Introduction
Coronary artery disease (CAD) is a common pathologic process affecting more than 15 million Americans every year.[1] Currently, it is listed as the most common cause of death in both men and women, accounting for 24.2% and 22.0% of all deaths, respectively, in 2016. CAD is characterized by a narrowing or blockage within the coronary arteries, often related to atherosclerosis. CAD, when significant, often results in reduced and inadequate blood flow to the myocardium leading to myocardial injury related to diminished oxygen and nutrient supply. Myocardial injury related to CAD often presents clinically as an acute coronary syndrome (ACS), including unstable angina (UA), non-ST segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI). ACS is a group of conditions characterized by angina or anginal equivalents that require emergency medical evaluation and treatment.
Cardiac catheterization with angiography is a minimally invasive diagnostic procedure and imaging modality that has become a mainstay in evaluating CAD.[2] During catheterization, a sheath gets introduced to the arterial system via either the femoral or, increasingly more commonly, the radial artery. A catheter is then advanced through the arterial system under fluoroscopy to the aortic root. Iodinated contrast is then utilized to visualize the aortic valve cusps and gain access to the right and left coronary arteries. After gaining access to individual coronary arteries utilizing a variety of guidewires, angiography is performed utilizing contrast to identify significant stenosis, atherosclerotic lesions, or blockages within individual arteries. Historically, the significance of these lesions has been determined by visual approximation and estimation performed by a cardiologist trained in either diagnostic or interventional cardiac catheterization. A study published in February 2018 evaluated coronary artery lesions treated with percutaneous coronary intervention (PCI) in China confirmed that physician visual assessment (PVA) of stenosis resulted in higher readings of stenosis severity when compared with quantitative coronary angiography (QCA). Additionally, the study revealed significant variations across hospitals and physicians, confirming the utility of additional diagnostic studies.[3]
Significant lesions, those with greater than 70% luminal narrowing, via visual estimation qualify for intervention utilizing techniques such as balloon angioplasty or percutaneous intervention with coronary artery stent placement. Lesions displaying less than 40% stenosis are determined non-significant, and the recommendation in these cases is to optimize medical therapy for treating CAD. Interventions in patients with indeterminate lesions, between 40% and 70% stenosis, previously were subject to debate. In the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE, 2007), revascularization with PCI in stable CAD with high-grade stenosis failed to display benefit over optimal medical therapy.[4]
Additional diagnostic modalities have been developed to characterize these lesions better and identify those that would benefit from intervention, including fractional flow reserve (FFR) and instantaneous wave-free ratio (iFR). FFR is described in depth within its review article; however, FFR is a guidewire-based technique that measures blood pressure and flows through a specific lesion. The DEFER trial (2007) determined that the 5-year, event-free survival was not significantly different between patients who performed and deferred PCI on intermediate coronary stenosis with an FFR greater than 0.75.[5] In the study, fractional flow reserve versus angiography for guiding percutaneous coronary intervention (FAME), FFR-guided PCI reduced composites of death, nonfatal myocardial infarction (MI), and repeat revascularization at 1 year compared with standard PCI alone.[6] In FFR, the interventionist utilizes a specialized guidewire to measure flow velocities and pressure across a target lesion. Following administering a hyperemic agent, typically adenosine, the FFR value is calculated. Studies have suggested that lesions with an FFR value of less than 0.75 are suspicious for inducible ischemia and would benefit from PCI. In contrast, those with values greater than 0.75 are candidates for treatment with optimum medical therapy.
