Introduction
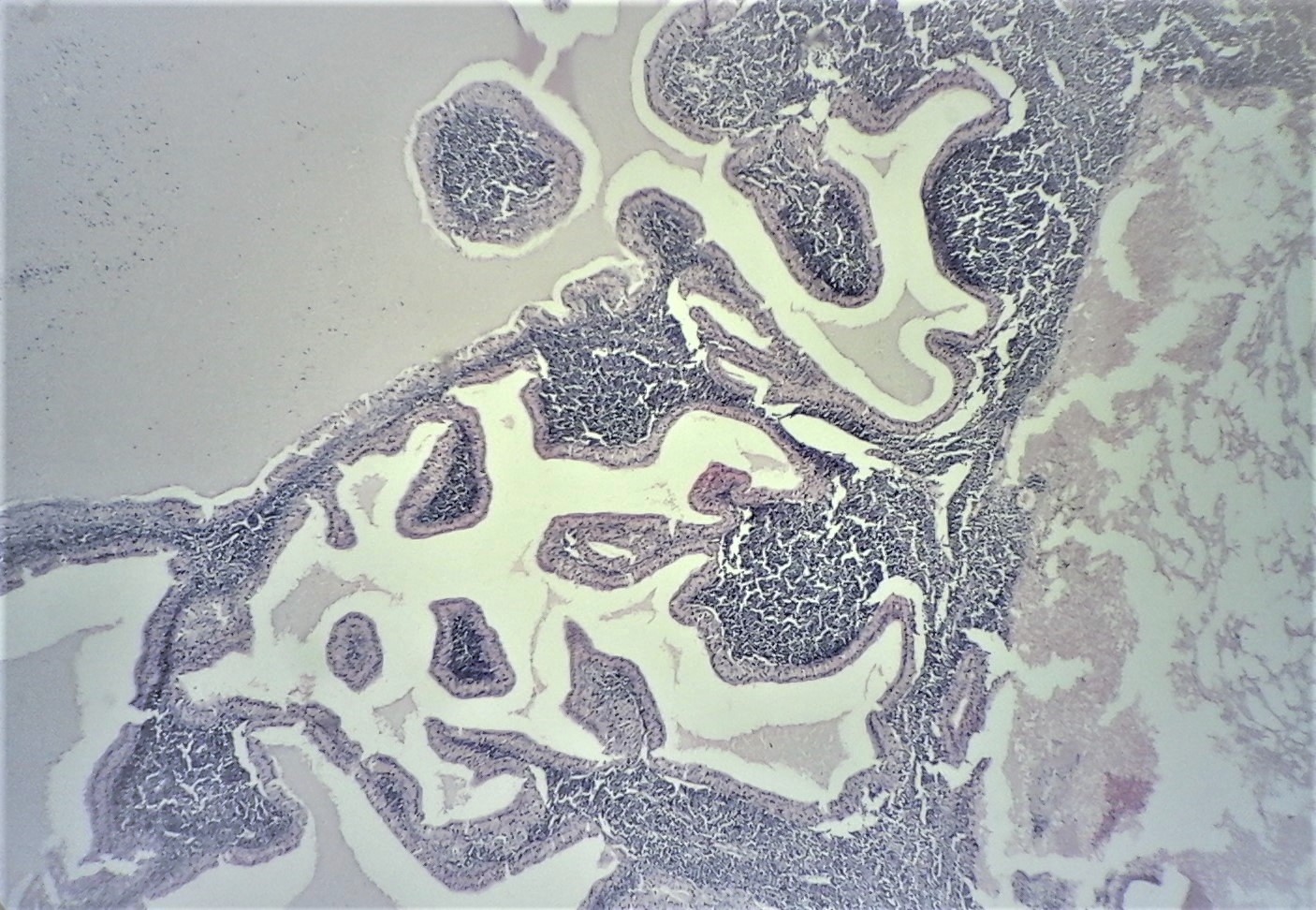
Initially described by Hildebrand in 1895, Warthin tumor (also known as cystadenolymphoma), is a benign and frequent salivary gland neoplasm. It represents about 2% to 15% of all primary epithelial tumors of the parotid gland. Extra-parotid Warthin tumor is very rare and may occur in the periparotid lymph node, nasopharynx, eyelid, and oral cavity. Warthin tumor is histologically characterized by a dense lymphoid stroma and a double layer of oncocytic epithelium with a papillary and cystic architectural pattern (see Image. Warthin Tumor, H&E ×40). Its etiology remains controversial.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of Warthin tumor has not yet been fully established. Some authors stipulated that this benign neoplasm arises as a result of some tumourigenic effect on epithelial inclusions located in the lymph nodes adjacent or the parotid gland.[2] Etiologic factors of Warthin tumor have been said to encompass Epstein Barr virus infection, tobacco, autoimmune disease, ionizing radiation, and chronic inflammation.[3][4][5] However, several questions remain regarding the male predominance in Warthin tumors and why tobacco should predominantly affect the parotid gland rather than the intraoral minor salivary glands.[3][6] Malignant transformation of Warthin tumor is extremely rare and accounts for 0.3% of the cases.[7]
Epidemiology
Warthin tumor is the most common ‘monomorphic’ adenoma of the major salivary glands. It accounts for about 2% to 15% of all parotid tumors.[8] It is the second most frequent benign neoplasm of the salivary glands after pleomorphic adenoma. Warthintumor occasionally occurs in young patients. In women, the peak incidence is in the 6th decade, whereas it is in the 7th decade in men. There is an apparent male predilection for the occurrence of Warthin tumor, although, with the recent reports, the difference in the sex ratio is declining.[9]
Pathophysiology
