the main vessel using 4-0 or 5-0 polyglactin 910 suture, transect the vessel, and place the specimen in formalin. Apply electrocoagulation to the vessel ends in situ. Ensure that hemostasis is achieved. Approximate the skin edges with 5-0 poliglecaprone subcutaneous sutures, and complete the closure with either a cyanoacrylate skin adhesive or 6-0 gut sutures. (Video 2)
Surgical Tips
- Consider marking the safe zone before the procedure, as shown in the video.
- Avoid sharp dissection under the superficial temporal fascia; blunt dissection is preferred.
- After dissecting through the superficial temporal fascia to identify the temporal artery, avoid additional deeper or blind dissection.
- Once the artery is identified, identify any nerve branches in the area, as the temporal facial nerve may be very close to the temporal artery in some patients, even when the safe zones are marked.
- Plan to biopsy the frontal branch of the superficial temporal artery rather than the main trunk or the parietal branch.
- Gentle handling of the temporal artery before ligation and harvesting can be accomplished using muscle hooks.
Complications
A significant challenge facing the pathologist interpreting the TAB is the potential for false-negative results, which may occur in 5% to 10% of cases. Therefore, the surgeon must perform the TAB employing appropriate biopsy site selection, meticulous tissue handling, and adequate specimen length to maximize diagnostic yield. Unfortunately, despite the correct technique, false-negative results remain common. In some cases, bilateral TAB may increase the yield and decrease the false-negative rates.
The most dreaded complication of TAB is temporary or permanent damage to the temporal branch of the facial nerve.[18] Techniques to reduce the risk of nerve injury include ultrasonographic localization of the artery, placement of incisions directly superficial to the artery to protect the potentially deeper running nerve, and blunt dissection only within or above the superficial temporal fascia. A 2009 study found that 1.25% of TAB specimens contained a portion of the temporal facial nerve, and a 2012 study found that 4% of patients undergoing TAB had frontalis dysfunction with no improvement at 6 months.[19][20]
Other than common surgical complications such as bleeding, infection, hematoma, and wound dehiscence, possible, albeit rare, complications of TAB include ischemic stroke and scalp or tongue necrosis, which have been reported.[21] Some authors recommend palpating and firmly holding a bounding temporal artery pulse for several minutes before proceeding with TAB or locating a major arterial branch other than that being biopsied via ultrasound to ensure collateral vascular supply and minimize the risk of subsequent stroke.
Clinical Significance
The gold standard for diagnosing giant cell arteritis is a temporal artery biopsy. Due to a relatively low negative predictive value, however, a negative biopsy result does not definitively rule out the diagnosis. Currently, patients are considered to have the diagnosis of temporal arteritis if three of the following five clinical features are present:[22]
- Age ≥50 years at the onset of symptoms
- New headache
- Temporal artery abnormalities, such as tenderness of the superficial artery or decreased palpability of its pulse
- ESR ≥50 mm/hr
- Abnormal TAB, demonstrating vasculitis, a predominance of mononuclear cell infiltration or granulomatous inflammation, or multinucleated giant cells
Enhancing Healthcare Team Outcomes
Patients with the signs and symptoms of giant cell arteritis rarely initially present to a surgeon trained to perform temporal artery biopsies. The referring healthcare professional needs to communicate the indications for the procedure to the surgeon, including when any corticosteroid therapy was initiated; corticosteroid therapy may be a contraindication to the procedure. Pathologists should communicate the interpretive results of the biopsy to the surgeon of record, the referring healthcare practitioner, and the primary care practitioner to facilitate proper treatment.
Patients should be informed that temporal artery biopsy is a diagnostic procedure only, as they sometimes believe it will improve or cure their underlying condition. The patient must be informed to continue any initiated oral corticosteroid therapy until the biopsy results are finalized and communicated to the interprofessional team.