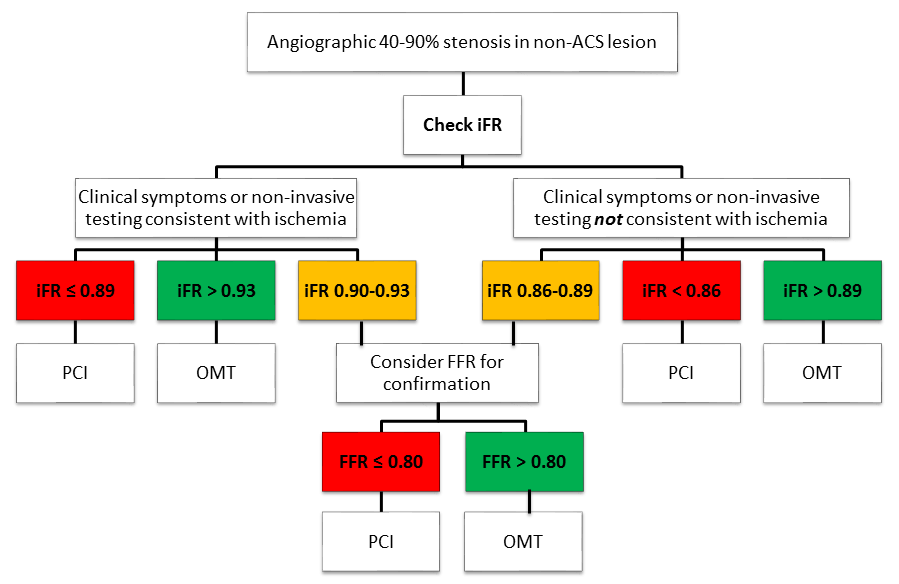
iFR is a newer physiologic measurement that utilizes principles similar to FFR but does not require a hyperemic agent. In a 2017 JACC study, iFR and FFR demonstrated no significant differences in the prediction of myocardial ischemia.[7] The MACE trial further justified using iFR, revealing that IiR-guided revascularization was non-inferior to FFR-guided revascularization for major adverse cardiac events at 1-year follow-up.[8] In iFR, the same pressure wires utilized in FFR get passed to a point distal to a stenotic lesion. During a period of diastole known as the “wave-free period,” iFR then calculates the ratio of the distal coronary artery pressure (Pd) to the pressure within the aortic outflow tract (Pa). During this timeframe completing blood flow complicating these measurements is negligible. Lesions found to have a Pd/Pa ratio less than 0.89 are determined to be significant and are non-inferior to the FFR cutoff of 0.8.[9][10] Coronary artery lesions with iFR ratios less than 0.89 and FFR ratios less than 0.8 are recommended for further treatment with PCI. As it is still a newer technology, some providers consider an iFR ratio of 0.86 to 0.93 an area of uncertainty and recommend a hybrid approach utilizing evaluation with FFR.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Relevant anatomy utilized during iFR is relatively limited, but detailed knowledge of the coronary vasculature is recommended and is reviewed elsewhere.
Indications
Indications for iFR are in patients with stable CAD and indeterminate lesions, between 40% and 70% stenosis.
Contraindications
There are no contraindications at this time for iFR. However, current recommendations for iFR do not include patients with ACS.
Equipment
iFR requires a specialized guidewire with pressure and flow velocity sensing capabilities and computer software that accurately calculates iFR values. Additional equipment, including the vascular sheath, cardiac catheters, and imaging modalities, are unchanged from traditional cardiac catheterization.
Personnel
iFR should be performed only by board-certified cardiologists with formal training in interventional cardiac catheterization.
Preparation
Once the computer software for calculating iFR is installed and specialized catheters are available, minimal additional setup is required compared to standard cardiac catheterization.
Technique or Treatment
In iFR, the same pressure wires utilized in FFR are passed to a point distal to a stenotic lesion. During a period of diastole known as the “wave-free period,” IiR then calculates the ratio of the distal coronary artery pressure (Pd) to the pressure within the aortic outflow tract (Pa). During this timeframe, completing blood flow complicating these measurements is negligible.
Complications
There are minimal complications associated directly with iFR; however, they are the same as those of a standard cardiac catheterization with angiography and PCI and include the following:
- Bleeding
- Access site hematoma and pseudoaneurysm
- Acute kidney injury caused by the contrast agent
- Anaphylaxis caused by the contrast agent
- Coronary artery dissection
Clinical Significance
Clinically, iFR may be utilized to assess indeterminate coronary artery stenosis further for lesions anywhere from 40% to 90%, but recommendations do not include patients with ACS. Patients with clinical symptoms or non-invasive testing consistent with ischemia and an iFR of 0.89 or less are candidates for PCI. While a patient with an iFR greater than 0.93 typically qualifies for optimization of medical therapy (OMT), those with a ratio of 0.90 to 0.93 should have a follow-up with FFR. In a patient with clinical symptoms not consistent with ischemia, PCI is recommended for iFR under 0.86. In those with an iFR ratio over 0.89, OMT is recommended. Patients with iFR ratios between 0.86 and 0.89 are recommended for FFR confirmation (see Image. iFR Flow Chart).[11]
Enhancing Healthcare Team Outcomes
In late 2018, the European Society of Cardiology (ESC) announced that it had incorporated iFR into its updated revascularization guidelines. The recommendations noted that iFR should be performed alongside FFR to objectively assess coronary lesions' hemodynamic relevance. The current AHA/ACC guidelines do not formally address using iFR during coronary revascularization. While an invasive cardiologist performs the procedure, the rest of the healthcare team should inform the patient about the importance of lifestyle changes in lowering the risk of coronary artery disease.
