Introduction
Lumbar disc herniations (LDH) are a relatively common and early manifestation of degeneration of the lumbar spine. The reported incidence of LDH is 2% ~3% and the prevalence is around 12%.[1][2] Prevalence of 4.8% among men and 2.5% among women above 35 years of age.[2] The most common site of LDH is at L4–L5 and/or L5–S1.[3] Surgery for LDH accounts for the most common indication for performing spinal surgery.[4][5]
The first description of a disc herniation causing sciatica was made as early as 1934.[6] For most patients, the radiculopathy associated with a herniated disc resolves nonoperatively, but for those in whom conservative management fails, surgical interventions can be a consideration.[7][8] Treatment for such disc herniations has understandably evolved considerably as techniques continue to evolve. Chymopapain chemonucleolysis and automated percutaneous discectomy were two such techniques that have now fallen out of favor - chymopapain, for example, due to its risk of transverse myelitis. In the 1970s, the focus of surgical treatment shifted to a less invasive approach with decreased manipulation and trauma to the paraspinal musculature, ligamentum flavum, and affected nerve root.[6]
The first documented experience with the micro-lumbar discectomy (MLD) technique using an operating microscope was in 1977, independently by both Yasargil and Caspar in Europe.[9][10] In 1978, Williams was the first to popularize and publish the technique in the United States.[11] Since then, studies have demonstrated the safety and efficacy of microdiscectomy compared to open discectomy and have published outcomes of decreased morbidity, quicker recovery, shorter hospital length of stay, and no significant difference with regard to long-term reoperation rates.[12][13][14][15][16]
Today, microdiscectomy with its smaller incision, less traumatic approach, and better visualization of the operative field than standard open discectomy is considered the gold standard for removing most lumbar disc herniations. Because of its collinear light and magnification, an operating microscope is preferred; however, magnifying loupes and a headlight may also be used. Most procedures are now done in the outpatient setting.
The major advantage of MLD compared to open/standard (SD) is the minimal trauma to the multifidus and reduced risk of post-operative peridural fibrosis.[2]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Understanding anatomical landmarks is critical. Palpation of bony landmarks, including spinous processes, the sacrum, and iliac crests (usually corresponding to the L4/5 disc level), may guide the start point and trajectory of the surgical approach. Such landmarks may be difficult to palpate as body mass index increases - for these patients; it is especially important to ensure the accuracy of trajectory throughout the approach. Disorientation during the procedure can also occur, especially under the operating microscope.
Lumbosacral Transitional Vertebrae
Beware of transitional anatomy. Low back pain in the presence of a lumbosacral transitional vertebra is referred to as Bertolotti syndrome. L5 may sometimes be “sacralized” (with L5 fused to the sacrum), or S1 may be “lumbarized” (with a well-developed disc seen between S1 and S2). Therefore, it is essential to study preoperative imaging and confirm agreement of the level intraoperatively as the incidence of transitional vertebrae can be as high as 4.6% of the general population.[17]
Nerve Roots
It is important to understand the difference between a traversing and exiting nerve root to characterize the anatomy of a disc herniation better. The location of a disc herniation can determine the surgical approach. Nerve roots exit the spinal canal at the level of the corresponding pedicle (except for those in the cervical spine). For example, the L4 nerve root crosses the L3/4 disc space centrally or traverses and exits the spinal canal beneath the L4 pedicle. It then crosses the L4/5 disc space at its lateral margin. This concept is critical to delineate from where a patient’s symptoms may be arising. A paracentral disc herniation at L4/5 would result in compression of the L5 traversing nerve root, whereas a foraminal disc herniation at the same level would compress the exiting L4 nerve root, possibly both the L4 and L5 nerve roots. A far-lateral disc herniation lies beyond the lateral intervertebral space outside the facet joint.
Indications
Prerequisites prior to surgery:
Detailed history taking and thorough neurological examination:
L5 disc cause step page with pelvic glissading while walking in L5 radiculopathy.S1 causes dragging of the foot along the ground while walking. Detailed dermatomal mapping must be obtained.
Correlation with pertinent radio-imagings:
Radio-imagings include plain and dynamic X-ray; CT, CT myelography or CT discography, MRI, and a spinal teleradiograph. This help to ascertain the presence of LDH, and confirm the level, position, and pattern of the herniated disc (posterolateral/ foraminal/extra-foraminal and extruded vs. sequestrated).[4]
A protrusion is when the height of the hernia is less than the length of the base. Extrusion is when the length of the base is less than the height of the hernia. Sequestration is when there is no continuity between the herniated material and the intervertebral disc.[2]
Patient counseling should encompass:
- Natural history of the disease process-There is a rapid relief of symptoms over a mean period of four to six weeks, with a recurrence of 5 to 10%, regardless of the type of management strategies.[2] Spontaneous resorptions occur in up to 66.66% of cases.[18]
- Different management strategies.
- Different surgical strategies.
- Risk and benefits of surgical management.[4]
The cornerstone of the surgical management of LDH includes:
- Detailed history and neurological examination.
- Good patient selection.
- Proper surgical techniques.[4]
Indication for surgery for LDH includes:
- Cauda equina syndrome
- Refractory and disabling pain despite 6-8 weeks of analgesics
- Progressive or new onset neurological deficits.[4]
Contraindications
Contraindications include concomitant pathologies such as infection or tumor and segmental instability or vertebral fractures in which further fusion or instrumentation would be required. However, some physicians consider spondylolisthesis or segmental instability only a relative contraindication in certain patients, as long as there is appropriate counseling regarding the potential need for further operative fixation if the microdiscectomy does not succeed.
Equipment
-
Standard radiolucent table with Wilson frame (versus Jackson spine flat top table).
