Introduction
Lung capacity or total lung capacity (TLC) is the volume of air in the lungs upon the maximum effort of inspiration. Among healthy adults, the average lung capacity is about 6 liters. Age, gender, body composition, and ethnicity are factors affecting the different ranges of lung capacity among individuals. TLC rapid increases from birth to adolescence and plateaus at around 25 years old. Males tend to have a greater TLC than females, while individuals with tall stature tend to have greater TLC than those with short stature, and individuals with a high waist-to-hip ratio generally have a lower TLC.[1][2] Individuals of African descent have a lower TLC compared to individuals of European descent.[3] Additional factors that affect an individual's lung capacity include the level of physical activity, chest wall deformities, and respiratory diseases.
Clinicians can measure lung capacity by plethysmography, dilutional helium gas method, nitrogen gas washout method, or radiographically by a relatively new technique using by computed tomography (CT). Methodically, the TLC is calculated by measuring the lung capacities: inspiratory capacity (IC), functional residual capacity (FRC), and the vital capacity (VC). Illustrated in Figure 1, Panel A, the lung capacities can be further divided into the following lung volumes: tidal volume (TV), inspiratory reserve volume (IRV), expiratory reserve volume (ERV), and the residual volume (RV). This review article will not delve into definitions of all of the lung capacities and lung volumes but instead will outline the methods in which lung capacity is measured and discuss the clinical significance of TLC (see image).
Related Testing
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Related Testing
The volume of air that makes up the TLC can be calculated by directly measuring the lung volumes at different phases of the respiratory cycle and by measuring the remaining volume of air in the lungs after maximum exhalation. This relationship calculates as the total lung capacity equaling the sum of functional residual capacity and the inspiratory capacity or as the equation: TLC = FRC + IC. The FRC is only measurable by plethysmography, nitrogen gas washout, or helium gas dilution methods, or using computed tomography (CT). Once the FRC gas volume is measured and the RV is determined, the following additional equations that can be used to calculate the TLC; the sum of the four lung volumes: TLC = RV + ERV + IRV + TV or the sum of vital capacity and the residual volume: TLC = VC + RV.
Plethysmography
Plethysmography is used to measure the changes of pressure within a constant temperature and volume chamber. This test requires a patient to exercise various respiratory maneuvers inside of an air sealed chamber while breathing through a spirometer or a pneumotachograph. During the respiratory exercises, chest wall expansion and collapse cause changes in the pressure within the chamber and a transducer within the chamber measures these changes.[4] These pressure changes at various phases of the respiratory cycle are then analyzed to calculate the FRC when compared to the results of spirometry. The underlying principle to calculate the FRC by plethysmography has as its basis Boyle’s Law which states there is an inverse relationship between the volume and pressure of a gas when the temperature of that gas remains constant.[5] Boyle’s Law of gases equation: P1V1 = P2V2 is applied to plethysmography as initial pressure in the chamber multiplied by the initial volume in the chamber equals the pressure at the end of a chest expansion multiplied by the volume in the chamber at the end of chest expansion. Plethysmography is the gold standard and most accurate test for measuring lung volumes.[6] If using plethysmography on patients with obstructive lung disease, the TLC may be subject to overestimation.[5][6]
Helium Gas Dilution
The helium gas dilution method utilizes helium gas, a non-absorbable gas by the alveoli of the lungs, to measure the FRC lung volume in patients. This test begins by having a patient breathe a known volume and concentration of helium gas mixture from a spirometry chamber through a tube attached to the patient’s mouth. During this time, the helium concentration within the chamber then equalizes with the helium concentration in the lungs, and the test concludes when a change in gas concentrations is less than 0.02%.[5][7] The FRC is calculated by knowing that the concentration of helium gas at the initiation of the test will equal the same concentration of gas at the end of the test based on the law of conservation of mass.[8] The equation used to solve for FRC in helium gas dilution then states that the FRC of helium gas equals the known volume of gas used in the test multiplied by the difference of the initial fraction helium gas and the final fraction of helium gas at the end of the test. This result is then divided by the final fraction of helium gas at the end of the test or as described in this equation: FRC = V1(FHe1-FHe2) / FHe2.[5] Helium and nitrogen gas dilution methods may measure lower lung volumes or TLC in patients with airflow obstruction; this is because both of these tests are unable to measure poorly ventilated areas of the lung.[5][7]
