Transcatheter Management of Left Ventricular Pseudoaneurysms
Transcatheter Management of Left Ventricular Pseudoaneurysms
Introduction
Left ventricular pseudoaneurysms (LVP) is a very rare but lethal complication of myocardial infarction, cardiac surgery, trauma, and infection.[1] [2] [3] LVP is characterized by left ventricle wall ruptures and is contained by pericardium or scar tissue.[1] Patients with LVP can present with congestive heart failure, arrhythmias. Development of tamponade after left ventricular rupture is usually fatal.[4] Casapo et al reported the incidence rate of LVP at around 0.29% (Clin Cardiol 1997). Studies suggest that, of all causes of LVP, myocardial infarction and cardiac surgery results in 55% and 33% respectively.[1] In cardiac surgery, Mitral Valve replacement is associated with a higher rate of LVP. [5]Traditionally, the preferred management of a left ventricular pseudoaneurysm has been emergency surgical intervention. The surgery itself has high mortality ranging from 20-36% but some of the recent studies have shown improvement in mortality to 10 %.[1] [[6] [7] [8] However cases, where surgery cannot be considered because of high risk and medical management is preferred, mortality is even high and its close to around 48 %.[5] But in last two decade or so, enhanced transcatheter procedural approaches and advanced device technology has made the percutaneous closure of LVP an increasingly practical option, especially in a patient with an unfavorable predicted surgical outcome. Percutaneous closure of the left ventricular pseudoaneurysm was first described by Clift et al10 in 2004.[9] In 2016, Okuyama and colleagues performed the first case of a PTC successfully following transcatheter aortic valve replacement using trans-apical access.[10] Before that, most cases reported in the literature were performed via surgery following life-threatening myocardial infarctions. There is no large study on the transcatheter management of LVP but multiple successful case studies have been reported which vouch for its future potential. There are also some reports of a hybrid approach which uses the PTC of the LVP to first stabilize the patient during the emergency setting followed by the gold standard surgical closure.[11] This article will discuss in detail the anatomy of a left ventricular pseudoaneurysm, potential etiologies of LVP, indications for PTC, contraindications for PTC, the technique of PTC, possible complications of PTC, and the clinical significance of the advent of the PTC procedure.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
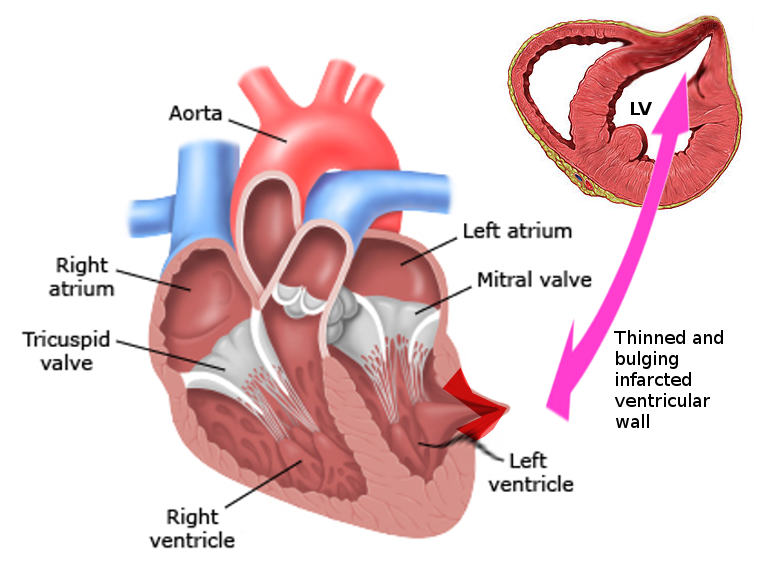
The left ventricular is made up of a thick muscle and forms the thickest muscle of the heart. It subsequently is prone to pseudoaneurysm development more commonly than true aneurysms. A pseudoaneurysm, also known as a false aneurysm, is when the wall is injured, and the leaking blood collects in the surrounding tissue. It should not be confused with a true aneurysm which occurs when the walls itself bulges from the fluid collection. A left ventricular pseudoaneurysm is a rupture of the left ventricular wall that is contained by adherent pericardium or scar tissue. Left ventricular pseudoaneurysm requires immediate intervention with either surgery or minimally invasive percutaneous transcatheter closure.
According to a study by Yeo et al, there is an association between the location of a pseudoaneurysm and the etiology of its presence. For example, following myocardial infarction, 82% of pseudoaneurysms are located in the inferior or posterolateral wall. Following congential cardiac surgery, pseudoaneurysms are found in the right ventricular outflow tract 87% of the time. After mitral valve replacement, 100% of pseudoaneurysms are located in the posterior subannular region of the mitral valve, and following aortic valve, replacement pseudoaneurysms are located in the subaortic region 100% of the time. [6]
Indications
Currently, the preferred method of treatment for LVP is emergency surgical intervention. However, percutaneous transcatheter LV closure is a feasible alternative for non-surgical candidates. Indications for this procedure is the presence of a left ventricular pseudoaneurysm in a patient who is a non-surgical candidate.
