Introduction
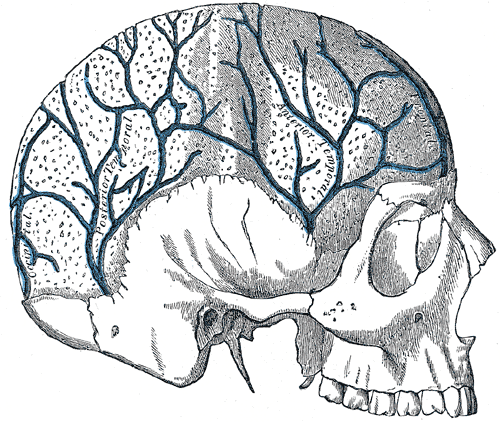
The scalp is a descriptive anatomical term that refers to the subcutaneous tissue that covers the cranium and is comprised of five layers: skin, dense connective tissue, epicranial aponeurosis, loose areolar connective tissue, and the periosteum. The first three layers move as one unit as they are tightly bound together. The veins of the scalp are present within the dense connective tissue, which also contains nerves and arteries, and the loose areolar connective tissue, which also contains emissary veins that connect to the diploic veins of the skull and the intracranial venous sinuses (see Image. Anterior Divisions, The Nerves fo the Scalp, Face, and Side of the Neck).
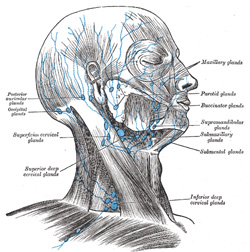
The venous drainage of the scalp divides into superficial and deep. The superficial veins of the scalp, starting anteriorly and moving posteriorly, are the supratrochlear and supraorbital veins, respectively, the superficial temporal veins and their branches, the posterior auricular vein, and the occipital vein and its branches (see Image. Veins in the Skull). The deep venous drainage is via the pterygoid venous plexus.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Venous anatomy starts with a thick outer layer of connective tissue called the tunica externa or adventitia, a middle layer of smooth muscle called the tunica media, and an interior layer of endothelial cells called the tunica intima.[1] As veins do not function like arteries in a primarily contractile manner and are not subject to the same kind of high pressures to which arteries are exposed, the smooth muscle layer of veins is less muscular than arteries. Veins also contain valves to prevent backflow.[2] The veins of the scalp serve to drain the deoxygenated blood from the scalp muscles and back to the right heart via the internal and external jugular veins and the superior vena cava. As previously mentioned, there are also the valveless emissary veins that connect the superficial veins to intracranial venous sinuses and diploic veins of the skull.
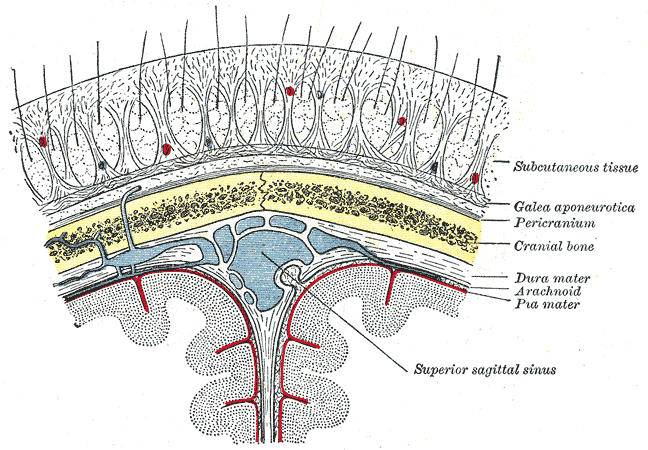
Here the blood supply and lymphatics of the scalp veins, starting with the superficial components anteriorly, and moving posteriorly, will be described (see Image. Lymphatic Supply for the Scalp).
Supratrochlear and Supraorbital Veins
The supratrochlear vein originates on the forehead, where it drains the superficial muscles and skin of the forehead and the front of the scalp supplied by the supratrochlear artery into the angular vein; there is no associated lymph tissue.
The supraorbital vein originates on the forehead, and its anastomosis with the frontal branch of the superficial temporal vein serves to drain the area of the forehead, eyebrow, and upper eyelid supplied by the supraorbital artery that anastomoses with the frontal branch of the superficial temporal vein.[3] The vein travels caudally over the frontal bone and superficial to the frontalis muscle before splitting to join the supratrochlear vein inferiorly and the superior ophthalmic vein medially; it also has no associated lymph tissue.