Nitrogen Gas Washout
A nitrogen washout method is also a form of a gas dilutional technique used to measure the FRC to calculate the TLC by giving a patient 100% oxygen to remove nitrogen gas from the lungs. This test requires a patient to breathe through a mouthpiece that has two-one way valves, one valve that allows the patient to inhale 100% oxygen and a second valve that allows the patient to exhale breaths into a pneumotachograph that measures nitrogen gas concentration and the volume of exhaled air.[4] The test begins with clipping the nares of the patient shut, followed by tidal breaths for 1 minute; then the patient is given 100% oxygen gas delivery at end expiration. This test lasts for about 7 minutes as this is the estimated time for completion of nitrogen washout from the lungs or the test discontinues after the nitrogen gas concentration falls to less than 1.5%.[5] Nitrogen washout works because of the following two reasons: 1) Nitrogen gas makes up about 78% of the gases in our atmosphere, and very minimal amounts of nitrogen gas can diffuse across the alveoli of the lungs and dissolve into the blood 2) The volume of nitrogen gas washed out of the lungs equals the initial volume of nitrogen in the lungs. Thus the FRC can be calculated by solving for the difference of volume nitrogen washed out and nitrogen gas tissue excretion divided by the difference between initial and final nitrogen gas concentration or the equation: FRC nitrogen gas = (nitrogen gas washed out) - (nitrogen gas tissue excretion) / initial - final nitrogen gas lung concentration.[5] Nitrogen gas washout testing remains a more simple and easy test for patients who may have difficulties performing plethysmography. Patients with obstructive lung disease who undergo nitrogen gas washout have been found to have underestimation of lung volume measurements and TLC to [5][9]
Computed Tomography (CT)
Computed tomography scan of the thorax is a method that requires the use of radiological imaging to calculate lung volumes. This test requires a patient to hold their breath at full inhalation while lying supine in the process of receiving a CT scan of the chest.[10] After completion of the CT of the chest, the TLC is calculated by solving for the total sum of each image axial cross-sectional area multiplied by the thickness of the slice.[4][5] The use of CT for measuring lung volumes in patients with normal pulmonary function testing and restrictive lung disease (caused by chest wall defects, pulmonary defects, or pleural disease) were found to have similar FRC, RV, and TLC values when compared to lung volumes measured by plethysmography and for both helium and nitrogen dilution techniques.[10] In patients with obstructive lung disease, plethysmography and CT yield similar measurements of lung volumes, while gas dilution techniques with helium gas in obstructive lung disease underestimates lung volumes when compared to CT measurements.[10] The CT scan method for measuring lung volumes is not widely used in the clinical setting as this method remains expensive and exposes patients to unnecessary radiation.[9]
Spirometry
Spirometry is a common test used in the clinical setting for assessing pulmonary function and diagnosis of pulmonary diseases by measuring forced expiratory volume in one second (FEV1) and forced vital capacity (FVC). The use of spirometry alone is often misconstrued as a test used to calculate the TLC when in fact, this test can not measure the RV, the remaining volume of air in the lungs after maximum exhalation. Furthermore, to use spirometry to calculate the TLC, it should be combined with plethysmography, gas dilution, gas washout, or radiographic imaging to estimate the RV.
Clinical Significance
Indication for Lung Volume Testing
The clinical indication for measuring lung volumes/capacities is usually when a patient presents with abnormal spirometry FEV1/FVC ratios significant for either obstructive or restrictive lung disease. Clinicians will then order additional testing either plethysmography, dilutional gas study, or radiographic imaging to confirm the presences of disease.