Warthin tumor is the only benign neoplasm of salivary glands associated with smoking.[10] The origin of this tumor is still debated despite the numerous theories concerning its histogenesis mentioned in the literature.[11][9] Numerous theories have been advocated, with each having different interpretations. Initially, Hildebrand proposed that the lesion may be remnants of the branchial pouches and a variant of the lateral cervical cyst. Later, Albrech and Artz proposed the heterotropic origin of Warthin tumor from the neoplastic proliferation of salivary gland ducts present within intra- or para-parotid nodes. This theory is widely accepted and was sustained by immunohistochemistry findings, which demonstrated that basal and luminal epithelial cells of Warthin tumor bear characteristics similar to those of the basal cells and striated duct cells of the excretory duct of the salivary gland.[9] Only a small subset of Warthin tumors present the t(11,19)(q21,p13) translocation and expression of the chimeric genes. These Warthin tumors are often classified as infarcted or metaplastic Warthin tumors.[12] Some authors suggested that the different histologic subtypes of Warthin tumor (epithelial predominance, mixed, lymphoid predominance) may result from staged pathogenetic development in which the lymphoid predominance subtype constitutes the early stage, followed by the mixed and the epithelial predominance subtypes.[13][14] This spectrum of modifications could be triggered by different and mostly unidentified pathogenetic factors, such as tobacco smoking, autoimmune disorders, or Epstein-Barr virus infection.[3] Interestingly, the latter was detected in very close association with multiple/bilateral Warthin tumors, in comparison with solitary Warthin tumors.[15]
Histopathology
Macroscopic Findings
Grossly, Warthin tumor is a well-circumscribed spherical to oval mass. On cut section, there are solid areas and multiple cysts with papillary projections (see Image. Warthin Tumor). The cystic spaces often contain mucoid creamy brown or white fluid.[16]
Cytology
Smears characteristically show oncocytic epithelial cells without atypia admixed with polymorphous lymphocytes and cellular debris. Mucinous differentiation and squamous cells with mixed inflammation and cytological are rarely encountered.[17][18] Fine needle aspiration cytology is a useful method for preoperative assessment of Warthin tumors. However, its accuracy is controversial compared with other methods. The confirmation of diagnosis with certainty relies on histopathological examination.