Nursing, Allied Health, and Interprofessional Team Interventions
The nursing staff is essential for educating the patient about possible complications and warning signs of severe adverse reactions. Proper guidance makes the patient more likely to report developing complications early and prevent severe morbidity. The nursing staff also assists the surgeon during the procedure and monitors the patient for immediate complications. It is essential for nurses practicing in the field of head and facial surgery to familiarize themselves with the possible complications of this procedure and to assess the neurologic status of patients undergoing TAB to identify adverse outcomes if they occur.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
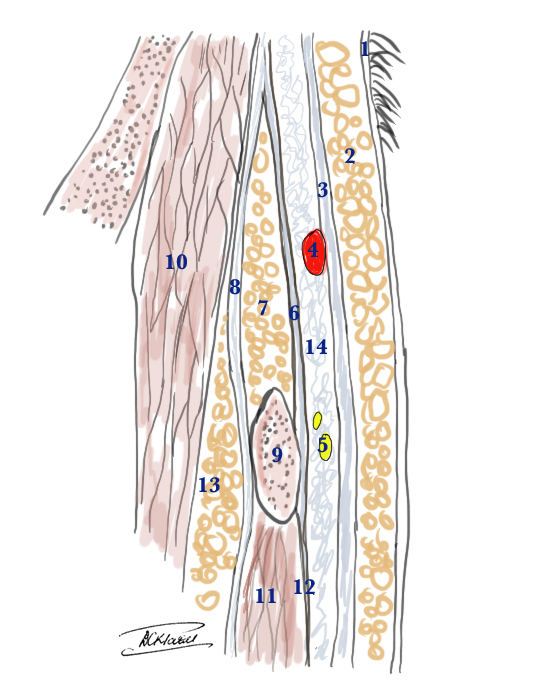
Superficial Temporal Artery and the Temporal branch of the Facial Nerve: anatomical cross section to show the relative layers above the zygomatic arch 1. Skin 2. Subcutaneous fat 3. Superficial temporal fascia (also called temporoparietal fascia) 4. Temporal artery within the superficial temporal fascia 5. Temporal branch of the facial nerve is just a little deeper than the artery below the superficial temporal fascia 6. Superficial layer of deep temporal fascia 7. Superficial temporal fat pad 8. Deep layer of deep temporal fascia 9. Zygomatic arch 10. Temporalis muscle 11. Masseter muscle 12. Masceteric fascia Contributed by Prof. Bhupendra C. K. Patel MD, FRCS
(Click Video to Play)
(Click Video to Play)
References
Croci S, Bonacini M, Muratore F, Caruso A, Fontana A, Boiardi L, Soriano A, Cavazza A, Cimino L, Belloni L, Perry O, Fridkin M, Parmeggiani M, Blank M, Shoenfeld Y, Salvarani C. The therapeutic potential of tuftsin-phosphorylcholine in giant cell arteritis. Journal of autoimmunity. 2019 Mar:98():113-121. doi: 10.1016/j.jaut.2019.01.002. Epub 2019 Jan 10 [PubMed PMID: 30638709]
Gokoffski KK, Chatterjee A, Khaderi SK. Seasonal incidence of biopsy-proven giant cell arteritis: a 20-year retrospective study of the University of California Davis Medical System. Clinical and experimental rheumatology. 2019 Mar-Apr:37 Suppl 117(2):90-97 [PubMed PMID: 30620274]
Level 2 (mid-level) evidencede Miguel E, Monjo I. Response to: A Comparative Study of Doppler Ultrasound Against Temporal Artery Biopsy in the Diagnosis of Giant Cell Arteritis. Reumatologia clinica. 2020 Nov-Dec:16(6):510-511. doi: 10.1016/j.reuma.2018.11.001. Epub 2018 Dec 23 [PubMed PMID: 30587463]
Level 2 (mid-level) evidenceMacchioni P, Boiardi L, Muratore F, Restuccia G, Cavazza A, Pipitone N, Catanoso M, Mancuso P, Luberto F, Giorgi Rossi P, Salvarani C. Survival predictors in biopsy-proven giant cell arteritis: a northern Italian population-based study. Rheumatology (Oxford, England). 2019 Apr 1:58(4):609-616. doi: 10.1093/rheumatology/key325. Epub [PubMed PMID: 30517710]
Pitanguy I, Ramos AS. The frontal branch of the facial nerve: the importance of its variations in face lifting. Plastic and reconstructive surgery. 1966 Oct:38(4):352-6 [PubMed PMID: 5926990]
Conway R, Smyth AE, Kavanagh RG, O'Donohoe RL, Purcell Y, Heffernan EJ, Molloy ES, McNeill G, Killeen RP. Diagnostic Utility of Computed Tomographic Angiography in Giant-Cell Arteritis. Stroke. 2018 Sep:49(9):2233-2236. doi: 10.1161/STROKEAHA.118.021995. Epub [PubMed PMID: 30354972]
Ing EB, Ing R. The Use of a Nomogram to Visually Interpret a Logistic Regression Prediction Model for Giant Cell Arteritis. Neuro-ophthalmology (Aeolus Press). 2018 Oct:42(5):284-286. doi: 10.1080/01658107.2018.1425728. Epub 2018 Feb 5 [PubMed PMID: 30258473]