Restrictive Lung Disease and Obstructive Lung Disease Effects on Lung Capacity
The American Thoracic Society/European Respiratory Society (ATS/ERS) defines a restrictive ventilatory defect as a reduced TLC below the 5th percentile of normal predicted value with a normal FEV1/VC ratio.[11] In patients with restrictive lung disease, the underlying pathophysiology associated with reduced TLC is a result of decreased lung compliance and decrease chest wall expansion. These patients cannot expand their lungs fully, resulting in reduce inhalation air volume. Due to loss of lung compliance, the TLC, FRC, and RV are reduced as seen in Figure 1 Panel C. Some restrictive lung disease include: pectus excavatum, kyphoscoliosis, myasthenia gravis, and amyotrophic lateral sclerosis. The ATS/ERS defines obstructive lung disease as a ventilatory defect with an unequal reduction of maximal airflow from the lung compared to the maximum volume of gas that can be removed from the lungs with a FEV1/VC ratio below the 5th percentile of the predicted value.[11][2] The underlying pathophysiology of obstructive lung diseases results from changes to the airway, lung parenchyma, and pulmonary vasculature resulting in hyperinflation and air trapping within the lungs and decreased air expelled from the lungs during exhalation. On lung volume testing the TLC and the RV is increased as seen in Figure 1 Panel C. Some obstructive lung disease include chronic obstructive pulmonary disease (COPD), chronic bronchitis, asthma, and emphysema. Infrequently, a patient may be diagnosed to have mixed obstructive-restrictive lung disease (MORLD). MORLD presents with a decreased TLC on lung volume testing and spirometry testing significant for airway obstruction.[2]
Obesity and Lung Capacity
Obesity is known to have many consequences on an individuals health and correlates to the causes of comorbidities among individuals in North America. Obesity is also a cause of reduced TLC on lung volume testing with characteristics of a restrictive lung disease pattern on pulmonary function testing.[9] Obesity-related reduce lung volumes is more prevalent among males when compared to females because of gender difference of central fat distribution central and peripheral fat distribution respectively.[12] The proposed mechanism is thought to be caused by the increased weight of adipose tissue on the chest wall causing decrease compliance and increase abdominal adipose tissue causes restriction of the expansion of the diaphragm during inhalation resulting in a decrease in TLC, ERV, and FRC.[13][14] Weight loss has been shown to reverse reduced lung volumes in morbidly obese patients and should be encouraged.[15]
Lung Capacity Used as Predictors of Health Outcomes
Patients with COPD and an inspiratory capacity/total lung capacity ratio (IC/TLC ratio) less than 25% are found to be at an increased risk for the following: the need for careful monitoring of treatment, frequent hospital admissions, and risk for both all-cause and respiratory mortality.[16][17] Studies continue to show a positive correlation associated with the risk of IC/TLC ratio of less than 25% but have not been yet recommended or applied to clinical practice in the management of patients with COPD.
With late progression of COPD, patients can develop hyperinflation of the lungs, a complication that results in shortness of breath with exertion or at rest. For patients with COPD, the residual volume/total lung capacity ratio (RV/TLC ratio) greater than 40% is a predictor of resting hyperinflation and an independent risk factor for all-cause mortality.[18]
Media
(Click Image to Enlarge)
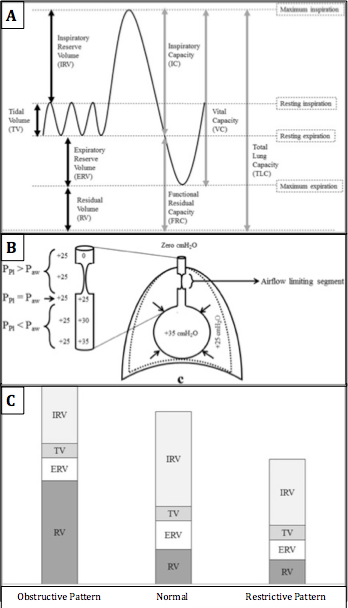
Residual Volume. Standard lung volumes and capacities (A), lung pressures at forceful expiration (B), and typical changes in lung volumes seen in restrictive and obstructive lung disease (C).