Microscopic Findings
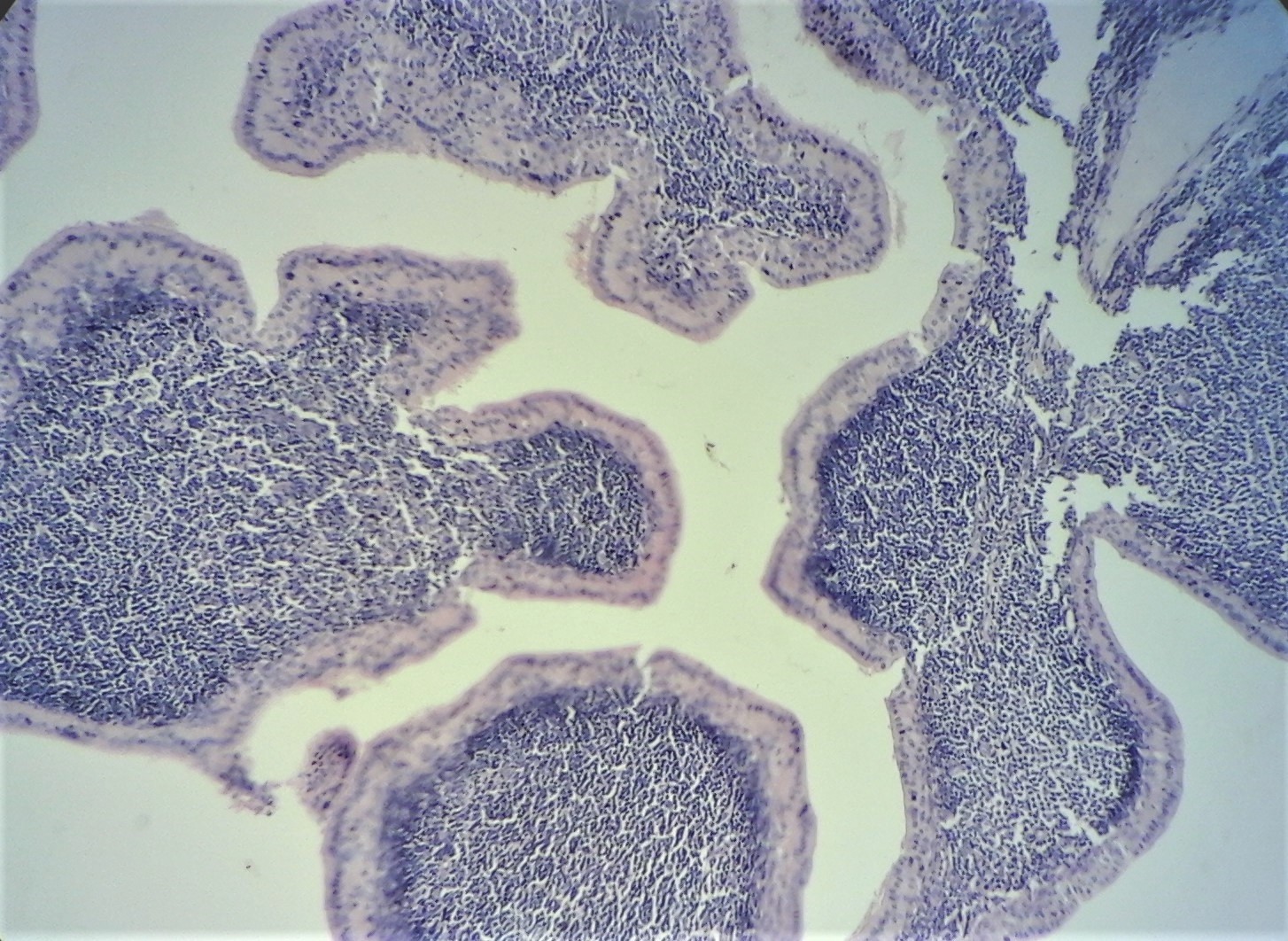
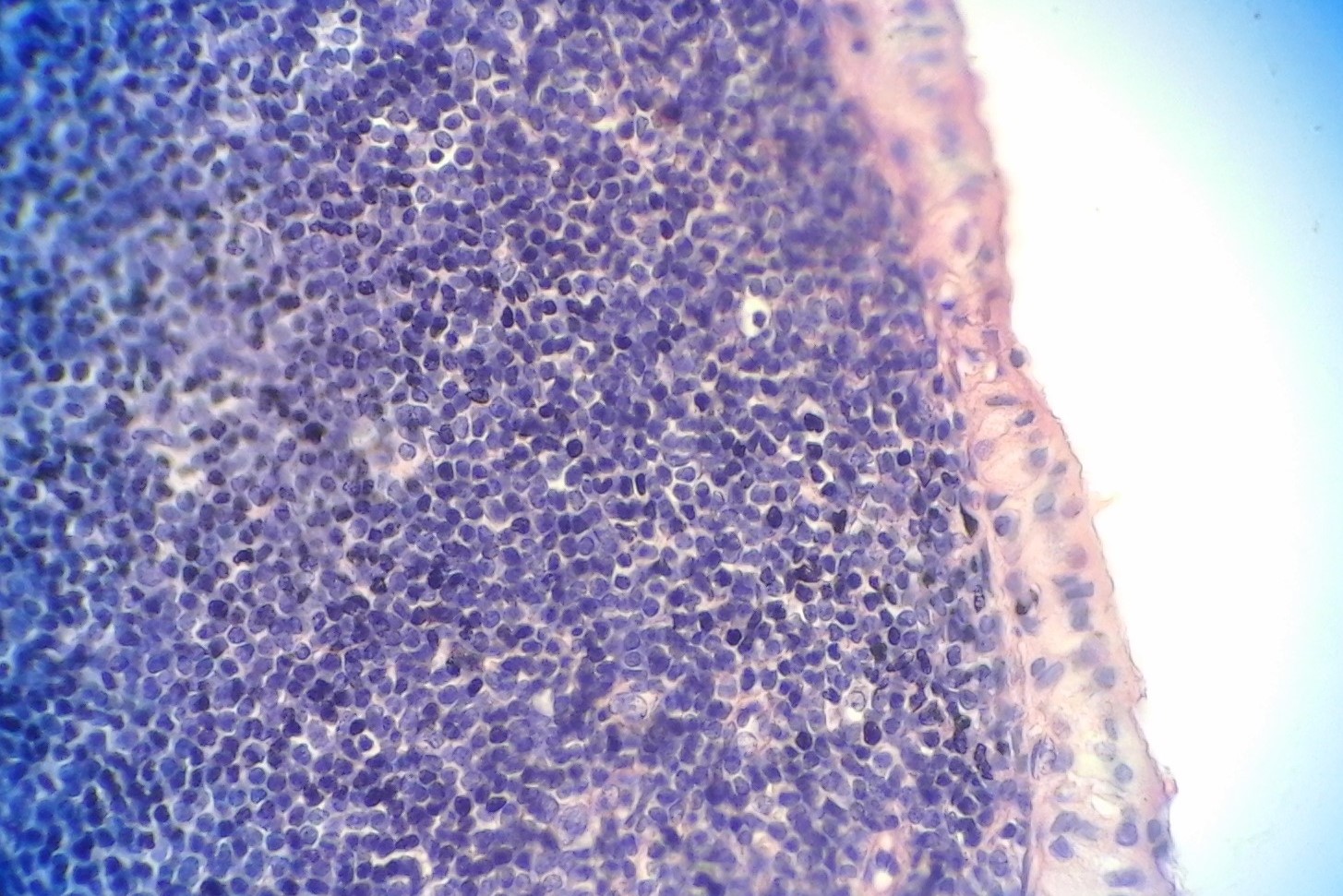
Warthin tumors are composed of varying proportions of papillary-cystic structures lined by oncocytic epithelial cells and a lymphoid stroma with germinal centers (see Image. Bilayered Eosinophilic Oncocytic Epithelium Lining the Cyst Lumen). The epithelial component is formed of inner columnar and outer cuboidal cells. Some foci of mucous, ciliated, sebaceous, and squamous cells can be present in Warthin tumors. A granulomatous reaction can be seen in some cases.[19] infarcted or metaplastic tumors may have marked mucinous or squamous metaplasia and stromal reaction, which may present diagnostic challenges.
The diagnosis of malignant transformation of Warthin tumor to carcinoma relies on :
- The presence of a Warthin tumor;
- The presence of transitional zones from a benign oncocytic to a malignant epithelium;
- The presence of an infiltrating growth in the surrounding lymphoid tissue;
- and the exclusion of metastasis to lymphoid stroma from another primary carcinoma.
Immunohistochemical study
- The epithelial component is immunoreactive for cytokeratin cocktail.