Contraindications
Contraindications to percutaneous transcatheter closure include left atrial thrombus,[12] active endocarditis, and/or the presence of cardiac anatomy unfavorable to catheter intervention.
Personnel
A skilled interventional cardiologist or structuralist knowledgeable or trained in percutaneous transcatheter LV closure technique is required to successfully and safely complete the procedure. The outcomes relative to the procedure are not available yet. Operator experience and volume are important factors, but given the rarity of this condition, even large referral centers have limited experience.[13] Personnel who may be present include a cardiac nurse, catheterization lab technician, and a cardiothoracic surgeon.
Preparation
Percutaneous transcatheter left ventricular closure is usually an emergent intervention. Ideally, on or before the day of the procedure the patient should receive instructions to fast at least 6 to 8 hours before the procedure starting. Anticoagulation should also be held prior to the procedure. If the patient is on warfarin, it will need to be held, and the patient must reach an international normalized ratio (INR) of at least 1.7 or less prior to or the day of the procedure. Also, before performing the PTC, right heart catheterization and/or left heart catheterization should be done to assess the pressures inside the heart and in the lungs. Additionally, a left ventriculogram is performed to assess the function and structure of the left ventricular wall. An anesthesiologist evaluation is optimal to determine the success of intubation and extubation. One case of a PVC of LVP in a child is an excellent example of the importance of the pre-procedure cardiac imaging in providing vital information to allow detailed planning of a management strategy for an unusual left ventricular pseudoaneurysm.[12] Detailed anatomy of the pseudo-aneurysmal sac and its communication can be easily viewed and assessed using a transoesophageal echocardiogram (TOE), CT Angiogram, or cardiac MRI.[14]
Technique or Treatment
Under transesophageal echocardiogram monitoring and anesthesia, using a femoral insertion, the procedure is begun with a transeptal approach. Once in the left atrium, a 7 French AL-2 (Amplatz Left Middle Type) guide catheter is used to capture the pseudoaneurysm, and a 0.035-in glide wire is advanced into it. A 5 Fr hypo tube is threaded over the glide wire into the cavity of the aneurysm and then glide wire is extracted. Multiple embolization coils of different lengths are advanced into the aneurysm cavity. The neck of the pseudoaneurysm is then occluded using a 12 mm AGA Amplatzer II vascular plug or duct occluder. There should be no communication between the LV cavity and the pseudoaneurysm cavity after deploying the plug. Following completion of the procedure, the patient should be monitored in the hospital for 1-2 days to assess for any complications.[14] Regular monitoring via echocardiogram is the recommended post-op procedure.
Complications
Complications of a percutaneous transcatheter left ventricular pseudoaneurysm closure include but are not limited to the following: bleeding, hematoma, infection, embolism of the closure device, arrhythmia, pacemaker dependence, stroke, and/or death. Since this procedure is rather new and the rate of intervention is low due to the low incidence of LVP, researchers need to perform more studies on the possible long-term effects/complications of this procedure.
Clinical Significance
The development of the PTC can provide lifesaving treatment to a cohort of patients who would have before been considered futile for surgical intervention or subjected to a sternotomy and cardiopulmonary bypass which both themselves have their own adverse effects.
Enhancing Healthcare Team Outcomes
The management of left ventricular wall pseudoaneurysm is challenging and complex. While once the domain of the cardiac surgeon, today it is realized that percutaneous transcatheter closure of the left ventricular pseudoaneurysm may be an alternative for patients not able to withstand surgical intervention. It also saves the patient a prolonged hospital stay, a sternotomy scar, and no need for cardiopulmonary bypass.[15] To achieve good outcomes the goals and objectives of the percutaneous transcatheter LVP closure have to be defined prior to taking the patient to the procedure. In some instances, chronic infection may preclude definitive repair thus the importance of incorporating assistance from an infectious disease consult. As with any other complex cardiac procedure, the preoperative workup should be thorough and the patient should be seen by a pulmonologist and cardiologist to optimize lung and cardiac function. Because of the potential risk of embolism, an echocardiogram must be performed prior to intervention to rule out the presence of a left atrial appendage thrombus. If a pericardial effusion or tamponade occurs during the closure, a prompt consult must be placed to a cardiothoracic surgeon.[16]
To further improve outcomes, an interprofessional team involving the specialty-trained clinicians and nurse should assess the patient preoperatively to determine the patient's candidacy for the procedure. Exceptions occur often in emergent situations. In these situations, it is optimal to review recent imaging if possible. Even in an emergency, a proper assessment of cardiac anatomy must be made to ensure the procedure will not be futile. Ideally, the cardiac team will have time to assess cardiac hemodynamics before initiating PTC of the LVP.[17]
In the post-op period, the role of the nurse and pharmacist is crucial. The patients must be monitored for pain, wound infection, hematoma or hemorrhage, and a variety of common postoperative complications such as atelectasis, deep vein thrombosis, and pain. Pharmacist involvement is essential for parenteral nutrition if complications result. The need for careful planning and discussion with other professionals involved in the management of the patient is strongly recommended to lower the morbidity and improve outcomes. (Level I)
To conclude, the outcomes relative to the procedure are not available yet. Operator experience and volume are important factors, but given the rarity of this condition, even large referral centers have limited experience.[13] Clinical outcome of percutaneous transcatheter left ventricular pseudoaneurysm closure depends on the degree of the pseudoaneurysm, location of the pseudoaneurysm, and the skill of the operator. However, to ensure the best outcomes, prompt consultation with an interprofessional group of specialists including a cardiothoracic surgeon, an interventional cardiologist, and a structuralist is recommended.