Contributed by Lutfi, 2017; Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/)
References
Stocks J, Quanjer PH. Reference values for residual volume, functional residual capacity and total lung capacity. ATS Workshop on Lung Volume Measurements. Official Statement of The European Respiratory Society. The European respiratory journal. 1995 Mar:8(3):492-506 [PubMed PMID: 7789503]
Level 1 (high-level) evidenceLutfi MF. The physiological basis and clinical significance of lung volume measurements. Multidisciplinary respiratory medicine. 2017:12():3. doi: 10.1186/s40248-017-0084-5. Epub 2017 Feb 9 [PubMed PMID: 28194273]
Rossiter CE, Weill H. Ethnic differences in lung function: evidence for proportional differences. International journal of epidemiology. 1974 Mar:3(1):55-61 [PubMed PMID: 4838716]
Wanger J, Clausen JL, Coates A, Pedersen OF, Brusasco V, Burgos F, Casaburi R, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Hankinson J, Jensen R, Johnson D, Macintyre N, McKay R, Miller MR, Navajas D, Pellegrino R, Viegi G. Standardisation of the measurement of lung volumes. The European respiratory journal. 2005 Sep:26(3):511-22 [PubMed PMID: 16135736]
Flesch JD, Dine CJ. Lung volumes: measurement, clinical use, and coding. Chest. 2012 Aug:142(2):506-510. doi: 10.1378/chest.11-2964. Epub [PubMed PMID: 22871760]
Coates AL, Peslin R, Rodenstein D, Stocks J. Measurement of lung volumes by plethysmography. The European respiratory journal. 1997 Jun:10(6):1415-27 [PubMed PMID: 9192953]
Brown R, Leith DE, Enright PL. Multiple breath helium dilution measurement of lung volumes in adults. The European respiratory journal. 1998 Jan:11(1):246-55 [PubMed PMID: 9543301]
Hopkins E, Sharma S. Physiology, Functional Residual Capacity. StatPearls. 2023 Jan:(): [PubMed PMID: 29763183]
Ruppel GL. What is the clinical value of lung volumes? Respiratory care. 2012 Jan:57(1):26-35; discussion 35-8. doi: 10.4187/respcare.01374. Epub [PubMed PMID: 22222123]
Tantucci C, Bottone D, Borghesi A, Guerini M, Quadri F, Pini L. Methods for Measuring Lung Volumes: Is There a Better One? Respiration; international review of thoracic diseases. 2016:91(4):273-80. doi: 10.1159/000444418. Epub 2016 Mar 17 [PubMed PMID: 26982496]
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CP, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre N, McKay R, Miller MR, Navajas D, Pedersen OF, Wanger J. Interpretative strategies for lung function tests. The European respiratory journal. 2005 Nov:26(5):948-68 [PubMed PMID: 16264058]
Maiolo C, Mohamed EI, Carbonelli MG. Body composition and respiratory function. Acta diabetologica. 2003 Oct:40 Suppl 1():S32-8 [PubMed PMID: 14618430]
Sue DY. Obesity and pulmonary function: more or less? Chest. 1997 Apr:111(4):844-5 [PubMed PMID: 9106556]
Jones RL, Nzekwu MM. The effects of body mass index on lung volumes. Chest. 2006 Sep:130(3):827-33 [PubMed PMID: 16963682]
Level 2 (mid-level) evidenceThomas PS, Cowen ER, Hulands G, Milledge JS. Respiratory function in the morbidly obese before and after weight loss. Thorax. 1989 May:44(5):382-6 [PubMed PMID: 2503905]
Cardoso J, Coelho R, Rocha C, Coelho C, Semedo L, Bugalho Almeida A. Prediction of severe exacerbations and mortality in COPD: the role of exacerbation history and inspiratory capacity/total lung capacity ratio. International journal of chronic obstructive pulmonary disease. 2018:13():1105-1113. doi: 10.2147/COPD.S155848. Epub 2018 Apr 5 [PubMed PMID: 29670346]
Zaman M, Mahmood S, Altayeh A. Low inspiratory capacity to total lung capacity ratio is a risk factor for chronic obstructive pulmonary disease exacerbation. The American journal of the medical sciences. 2010 May:339(5):411-4. doi: 10.1097/MAJ.0b013e3181d6578c. Epub [PubMed PMID: 20375693]
Level 2 (mid-level) evidenceShin TR, Oh YM, Park JH, Lee KS, Oh S, Kang DR, Sheen S, Seo JB, Yoo KH, Lee JH, Kim TH, Lim SY, Yoon HI, Rhee CK, Choe KH, Lee JS, Lee SD. The Prognostic Value of Residual Volume/Total Lung Capacity in Patients with Chronic Obstructive Pulmonary Disease. Journal of Korean medical science. 2015 Oct:30(10):1459-65. doi: 10.3346/jkms.2015.30.10.1459. Epub 2015 Sep 12 [PubMed PMID: 26425043]