Media
(Click Image to Enlarge)
References
Sanchis-Gomar F, Perez-Quilis C, Leischik R, Lucia A. Epidemiology of coronary heart disease and acute coronary syndrome. Annals of translational medicine. 2016 Jul:4(13):256. doi: 10.21037/atm.2016.06.33. Epub [PubMed PMID: 27500157]
Libby P, Theroux P. Pathophysiology of coronary artery disease. Circulation. 2005 Jun 28:111(25):3481-8 [PubMed PMID: 15983262]
Zhang H, Mu L, Hu S, Nallamothu BK, Lansky AJ, Xu B, Bouras G, Cohen DJ, Spertus JA, Masoudi FA, Curtis JP, Gao R, Ge J, Yang Y, Li J, Li X, Zheng X, Li Y, Krumholz HM, Jiang L, China PEACE Collaborative Group. Comparison of Physician Visual Assessment With Quantitative Coronary Angiography in Assessment of Stenosis Severity in China. JAMA internal medicine. 2018 Feb 1:178(2):239-247. doi: 10.1001/jamainternmed.2017.7821. Epub [PubMed PMID: 29340571]
Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, Knudtson M, Dada M, Casperson P, Harris CL, Chaitman BR, Shaw L, Gosselin G, Nawaz S, Title LM, Gau G, Blaustein AS, Booth DC, Bates ER, Spertus JA, Berman DS, Mancini GB, Weintraub WS, COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. The New England journal of medicine. 2007 Apr 12:356(15):1503-16 [PubMed PMID: 17387127]
Level 1 (high-level) evidenceZimmermann FM, Ferrara A, Johnson NP, van Nunen LX, Escaned J, Albertsson P, Erbel R, Legrand V, Gwon HC, Remkes WS, Stella PR, van Schaardenburgh P, Bech GJ, De Bruyne B, Pijls NH. Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. European heart journal. 2015 Dec 1:36(45):3182-8. doi: 10.1093/eurheartj/ehv452. Epub 2015 Sep 23 [PubMed PMID: 26400825]
Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van' t Veer M, Klauss V, Manoharan G, Engstrøm T, Oldroyd KG, Ver Lee PN, MacCarthy PA, Fearon WF, FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. The New England journal of medicine. 2009 Jan 15:360(3):213-24. doi: 10.1056/NEJMoa0807611. Epub [PubMed PMID: 19144937]
Level 1 (high-level) evidenceHwang D, Jeon KH, Lee JM, Park J, Kim CH, Tong Y, Zhang J, Bang JI, Suh M, Paeng JC, Na SH, Cheon GJ, Cook CM, Davies JE, Koo BK. Diagnostic Performance of Resting and Hyperemic Invasive Physiological Indices to Define Myocardial Ischemia: Validation With (13)N-Ammonia Positron Emission Tomography. JACC. Cardiovascular interventions. 2017 Apr 24:10(8):751-760. doi: 10.1016/j.jcin.2016.12.015. Epub 2017 Mar 29 [PubMed PMID: 28365268]
Level 1 (high-level) evidenceGötberg M, Christiansen EH, Gudmundsdottir IJ, Sandhall L, Danielewicz M, Jakobsen L, Olsson SE, Öhagen P, Olsson H, Omerovic E, Calais F, Lindroos P, Maeng M, Tödt T, Venetsanos D, James SK, Kåregren A, Nilsson M, Carlsson J, Hauer D, Jensen J, Karlsson AC, Panayi G, Erlinge D, Fröbert O, iFR-SWEDEHEART Investigators. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. The New England journal of medicine. 2017 May 11:376(19):1813-1823. doi: 10.1056/NEJMoa1616540. Epub 2017 Mar 18 [PubMed PMID: 28317438]
Berry C, van 't Veer M, Witt N, Kala P, Bocek O, Pyxaras SA, McClure JD, Fearon WF, Barbato E, Tonino PA, De Bruyne B, Pijls NH, Oldroyd KG. VERIFY (VERification of Instantaneous Wave-Free Ratio and Fractional Flow Reserve for the Assessment of Coronary Artery Stenosis Severity in EverydaY Practice): a multicenter study in consecutive patients. Journal of the American College of Cardiology. 2013 Apr 2:61(13):1421-7. doi: 10.1016/j.jacc.2012.09.065. Epub 2013 Feb 6 [PubMed PMID: 23395076]
Level 2 (mid-level) evidenceJeremias A, Maehara A, Généreux P, Asrress KN, Berry C, De Bruyne B, Davies JE, Escaned J, Fearon WF, Gould KL, Johnson NP, Kirtane AJ, Koo BK, Marques KM, Nijjer S, Oldroyd KG, Petraco R, Piek JJ, Pijls NH, Redwood S, Siebes M, Spaan JAE, van 't Veer M, Mintz GS, Stone GW. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting Pd/Pa with fractional flow reserve: the RESOLVE study. Journal of the American College of Cardiology. 2014 Apr 8:63(13):1253-1261. doi: 10.1016/j.jacc.2013.09.060. Epub 2013 Nov 6 [PubMed PMID: 24211503]
Level 2 (mid-level) evidenceCoughlan JJ, MacDonnell C, Arnous S, Kiernan TJ. Fractional flow reserve in 2017: current data and everyday practice. Expert review of cardiovascular therapy. 2017 Jun:15(6):457-472. doi: 10.1080/14779072.2017.1327810. Epub 2017 May 15 [PubMed PMID: 28475383]