Introduction
Double external defibrillation (DED) is the application and administration of transthoracic electrical currents from two defibrillator devices to a single patient experiencing a single type of lethal dysrhythmia during cardiac arrest, known as refractory ventricular fibrillation (RVF).[1][2]
In November of 2020, the American Heart Association guidelines changed. "The usefulness of double sequential defibrillation for refractory shockable rhythm has not been established." It is currently not recommended.
This use of DED occurs after standard transthoracic electrical current from a single defibrillator have failed to terminate this lethal rhythm. Refractory ventricular fibrillation is defined as ventricular fibrillation that does not convert with three or more single defibrillation attempts.[2][3] The estimated incidence of RVF is 0.5 to 0.6 per 100000 of the population; some authors report that 10 to 25% of cardiac arrest cases could develop RVF or recurrent VF.[3][4][5] Patients who experience RVF during their cardiac arrest have a mortality of up to 97%.[6][7]
Proposed Theories
1) Power Theory
- Studies have shown that higher energy has improved success on subsequent defibrillation.[8][9][10][11] One of the leading theories behind the success of DED is that the administration of more joules during transthoracic defibrillation allows for the conversion of all the myocytes out of RVF. This approach requires the two electrical currents from both defibrillator devices to be administered at the same time or as close together as possible and is where DED gets one of it’s more common names of “double simultaneous defibrillation” (DSiD).[12][13][14]
2) Setting Up Theory
- Another leading theory behind DED suggests that that the first transthoracic current lowers the defibrillation threshold, which then increases the second transthoracic current’s success at converting any remaining fibrillating myocytes.[1][15] This theory requires a deliberate pause when administering the two electrical currents to ensure they are close together but not delivered at exactly the same time, and is where DED gets its most common name of “double sequential defibrillation” (DSD).
3) Multiple Vector Theory
- Another hypothesized theory behind DED directly applies to the two proposed theories above and suggests that application of multiple defibrillator pads increases the number of vectors the electrical current can use to reach the myocardium.[1][15]
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
Early DED is indicated for refractory ventricular fibrillation (RVF). RVF is ventricular fibrillation that does not convert or respond to three or more single defibrillation attempts.[2][3]
Contraindications
Double defibrillation does not have any relative or absolute contraindications. The patient having a pacemaker or implanted automated internal cardiac defibrillator does not change the indication of DED.
Equipment
- Two biphasic defibrillators
- Two sets of defibrillator pads
Personnel
If attempting the power theory; one experienced ACLS qualified healthcare provider is needed to operate both defibrillator devices. If using the setting up theory, then two experienced ACLS qualified healthcare providers are necessary, each operating one of the two defibrillator devices.
Preparation
Begin efforts at obtaining and setting up the second defibrillator if the patient is in ventricular fibrillation and requires a second shock. The placement of this second defibrillator device should be physically close to the first defibrillator, should the two need to be operated by one individual. If the patient was already defibrillated two or more times in the pre-hospital setting, then apply the pads as mentioned below when transferring the patient from the ambulance stretcher to the hospital bed.
- While many defibrillators still have the manual paddles, most manufacturers recommend the use of the adhesive “hands-free” pads. These pads should be the only method of administering DED to ensure adequate delivery of energy and to avoid any operator interference that may occur when using the paddles. Ensure you have the correct size pads on the second defibrillator device before application onto the patient.
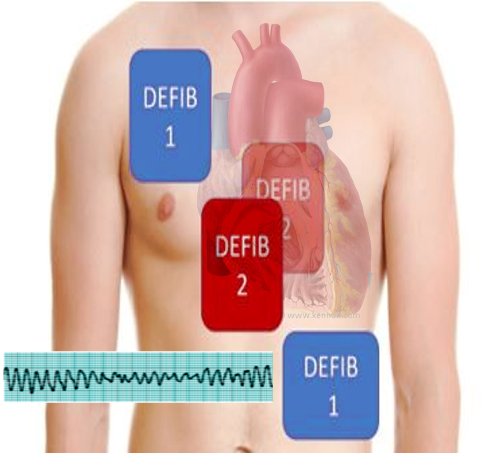
Pad Placement
- The first set of defibrillator pads should remain in their original location, one pad along the upper right sternal border and the second at the cardiac apex.
- IMPORTANT: If the pads touch one another, there is a significant risk of damaging one or BOTH defibrillators. Device manufacturers do not cover damage to the defibrillators using DED
There are two location options for placement of the second defibrillator pads:
- The first pad should be immediately medial or lateral to the pad located at the right sternal border without touching that first pad. The second pad should also be placed immediately medial or lateral to the first defibrillator pad located at the cardiac apex and also not touching it
- An anteroposterior placement of the second set of defibrillator pads is also an option. This method is preferred as the pads can easily be applied when transferring patients from pre-hospital stretcher to hospital bed. Furthermore, there is less risk of the pads touching and damaging the defibrillator devices.