Superficial Temporal Vein
The superficial temporal vein has frontal and parietal branches, which drain the superficial muscles and skin of the temporal region. It originates from a venous plexus on the side of the head and travels laterally from the temporal region over the zygomatic arch, and enters the parotid gland to become the retromandibular vein, where it joins the transverse facial vein.[4][5] The retromandibular vein then drains into the internal jugular vein via its anterior branch and the external jugular vein via its posterior branch. The frontal branch also connects to a parietal emissary vein that runs from the side of the head to the top of the head, where it pierces the cranium and communicates with the superior sagittal sinus.[6] The parietal branch anastomoses with the occipital vein. The parotid and auricular lymph vessels are located both anteriorly and posteriorly of the superficial temporal vein and artery, and the superficial parotid and preauricular lymph nodes located posteriorly drain the area supplied by the branches of the superficial temporal artery.
Posterior Auricular and Occipital Veins
The posterior auricular vein assists with the draining of the muscles and skin of the scalp (see Image. Veins of the Scalp). It originates from small vessels behind the ear superficial to the temporal fascia and anastomoses with the occipital vein superiorly.[7] It runs just behind the ear, where it then confluences with the occipital and deep cervical veins, then receives blood from the posterior branch of the retromandibular vein before turning into the external jugular vein. The posterior auricular vein runs alongside the posterior auricular artery, which originates from the external carotid artery. It is surrounded anteriorly by the mastoid lymph nodes that drain into the parotid and auricular lymph vessels and posteriorly from sternocleidomastoid lymph nodes that drain into the occipital lymph vessels. These lymph vessels then drain into the jugular lymph vessels.
The occipital vein originates from small vessels on the posterior aspect of the scalp and drains the superficial muscles and skin of the occipital region. It is superficial to the occipital fascia and the occipital artery and anastomoses laterally with the parietal branch of the superficial temporal vein and inferolateral to the posterior auricular vein. It then runs into the inferior portion of the posterior auricular vein, where it becomes the external jugular vein. The occipital vein also has an anastomosis with the intracranial confluence of the sinuses via the occipital emissary vein.[8] The occipital lymph nodes and vessels drain lymph from this area and drain into the jugulodigastric lymph node, which drains into the jugular lymph vessels.
Deep Venous Drainage
The venous drainage of the deep scalp layers is via the pterygoid venous plexus, an extensive plexus of veins located between the lateral pterygoid and temporalis muscles, draining into the maxillary vein. It receives branches corresponding with the branches of the maxillary artery.[9] These veins include:
- Alveolar
- Buccinator
- Deep temporal (anterior and posterior)
- Infraorbital
- Masseteric
- Middle meningeal
- Pterygoid
- Sphenopalatine
The pterygoid venous plexus also receives blood from some branches of the palatine veins and contains a communicating vein that travels through the inferior orbital fissure to connect the ophthalmic vein to the cavernous sinus.
Embryology
The scalp veins are derived from the mesoderm of the first and second branchial arches, embryologic structures that form between the fourth and seventh week of gestation. The branchial arches go on to form the blood vessels, bone, cartilage, and muscles of the face, among other structures.[10] The muscles that these veins drain also derive from the first and second branchial arches. Second branchial arch anomalies account for the majority (95%) of branchial arch anomalies, with first branchial arch anomalies accounting for only 1 to 4% of cases.[11]
Nerves
Several nerves are relevant and proximal to the scalp veins, with varying relationships anatomically to these structures.
- The supratrochlear nerve is located medially to the supratrochlear vein, whereas the medial branch of the supraorbital nerve is just deep in the supratrochlear vein.
- The lateral branch of the supraorbital nerve is just medial and deep to the supraorbital vein.
- The temporal branches of the facial nerve are located between the zygomatic orbital vein (a non-scalp vein) inferiorly and the frontal branch of the superficial temporal vein superiorly and posteriorly.
- The auriculotemporal nerve runs just anterior and deep to the superficial temporal artery and vein.