Media
References
Frances C, Romero A, Grady D. Left ventricular pseudoaneurysm. Journal of the American College of Cardiology. 1998 Sep:32(3):557-61 [PubMed PMID: 9741493]
Krawczyk-Ożóg A,Sorysz D,Dziewierz A,Rajtar-Salwa R,Daniec M,Dudek D, Apical pseudoaneurysm after transapical transcatheter aortic valve implantation. Polish archives of internal medicine. 2018 Jan 31; [PubMed PMID: 29219144]
Katada Y,Ito J,Shibayama K,Nakatsuka D,Kawano Y,Watanabe H,Tabata M, Transapical Transcatheter Closure of the Pseudoaneurysm in the Left Ventricular Outflow Tract After Aortic Valve Replacement. JACC. Cardiovascular interventions. 2016 Sep 26; [PubMed PMID: 27592012]
Van Tassel RA,Edwards JE, Rupture of heart complicating myocardial infarction. Analysis of 40 cases including nine examples of left ventricular false aneurysm. Chest. 1972 Feb [PubMed PMID: 5058893]
Level 3 (low-level) evidenceSakai K,Nakamura K,Ishizuka N,Nakagawa M,Hosoda S, Echocardiographic findings and clinical features of left ventricular pseudoaneurysm after mitral valve replacement. American heart journal. 1992 Oct [PubMed PMID: 1529909]
Yeo TC, Malouf JF, Oh JK, Seward JB. Clinical profile and outcome in 52 patients with cardiac pseudoaneurysm. Annals of internal medicine. 1998 Feb 15:128(4):299-305 [PubMed PMID: 9471934]
Level 2 (mid-level) evidencePrêtre R,Linka A,Jenni R,Turina MI, Surgical treatment of acquired left ventricular pseudoaneurysms. The Annals of thoracic surgery. 2000 Aug [PubMed PMID: 10969679]
Level 2 (mid-level) evidencePerek B,Jemielity M,Dyszkiewicz W, Clinical profile and outcome of patients with chronic postinfarction left ventricular false aneurysm treated surgically. The heart surgery forum. 2004 Apr 1 [PubMed PMID: 15138090]
Clift P,Thorne S,de Giovanni J, Percutaneous device closure of a pseudoaneurysm of the left ventricular wall. Heart (British Cardiac Society). 2004 Oct [PubMed PMID: 15367535]
Level 3 (low-level) evidenceOkuyama K,Chakravarty T,Makkar RR, Percutaneous transapical pseudoaneurysm closure following transcatheter aortic valve replacement. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 27619932]
Kadner A,Fasnacht M,Kretschmar O,Prêtre R, Traumatic free wall and ventricular septal rupture - 'hybrid' management in a child. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2007 May; [PubMed PMID: 17337199]
Level 3 (low-level) evidenceSrivastava NT,Hoyer MH, Thromboexclusion of an atypical left ventricular pseudoaneurysm. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 24824727]
Level 3 (low-level) evidenceAcharya D,Nagaraj H,Misra VK, Transcatheter closure of left ventricular pseudoaneurysm. The Journal of invasive cardiology. 2012 Jun; [PubMed PMID: 22684390]
Level 3 (low-level) evidenceUssia GP,Cammalleri V,De Vico P,Sergi D,Romeo F, Transcatheter closure of paravalvular leak secondary to left ventricular peri-annular pseudoaneurysm. European heart journal cardiovascular Imaging. 2013 Jun; [PubMed PMID: 23288889]
Level 3 (low-level) evidenceMendiz O,Fava C,Cerda M,Lev G,Caponi G,Valdivieso L, Percutaneous repair of left ventricular pseudoaneurysm after transcatheter aortic valve replacement. Cardiovascular revascularization medicine : including molecular interventions. 2017 Sep; [PubMed PMID: 28262477]
Sawlani N,Berry N,Sobieszczyk P,Kaneko T,Pelletier M,Shah P, Percutaneous Closure of a Delayed Left Ventricular Pseudoaneurysm After Transseptal Transcatheter Mitral Valve Replacement. JACC. Cardiovascular interventions. 2017 Jul 24; [PubMed PMID: 28668314]
Madan T,Juneja M,Raval A,Thakkar B, Transcatheter device closure of pseudoaneurysms of the left ventricular wall: An emerging therapeutic option. Revista portuguesa de cardiologia : orgao oficial da Sociedade Portuguesa de Cardiologia = Portuguese journal of cardiology : an official journal of the Portuguese Society of Cardiology. 2016 Feb; [PubMed PMID: 26852302]