Technique or Treatment
If attempting DED simultaneously using the power theory then it is recommended that a single healthcare provider operate both defibrillator devices to ensure the administration of is as close together as possible
If attempting DED sequentially using the setting up theory, then it is recommended that two healthcare providers each operate a single defibrillator device to ensure an intentional delay exists between the two administered shocks. Alternatively, if only one ACLS qualified healthcare provider is available, then the “shock” button on both defibrillators can be pushed with one hand to ensure the creation of the intentional delay.
As per the current ACLS recommendation with single defibrillation minimize interruptions to chest compressions. CPR should continue while both defibrillators are charging to their initial energy level of 200 Joules. Once both devices become fully charged, and the scene is checked to make sure that no one is touching the patient or in contact with anything touching the patient, administer the shock as described using one of the two methods detailed above. CPR should immediately resume following administration of DED, and the patient’s pulse checked after that 2-minute cycle of compressions.
Complications
Several studies have shown that safety in a patient receiving up to 720 Joules. Furthermore, studies indicate that energy level does not require adjustment for the weight.[1][9][13][14]
As mentioned previously, there is a risk of damaging one or both defibrillator devices if any of the pads are touching one another when delivering the two shocks. To reiterate, damage to a defibrillator from the administration of DED is typically not covered by the manufacturer’s warranty.
Clinical Significance
Several case reports show the effectiveness of a second defibrillator for terminating RVF.[1][8][16][17][18] A large literature review showed DED terminating RVF in 77% of 39 cases with 11 of those patients being discharge with good neurologic outcomes indicated by a Cerebral Performance Category Score of 2 or less.[19] There is currently no evidence suggesting the use of the power theory or the setting up theory is more successful in the administration of DED or the termination of RVF. While more studies are necessary to understand DED better, the use of a second defibrillator may provide benefit and should be a consideration when treating RVF.
Enhancing Healthcare Team Outcomes
There is still much unknown regarding double external defibrillation. Future studies are required to understand better whether DSD or DSiD leads to better outcomes and whether or not increased size of the defibrillator pads, to allow more surface area for the vectors of electricity, leads to more successful defibrillation. Until then, the focus during any cardiac arrest remains early defibrillation and high-quality cardiopulmonary resuscitation. DED serves as another tool in during cardiac arrest and should be an option with other advanced life-saving therapies such as ECMO and cardiac catheterization.
Administration of double defibrillation requires an interprofessional team approach, including physicians, specialists, specialty-trained nurses, and emergency medical personnel, all collaborating across disciplines to achieve optimal patient results. [Level V]
Media
References
Hoch DH, Batsford WP, Greenberg SM, McPherson CM, Rosenfeld LE, Marieb M, Levine JH. Double sequential external shocks for refractory ventricular fibrillation. Journal of the American College of Cardiology. 1994 Apr:23(5):1141-5 [PubMed PMID: 8144780]
Eifling M, Razavi M, Massumi A. The evaluation and management of electrical storm. Texas Heart Institute journal. 2011:38(2):111-21 [PubMed PMID: 21494516]
Sakai T, Iwami T, Tasaki O, Kawamura T, Hayashi Y, Rinka H, Ohishi Y, Mohri T, Kishimoto M, Nishiuchi T, Kajino K, Matsumoto H, Uejima T, Nitta M, Shiokawa C, Ikeuchi H, Hiraide A, Sugimoto H, Kuwagata Y. Incidence and outcomes of out-of-hospital cardiac arrest with shock-resistant ventricular fibrillation: Data from a large population-based cohort. Resuscitation. 2010 Aug:81(8):956-61 [PubMed PMID: 20653086]
Level 2 (mid-level) evidenceSarkozy A, Dorian P. Strategies for reversing shock-resistant ventricular fibrillation. Current opinion in critical care. 2003 Jun:9(3):189-93 [PubMed PMID: 12771668]