- The posterior auricular artery and vein are sandwiched between the posterior auricular nerve anteriorly and the great auricular nerve just deep and posteroinferiorly.
- Sandwiching the occipital artery and vein are the lesser and greater occipital nerve branches, superficially and anteriorly, and posteriorly, respectively.[12]
Muscles
The scalp veins primarily drain the deoxygenated blood from the epicranial aponeurosis and the frontal and occipital belly of the occipitofrontalis muscle, the temporalis muscle, the auricularis superior muscle, the temporoparietalis muscle, the auricularis anterior muscle, and the auricularis posterior muscles.
Physiologic Variants
The parietal emissary vein most commonly communicates with the superficial temporal vein, specifically the frontal branch, but may communicate with other scalp veins. The occipital emissary vein may not be present in all individuals. The multiple anastomoses of the scalp may also have variability in which branches they interconnect with.[13][14]
Clinical Significance
Deep lacerations to the scalp are inclined to bleed profusely for several reasons.[15] These reasons are as follows:
- Vasoconstriction is prevented due to the close-fitting adherence of the dense connective tissue to the blood vessels.
- The pulling effect of the occipitofrontalis muscle precludes the closing of the actively bleeding vessel and the surrounding skin.
- There are numerous anastomoses of the scalp blood vessels, such as the anastomosis of the occipital and the posterior auricular veins.
Scalp arteriovenous malformations (AVM), or cirsoid aneurysms, are uncommon lesions whose etiologies are most commonly congenital, post-infectious, or traumatic.[16] These AVMs often comprise arterial blood from the superficial temporal or occipital arteries and venous outflow into extracranial venous structures. Treatment of AVMs typically consists of endovascular embolization, followed by surgical resection; therefore, variant arterial supply and venous drainage should be considered in these cases.[17]
Subgaleal hematoma (SGH) is an abnormal collection of blood beneath the galea aponeurosis of the scalp, commonly caused by traumatic shearing of emissary veins in the loose areolar tissue. This condition is more commonly seen in neonates, infants, and small children, although there have been case reports of SGHs occurring in adults.[5] Mild trauma typically occurs via contusion, hair pulling, or vacuum-assisted vaginal delivery. Treatment is typically conservative, principally with bandage compression.[18]
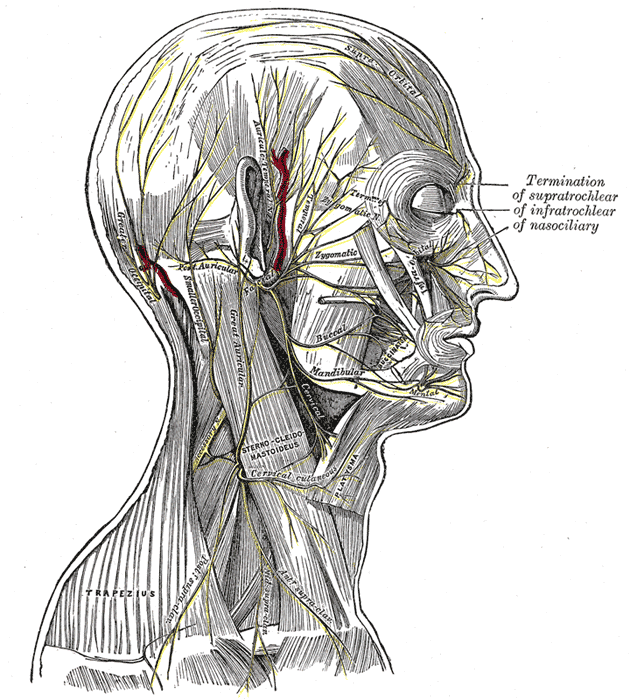
The ‘danger area of the scalp’ refers to the layer of loose areolar connective tissue as it contains the valveless emissary veins that connect the superficial veins in the subaponeurotic space with the intracranial venous sinuses. This connection makes it possible for an infection to spread from the scalp to the meninges. See Image. Relationship of the Meninges to the Skill and Brain.