- The lymphoid portion shows kappa and lambda light-chain polyclonality
History and Physical
Clinically, Warthin tumor presents as a rounded or an ovoid nodular painless, slow-growing, fluctuant to firm at palpation. It can be unilateral, bilateral, or multicentric and is asymptomatic in 90% of cases. Warthin tumor induces little or no pain, ear ringing, ear pain, and hearing loss in some cases.[20] The size of a Warthin tumor can be several millimeters to centimeters and two to four centimeters on average.[21] According to one study, 56% of Warthin tumors measured one to three centimeters, and 40% measured four to six centimeters, with one case measuring more than ten centimeters.[21]
Evaluation
Ultrasonography
High-resolution ultrasonography is considered to be the modality of the first choice for the detection of neoplasms in the salivary glands. However, ultrasonography is unable to evaluate that portion of the parotid gland situated deep in the mandible. Ultrasonography of salivary gland masses includes the evaluation of the contralateral gland as well as the cervical lymph nodes. If the lesion requires to be identified before surgery, ultrasound-guided FNAC may be performed. In Warthin tumors, ultrasonography reveals a well-defined mass with multiple anechoic areas or an anechoic mass, with posterior acoustic enhancement at the lower pole of the parotid. Nevertheless, the pattern may vary, and fast growth secondary to infection may occur. In some cases, multiple septa and the thickness of intratumoral fluid give a heterogeneous echogenic pattern. Since Warthin tumors are often multiple and bilateral, the contralateral gland should always be examined.[22]
Magnetic Resonance Imaging
On MRI examination, Warthin tumors are often seen as encapsulated lesions that show low or intermediate T1-weighted signal features. The neoplasm shows intermediate signal intensity on T2-weighted images.[23] The solid portion is predominant in the Warthin tumors, and small cystic parts are seen in about 30% with thin uniform walls without enhancement. Well defined contour is a crucial finding in distinguishing benign parotid tumors from malignant neoplasms. Magnetic resonance imaging is useful to identify the capsule and contour feature and content of the mass owing to higher soft-tissue resolution.[23] Both MRI and multislice CT have the capacity of multiplanar demonstration of the tumors. Multislice CT provides acceptable timing for the contrast enhancement optimization and an applicable method.
Treatment / Management
The optimal treatment of Warthin tumor relies on surgical removal, which can be easily realized due to the superficial location of the tumor. Some surgeons prefer the superficial parotidectomy to avoid the rupture of the tumor capsule, whereas others chose local resection with the surrounding tissue.[2] Some authors considered that the likelihood of malignant transformation of Warthin tumors is only 0.3% and that it is a frankly benign neoplasm of the salivary glands. Hence, they certified that enucleation was the best treatment modality for this tumor.[24] Another study stipulated that parotidectomy reduces the recurrence rate of Warthin tumor significantly because of its possible bilaterality and multicentricity.[25](B2)
Since the Warthin tumor is well-defined and because of its superficial location on the surface layer of the parotid gland, some authors prefer to perform superficial parotidectomy. The best treatment option for Warthin tumor located in the deep lobe is deep parotidectomy following superficial parotidectomy and confirmation of the facial nerves. According to some authors, since Warthin tumor is often located in the tail of the parotid gland, partial parotidectomy could be a relevant option. Partial parotidectomy excises not only the bottom branches of the facial nerves but also the tumor, including the neighboring normal tissues.
Differential Diagnosis
Histological differential diagnosis
- Lymph node metastases: usually there is marked cellular atypia. Lymph node metastases are devoid of the bilayered, oncocytic epithelial element
- Sebaceous lymphadenoma: it is devoid of the bilayered, oncocytic epithelial element
- Cystadenomas of the salivary glands: they can be oncocytic however, they are devoid of lymphoid stroma and usually have small, multilocular cystic spaces.
- Lymphoepithelial cysts
Prognosis
Warthin’s tumor has a favorable prognosis and almost never recurs. Malignant degeneration of Warthin tumor is very rare. In such cases, a close follow-up of the patients is mandatory so as to detect metastases. According to some authors, the enucleation of Warthin tumor or follow-up without removal may be sufficient.
Complications
Local Recurrence
The local recurrence rate is low; when recurrence does occur, it is probably due to multifocal tumors or inadequate excision.
Malignant Transformation
Malignant transformation in a Warthin tumor is extremely rare; however, there are a few reported examples in both the epithelial and the lymphoid component. The most frequent histological types of malignant transformation in a Warthin tumor are mucoepidermoid carcinoma, squamous cell carcinoma, undifferentiated carcinoma, oncocytic adenocarcinoma, and adenocarcinoma.