Level 3 (low-level) evidenceDorian P, Cass D, Schwartz B, Cooper R, Gelaznikas R, Barr A. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. The New England journal of medicine. 2002 Mar 21:346(12):884-90 [PubMed PMID: 11907287]
Level 1 (high-level) evidenceWindecker S. Percutaneous left ventricular assist devices for treatment of patients with cardiogenic shock. Current opinion in critical care. 2007 Oct:13(5):521-7 [PubMed PMID: 17762230]
Level 3 (low-level) evidenceHerlitz J,Bång A,Holmberg M,Axelsson A,Lindkvist J,Holmberg S, Rhythm changes during resuscitation from ventricular fibrillation in relation to delay until defibrillation, number of shocks delivered and survival. Resuscitation. 1997 Feb; [PubMed PMID: 9051819]
Leacock BW. Double simultaneous defibrillators for refractory ventricular fibrillation. The Journal of emergency medicine. 2014 Apr:46(4):472-4. doi: 10.1016/j.jemermed.2013.09.022. Epub 2014 Jan 21 [PubMed PMID: 24462025]
Level 3 (low-level) evidenceStiell IG, Walker RG, Nesbitt LP, Chapman FW, Cousineau D, Christenson J, Bradford P, Sookram S, Berringer R, Lank P, Wells GA. BIPHASIC Trial: a randomized comparison of fixed lower versus escalating higher energy levels for defibrillation in out-of-hospital cardiac arrest. Circulation. 2007 Mar 27:115(12):1511-7 [PubMed PMID: 17353443]
Level 1 (high-level) evidenceKoster RW, Walker RG, Chapman FW. Recurrent ventricular fibrillation during advanced life support care of patients with prehospital cardiac arrest. Resuscitation. 2008 Sep:78(3):252-7. doi: 10.1016/j.resuscitation.2008.03.231. Epub 2008 Jun 16 [PubMed PMID: 18556106]
Walsh SJ, McClelland AJ, Owens CG, Allen J, Anderson JM, Turner C, Adgey AA. Efficacy of distinct energy delivery protocols comparing two biphasic defibrillators for cardiac arrest. The American journal of cardiology. 2004 Aug 1:94(3):378-80 [PubMed PMID: 15276112]
Level 3 (low-level) evidenceMorgan JP, Hearne SF, Raizes GS, White RD, Giuliani ER. High-energy versus low-energy defibrillation: experience in patients (excluding those in the intensive care unit) at Mayo Clinic-affiliated hospitals. Mayo Clinic proceedings. 1984 Dec:59(12):829-34 [PubMed PMID: 6503363]
Level 1 (high-level) evidenceChen B, Yin C, Ristagno G, Quan W, Tan Q, Freeman G, Li Y. Retrospective evaluation of current-based impedance compensation defibrillation in out-of-hospital cardiac arrest. Resuscitation. 2013 May:84(5):580-5. doi: 10.1016/j.resuscitation.2012.09.017. Epub 2012 Sep 20 [PubMed PMID: 23000364]
Level 2 (mid-level) evidenceWhite RD, Blackwell TH, Russell JK, Jorgenson DB. Body weight does not affect defibrillation, resuscitation, or survival in patients with out-of-hospital cardiac arrest treated with a nonescalating biphasic waveform defibrillator. Critical care medicine. 2004 Sep:32(9 Suppl):S387-92 [PubMed PMID: 15508666]
Level 2 (mid-level) evidencePourmand A, Galvis J, Yamane D. The controversial role of dual sequential defibrillation in shockable cardiac arrest. The American journal of emergency medicine. 2018 Sep:36(9):1674-1679. doi: 10.1016/j.ajem.2018.05.078. Epub 2018 Jun 1 [PubMed PMID: 29880409]
Cabañas JG, Myers JB, Williams JG, De Maio VJ, Bachman MW. Double Sequential External Defibrillation in Out-of-Hospital Refractory Ventricular Fibrillation: A Report of Ten Cases. Prehospital emergency care. 2015 January-March:19(1):126-130 [PubMed PMID: 25243771]
Level 3 (low-level) evidenceCortez E, Krebs W, Davis J, Keseg DP, Panchal AR. Use of double sequential external defibrillation for refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation. 2016 Nov:108():82-86. doi: 10.1016/j.resuscitation.2016.08.002. Epub 2016 Aug 10 [PubMed PMID: 27521470]
El Tawil C, Mrad S, Khishfe BF. Double sequential defibrillation for refractory ventricular fibrillation. The American journal of emergency medicine. 2017 Dec:35(12):1985.e3-1985.e4. doi: 10.1016/j.ajem.2017.09.009. Epub 2017 Sep 8 [PubMed PMID: 28978402]
Hajjar K, Berbari I, El Tawil C, Bou Chebl R, Abou Dagher G. Dual defibrillation in patients with refractory ventricular fibrillation. The American journal of emergency medicine. 2018 Aug:36(8):1474-1479. doi: 10.1016/j.ajem.2018.04.060. Epub 2018 Apr 30 [PubMed PMID: 29730094]