Braun J, Baraliakos X, Fruth M. The role of 18F-FDG positron emission tomography for the diagnosis of vasculitides. Clinical and experimental rheumatology. 2018 Sep-Oct:36 Suppl 114(5):108-114 [PubMed PMID: 30296989]
Sammel AM, Fraser CL. Update on giant cell arteritis. Current opinion in ophthalmology. 2018 Nov:29(6):520-527. doi: 10.1097/ICU.0000000000000528. Epub [PubMed PMID: 30138144]
Level 3 (low-level) evidenceShin KJ, Shin HJ, Lee SH, Koh KS, Song WC. Surgical anatomy of the superficial temporal artery to prevent facial nerve injury during arterial biopsy. Clinical anatomy (New York, N.Y.). 2018 May:31(4):608-613. doi: 10.1002/ca.23033. Epub 2017 Dec 21 [PubMed PMID: 29226469]
Cahais J, Houdart R, Lupinacci RM, Valverde A. Operative technique: Superficial temporal artery biopsy. Journal of visceral surgery. 2017 Jun:154(3):203-207. doi: 10.1016/j.jviscsurg.2017.05.001. Epub 2017 Jun 7 [PubMed PMID: 28601496]
Yoon MK, Horton JC, McCulley TJ. Facial nerve injury: a complication of superficial temporal artery biopsy. American journal of ophthalmology. 2011 Aug:152(2):251-255.e1. doi: 10.1016/j.ajo.2011.02.003. Epub 2011 Jun 17 [PubMed PMID: 21683331]
Level 3 (low-level) evidenceHassan N, Dasgupta B, Barraclough K. Giant cell arteritis. BMJ (Clinical research ed.). 2011 May 23:342():d3019. doi: 10.1136/bmj.d3019. Epub 2011 May 23 [PubMed PMID: 21606138]
Ray-Chaudhuri N, Kiné DA, Tijani SO, Parums DV, Cartlidge N, Strong NP, Dayan MR. Effect of prior steroid treatment on temporal artery biopsy findings in giant cell arteritis. The British journal of ophthalmology. 2002 May:86(5):530-2 [PubMed PMID: 11973248]
Level 1 (high-level) evidenceNarváez J, Bernad B, Roig-Vilaseca D, García-Gómez C, Gómez-Vaquero C, Juanola X, Rodriguez-Moreno J, Nolla JM, Valverde J. Influence of previous corticosteroid therapy on temporal artery biopsy yield in giant cell arteritis. Seminars in arthritis and rheumatism. 2007 Aug:37(1):13-9 [PubMed PMID: 17360027]
Level 2 (mid-level) evidencePapadakos SP, Papazoglou AS, Moysidis DV, Tsagkaris C, Papadakis DL, Koutsogianni A, Fragoulis G, Papadakis M. The Effect of Corticosteroids on Temporal Artery Biopsy Positivity in Giant Cell Arteritis: Timing is Everything. Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases. 2023 Jun 1:29(4):173-176. doi: 10.1097/RHU.0000000000001938. Epub 2023 Jan 9 [PubMed PMID: 36728371]
Boyev LR, Miller NR, Green WR. Efficacy of unilateral versus bilateral temporal artery biopsies for the diagnosis of giant cell arteritis. American journal of ophthalmology. 1999 Aug:128(2):211-5 [PubMed PMID: 10458178]
Level 2 (mid-level) evidenceHohman MH, Bhama PK, Hadlock TA. Epidemiology of iatrogenic facial nerve injury: a decade of experience. The Laryngoscope. 2014 Jan:124(1):260-5. doi: 10.1002/lary.24117. Epub 2013 Apr 18 [PubMed PMID: 23606475]
Level 2 (mid-level) evidenceGuffey Johnson J, Grossniklaus HE, Margo CE, Foulis P. Frequency of unintended vein and peripheral nerve biopsy with temporal artery biopsy. Archives of ophthalmology (Chicago, Ill. : 1960). 2009 May:127(5):703. doi: 10.1001/archophthalmol.2009.77. Epub [PubMed PMID: 19433728]
Murchison AP, Bilyk JR. Brow ptosis after temporal artery biopsy: incidence and associations. Ophthalmology. 2012 Dec:119(12):2637-42. doi: 10.1016/j.ophtha.2012.07.020. Epub 2012 Sep 15 [PubMed PMID: 22986114]
Schlezinger NS, Schatz NJ. Giant cell arteritis (temporal arteritis). Transactions of the American Neurological Association. 1971:96():12-5 [PubMed PMID: 5159067]
Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, Edworthy SM, Fauci AS, Leavitt RY, Lie JT. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis and rheumatism. 1990 Aug:33(8):1122-8 [PubMed PMID: 2202311]