Cavernous sinus thrombosis is the development of a blood clot within the cavernous sinus. The cavernous sinus is one of the dural venous sinuses, a cavity at the base of the brain that helps drain deoxygenated blood from the brain via the superior and inferior ophthalmic veins, the superficial middle cerebral veins, the sphenoparietal sinus, and the inferior cerebral veins. The cavernous sinus has connections to the pterygoid venous plexus via the inferior ophthalmic vein, deep facial vein, and emissary veins. Due to this connection, superficial facial infections from the nose, sinuses, ears, or teeth may spread to the cavernous sinus to cause this disorder.[19]
Symptoms may include proptosis, unilateral periorbital edema, decrease or loss of vision, headaches, and possible cranial nerve paralysis, particularly of the delicate abducens nerve that runs through the cavernous sinus. There are two types of cavernous sinus thromboses: septic and aseptic. Treatment of septic disease includes initial broad-spectrum IV antibiotics covering staph and strep, the most commonly associated bacteria, then a prolonged course (3 to 4) weeks of targeted IV antibiotics. Surgical drainage may be necessary in cases of sphenoidal sinus infection.[20]
Scalp veins may be used for venous catheterization as they offer easy access with little risk.[21] Most commonly, scalp catheterization is utilized in infants and neonates after unsuccessful attempts at cannulation of extremity veins as the scalp veins in this population have less overlying subcutaneous fat and are more prominent compared to other peripheral sites, and they are less obscured by hair. These factors allow for easier visualization and, therefore, cannulation. The most commonly used veins are the superficial temporal, supratrochlear, and occipital veins.
Media
(Click Image to Enlarge)
Veins in the Skull. Veins in the skull: occipital, posterior temporal, and anterior temporal.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
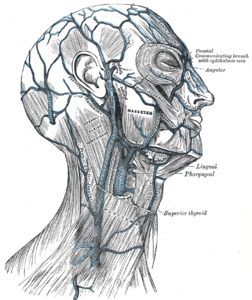
The Anterior Divisions, The Nerves of the Scalp, Face, and Side of the Neck
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
Relationship of the Meniges to the Skull and Brain. This coronal section shows the scalp, subcutaneous tissue, galea aponeurotica, pericranium, cranial bone (skull), dura mater, arachnoid mater, pia mater, superior sagittal sinus, and cerebral falx (not labeled).
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
Veins of the Scalp. Venous drainage of the scalp includes the supratrochlear and supraorbital veins, the temporal veins and their branches, the posterior auricular vein, and the occipital vein and its branches.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Kiliç T, Akakin A. Anatomy of cerebral veins and sinuses. Frontiers of neurology and neuroscience. 2008:23():4-15 [PubMed PMID: 18004050]
Bechmann S, Rahman S, Kashyap V. Anatomy, Head and Neck, External Jugular Veins. StatPearls. 2024 Jan:(): [PubMed PMID: 30855810]
Shimizu Y, Imanishi N, Nakajima T, Nakajima H, Aiso S, Kishi K. Venous architecture of the glabellar to the forehead region. Clinical anatomy (New York, N.Y.). 2013 Mar:26(2):183-95. doi: 10.1002/ca.22143. Epub 2012 Aug 7 [PubMed PMID: 22887451]
Sugahara K,Matsunaga S,Yamamoto M,Noguchi T,Morita S,Koyachi M,Koyama Y,Koyama T,Kasahara N,Abe S,Katakura A, Retromandibular vein position and course patterns in relation to mandible: anatomical morphologies requiring particular vigilance during sagittal split ramus osteotomy. Anatomy [PubMed PMID: 33214345]
Kagaya Y, Arikawa M, Akazawa S. Superficial Temporal Vein and Alternative Middle Temporal Vein as Recipient Veins for Free-flap Reconstruction. Plastic and reconstructive surgery. Global open. 2022 Mar:10(3):e4170. doi: 10.1097/GOX.0000000000004170. Epub 2022 Mar 8 [PubMed PMID: 35284200]