Consultations
- Otolaryngologist
- Maxillofacial surgeon
- Radiologist
- Pathologist
Deterrence and Patient Education
It is mandatory that patients consult an otolaryngologist whenever they detect any swelling in the parotid gland. The interprofessional team should ensure that the patients are well informed about Warthin tumor of the parotid gland. Patients should be informed about educational websites so as to help them better understand this benign neoplasm, its outcome, and its treatment. Patient education plays a crucial role in the deterrence of the processes that can cause a Warthin tumor. Specialty-trained nurses often do this. For instance, advise the patient to stop smoking since Warthin tumor is linked to tobacco.
Enhancing Healthcare Team Outcomes
Management of Warthin tumor needs an interprofessional approach involving a team that consists of an otolaryngologist, maxillofacial surgeon, radiologist, and pathologist. The primary care provider and NP must refer patients with any parotid lump to an otolaryngologist for further workup. All health professionals must coordinate their actions to enhance the management of patients with Warthin tumor. Coordination starts with appropriate communication between doctors, nurses, and pharmacists.
The optimal treatment of Warthin tumor relies on surgical removal of the tumor. The interprofessional team should perform an exhaustive preoperative workup to minimize postoperative complications of surgery. This will result in a better patient outcome.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Mathur A, Mehrotra ML, Dhaliwal U. Warthin's tumour of the eye lid. Indian journal of ophthalmology. 1989 Oct-Dec:37(4):193 [PubMed PMID: 2638310]
Level 3 (low-level) evidenceMaiorano E, Lo Muzio L, Favia G, Piattelli A. Warthin's tumour: a study of 78 cases with emphasis on bilaterality, multifocality and association with other malignancies. Oral oncology. 2002 Jan:38(1):35-40 [PubMed PMID: 11755819]
Level 2 (mid-level) evidenceGallo O, Bocciolini C. Warthin's tumour associated with autoimmune diseases and tobacco use. Acta oto-laryngologica. 1997 Jul:117(4):623-7 [PubMed PMID: 9288224]
Level 2 (mid-level) evidenceCennamo A, Falsetto A, Gallo G, Lanna M, Calleri G, Di Giacomo D. Warthin's tumour in the parotid gland (an inflammatory or a neoplastic disease?). Chirurgia italiana. 2000 Jul-Aug:52(4):361-7 [PubMed PMID: 11190526]
Kristensen S, Tveterås K, Friedmann I, Thomsen P. Nasopharyngeal Warthin's tumour: a metaplastic lesion. The Journal of laryngology and otology. 1989 Jun:103(6):616-9 [PubMed PMID: 2769033]
Level 3 (low-level) evidenceKale AD, Prasad UC. Re: Yu et al. Smoking and the development of Warthin's tumour of the parotid gland. The British journal of oral & maxillofacial surgery. 1999 Jun:37(3):245 [PubMed PMID: 10454034]
Level 3 (low-level) evidenceTherkildsen MH, Christensen N, Andersen LJ, Larsen S, Katholm M. Malignant Warthin's tumour: a case study. Histopathology. 1992 Aug:21(2):167-71 [PubMed PMID: 1505934]
Level 3 (low-level) evidenceNishikawa H, Kirkham N, Hogbin BM. Synchronous extra-parotid Warthin's tumour. The Journal of laryngology and otology. 1989 Aug:103(8):792-3 [PubMed PMID: 2769053]
Level 3 (low-level) evidenceA R R, Rehani S, Bishen KA, Sagari S. Warthin's Tumour: A Case Report and Review on Pathogenesis and its Histological Subtypes. Journal of clinical and diagnostic research : JCDR. 2014 Sep:8(9):ZD37-40. doi: 10.7860/JCDR/2014/8503.4908. Epub 2014 Sep 20 [PubMed PMID: 25386545]
Level 3 (low-level) evidenceKotwall CA. Smoking as an etiologic factor in the development of Warthin's tumor of the parotid gland. American journal of surgery. 1992 Dec:164(6):646-7 [PubMed PMID: 1334381]