Sharma A Sr, Sharma M. Sinus Pericranii (Parietal and Occipital) With Epicranial Varicosities in a Case of Craniosynostosis. Cureus. 2022 Feb:14(2):e21891. doi: 10.7759/cureus.21891. Epub 2022 Feb 4 [PubMed PMID: 35273853]
Level 3 (low-level) evidenceKobayashi S, Nagase T, Ohmori K. Colour Doppler flow imaging of postauricular arteries and veins. British journal of plastic surgery. 1997 Apr:50(3):172-5 [PubMed PMID: 9176003]
Hedjoudje A,Piveteau A,Gonzalez-Campo C,Moghekar A,Gailloud P,San Millán D, The Occipital Emissary Vein: A Possible Marker for Pseudotumor Cerebri. AJNR. American journal of neuroradiology. 2019 Jun; [PubMed PMID: 31072972]
Chang L, Zixiang Y, Zheming F, Gongbiao L, Zhichun L, Rong Z, Aidong Z, Shuzhan L. Management of pterygoid venous plexus hemorrhage during resection of a large juvenile nasopharyngeal angiofibroma: a review of 27 cases. Ear, nose, & throat journal. 2013 Apr-May:92(4-5):204-8 [PubMed PMID: 23599103]
Level 3 (low-level) evidenceAdams A, Mankad K, Offiah C, Childs L. Branchial cleft anomalies: a pictorial review of embryological development and spectrum of imaging findings. Insights into imaging. 2016 Feb:7(1):69-76. doi: 10.1007/s13244-015-0454-5. Epub 2015 Dec 10 [PubMed PMID: 26661849]
Koeller KK, Alamo L, Adair CF, Smirniotopoulos JG. Congenital cystic masses of the neck: radiologic-pathologic correlation. Radiographics : a review publication of the Radiological Society of North America, Inc. 1999 Jan-Feb:19(1):121-46; quiz 152-3 [PubMed PMID: 9925396]
Kemp WJ 3rd,Tubbs RS,Cohen-Gadol AA, The innervation of the scalp: A comprehensive review including anatomy, pathology, and neurosurgical correlates. Surgical neurology international. 2011; [PubMed PMID: 22276233]
Chen Z, Feng H, Zhu G, Wu N, Lin J. Anomalous intracranial venous drainage associated with basal ganglia calcification. AJNR. American journal of neuroradiology. 2007 Jan:28(1):22-4 [PubMed PMID: 17213417]
Level 3 (low-level) evidenceGulmez Cakmak P, Ufuk F, Yagci AB, Sagtas E, Arslan M. Emissary veins prevalence and evaluation of the relationship between dural venous sinus anatomic variations with posterior fossa emissary veins: MR study. La Radiologia medica. 2019 Jul:124(7):620-627. doi: 10.1007/s11547-019-01010-2. Epub 2019 Mar 2 [PubMed PMID: 30825075]
Yoon J, Puthumana JS, Nam AJ. Management of Scalp Injuries. Oral and maxillofacial surgery clinics of North America. 2021 Aug:33(3):407-416. doi: 10.1016/j.coms.2021.05.001. Epub 2021 Jun 3 [PubMed PMID: 34092461]
Scalp Arteriovenous Malformation (Cirsoid Aneurysm) in Adolescence: Report of 2 Cases and Review of the Literature., Li D,Heiferman DM,Rothstein BD,Syed HR,Shaibani A,Tomita T,, World neurosurgery, 2018 Aug [PubMed PMID: 29864562]
Level 3 (low-level) evidenceMatsushige T, Kiya K, Satoh H, Mizoue T, Kagawa K, Araki H. Arteriovenous malformation of the scalp: case report and review of the literature. Surgical neurology. 2004 Sep:62(3):253-9 [PubMed PMID: 15336874]
Level 3 (low-level) evidenceLee SJ, Kim JK, Kim SJ. The clinical characteristics and prognosis of subgaleal hemorrhage in newborn. Korean journal of pediatrics. 2018 Dec:61(12):387-391. doi: 10.3345/kjp.2018.06800. Epub 2018 Sep 16 [PubMed PMID: 30304906]
Caranfa JT, Yoon MK. Septic cavernous sinus thrombosis: A review. Survey of ophthalmology. 2021 Nov-Dec:66(6):1021-1030. doi: 10.1016/j.survophthal.2021.03.009. Epub 2021 Apr 5 [PubMed PMID: 33831391]
Level 3 (low-level) evidenceMatthew TJH,Hussein A, Atypical Cavernous Sinus Thrombosis: A Diagnosis Challenge and Dilemma. Cureus. 2018 Dec 4; [PubMed PMID: 30761237]
Doyle TD, Anand S, Edens MA. Scalp Catheterization. StatPearls. 2024 Jan:(): [PubMed PMID: 29939633]