Level 2 (mid-level) evidenceTHOMPSON AS, BRYANT HC Jr. Histogenesis of papillary cystadenoma lymphomatosum (Warthin's tumor) of the parotid salivary gland. The American journal of pathology. 1950 Sep:26(5):807-49 [PubMed PMID: 15432614]
Bullerdiek J, Haubrich J, Meyer K, Bartnitzke S. Translocation t(11;19)(q21;p13.1) as the sole chromosome abnormality in a cystadenolymphoma (Warthin's tumor) of the parotid gland. Cancer genetics and cytogenetics. 1988 Oct 1:35(1):129-32 [PubMed PMID: 3180001]
Level 3 (low-level) evidenceAguirre JM, Echebarría MA, Martínez-Conde R, Rodriguez C, Burgos JJ, Rivera JM. Warthin tumor. A new hypothesis concerning its development. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 1998 Jan:85(1):60-3 [PubMed PMID: 9474616]
Seifert G, Bull HG, Donath K. Histologic subclassification of the cystadenolymphoma of the parotid gland. Analysis of 275 cases. Virchows Archiv. A, Pathological anatomy and histology. 1980:388(1):13-38 [PubMed PMID: 7467121]
Level 3 (low-level) evidenceSantucci M, Gallo O, Calzolari A, Bondi R. Detection of Epstein-Barr viral genome in tumor cells of Warthin's tumor of parotid gland. American journal of clinical pathology. 1993 Dec:100(6):662-5 [PubMed PMID: 8249914]
Köybaşioğlu FF, Önal B, Han Ü, Adabağ A, Şahpaz A. Cytomorphological findings in diagnosis of Warthin tumor. Turkish journal of medical sciences. 2020 Feb 13:50(1):148-154. doi: 10.3906/sag-1901-215. Epub 2020 Feb 13 [PubMed PMID: 31769640]
Schindler S, Nayar R, Dutra J, Bedrossian CW. Diagnostic challenges in aspiration cytology of the salivary glands. Seminars in diagnostic pathology. 2001 May:18(2):124-46 [PubMed PMID: 11403256]
Kawasaki T, Kanamaru T, Shingaki S, Mizutani H, Nakajima T. Cytologic study of salivary gland tumors. International journal of oral surgery. 1980 Feb:9(1):68-73 [PubMed PMID: 6769832]
Chen SL, Hwang CC, Liu YC, Chen WT, Yang SW. Warthin's tumor with necrotizing tuberculous granulomatous inflammation causing severe facial nerve adhesion in parotid gland: A case report and literature review. Medicine. 2020 Feb:99(7):e18763. doi: 10.1097/MD.0000000000018763. Epub [PubMed PMID: 32049782]
Level 3 (low-level) evidencePsychogios G, Vlastos I, Thölken R, Zenk J. Warthin's tumour seems to be the most common benign neoplasm of the parotid gland in Germany. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2020 Jul:277(7):2081-2084. doi: 10.1007/s00405-020-05894-z. Epub 2020 Mar 18 [PubMed PMID: 32189070]
Párraga-Linares L, Aguirre-Urízar JM, Berini-Aytés L, Gay-Escoda C. Papillary cystoadenoma lymphomatosum (Warthin-like) of minor salivary glands. Medicina oral, patologia oral y cirugia bucal. 2009 Nov 1:14(11):e597-600 [PubMed PMID: 19680204]
Level 3 (low-level) evidenceShimizu M, Ussmüller J, Hartwein J, Donath K. A comparative study of sonographic and histopathologic findings of tumorous lesions in the parotid gland. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 1999 Dec:88(6):723-37 [PubMed PMID: 10625857]
Level 2 (mid-level) evidenceAlibek S, Zenk J, Bozzato A, Lell M, Grunewald M, Anders K, Rabe C, Iro H, Bautz W, Greess H. The value of dynamic MRI studies in parotid tumors. Academic radiology. 2007 Jun:14(6):701-10 [PubMed PMID: 17502260]
Batsakis JG. Carcinoma ex papillary cystadenoma lymphomatosum. Malignant Warthin's tumor. The Annals of otology, rhinology, and laryngology. 1987 Mar-Apr:96(2 Pt 1):234-5 [PubMed PMID: 3566067]
Teymoortash A, Krasnewicz Y, Werner JA. Clinical features of cystadenolymphoma (Warthin's tumor) of the parotid gland: a retrospective comparative study of 96 cases. Oral oncology. 2006 Jul:42(6):569-73 [PubMed PMID: 16469528]
Level 2 (mid-level) evidence