-
Fluoroscopy/C-arm to localize level and minimize skin incision.
-
Operative microscope (in from the opposite side of C-arm), or headlight and magnifying loupes.
-
Microdiscectomy set including high-speed drill, Kerrison rongeurs.
-
Bipolar cautery.
Personnel
Standard operating room staff personnel along with one or two surgeons and the anesthesiologist.
Preparation
After the administration of general anesthesia, the patient is positioned prone on a spine frame or designated table. Local anesthesia may be used; however, general anesthesia is preferred to better manage both the airway and hemodynamics. The head is positioned on foam support with orbital and facial cutouts to minimize pressure on the eyes, nose, and mouth while also allowing airway access. The arms are positioned with shoulders at 90 degrees abduction and elbows at 90 degrees flexion with the axillae free of compression to prevent neuropraxia of the brachial plexus. Ensure chest support with padding, so nipples are midline and straight down. The anterior superior iliac spine and knees are positioned on gel pads with slight flexion of the hips and knees. Check to ensure there are no compression on the lateral femoral cutaneous nerve, peroneal and ulnar nerves. Placing the lumbar spine in kyphosis facilitates access by opening the interlaminar space. Ensure the abdomen is free to reduce intra-abdominal pressure, thereby reducing central venous pressure and epidural venous congestion to minimize surgical site bleeding.
Administer prophylactic intravenous antibiotics before skin incision. Fluoroscopic imaging is used for localization and making the most accurate skin incision directed over the appropriate interspace. A spinal needle can be utilized to mark the incision site with image guidance. The skin is prepped in the usual sterile fashion.
Patient preparation and surgical aspects to be taken into consideration can be summarized as:
- OT Safety checklist.
- Sterile theatre environment.
- Antibiotic prophylaxis 30 minutes prior to incision.
- Proper positioning: Genupectoral ensuring free abdomen, chest support, eyes protection, shoulders in 90° abduction, elbows in 90° flexion, and placing the spine in kyphosis to open up the inter-laminar space.
- Localization and exposure- Through surface landmarks and fluoroscopic guidance.
Technique or Treatment
Micro-lumbar discectomy (MLD)
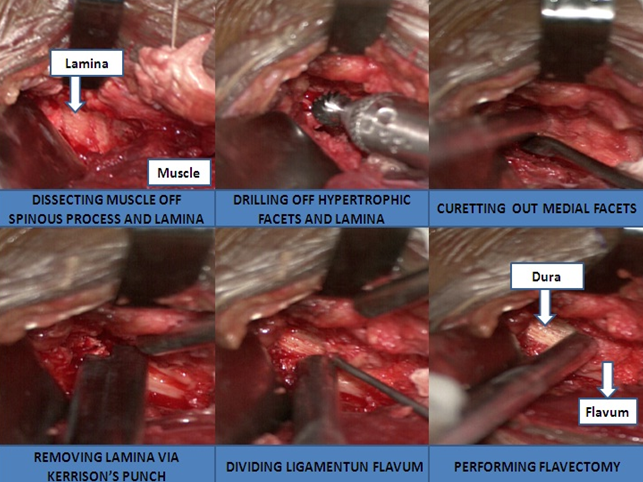
Using intraoperative radiography to confirm the target level, a two to three-centimeter marking for a longitudinal midline incision is made over the interspace. The skin incision is made with a sharp scalpel, and subcutaneous dissection with electrocautery reveals the lumbar fascia over the midline. The muscular aponeurosis is incised just off of the midline on the side of the approach, and the multifidus is released subperiosteally from the spinous process on one side out to the facet joints with a Cobb elevator. The dissection should include half of the lamina both above and below the interspace. Do not violate the facet capsule. At this point, repeat imaging should be performed to confirm the appropriate level. Retractors are introduced to establish the working window, and the microscope is positioned accordingly over the incision. The surgeon can alternately use magnifying loupes.
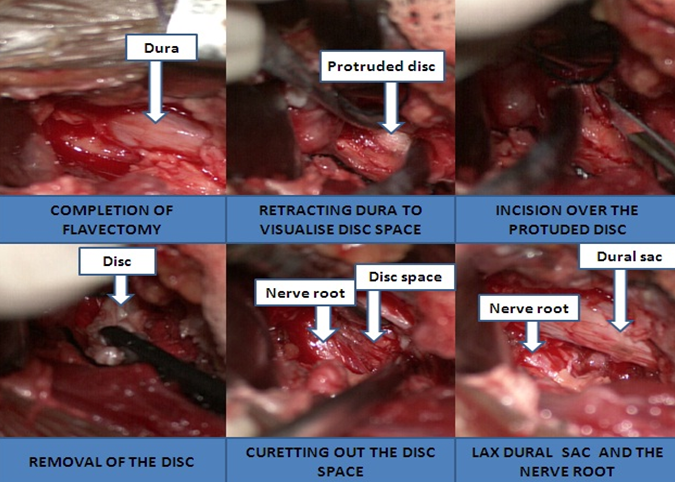
The ligamentum flavum is exposed and released with a curette from its attachment on the anterior aspect of the superior lamina of the inferior vertebra. The ligamentum flavum is then incised sharply to allow for its retraction. An angled Woodson elevator can be used beneath the ligamentum to protect the dura during this incision Retraction of the ligamentum or removal with a Kerrison rongeur should allow for visualization of the exiting nerve root with its associated epidural fat. The nerve root must be identified before proceeding to disc resection. If visualization is inadequate, the medial aspect of the inferior facet of the superior vertebra may need to be removed. To minimize the risk of iatrogenic instability, it is important to preserve at least half of the facet joint and 8 to 12 mm of bone from the lateral edge of decompression to the edge of the pars interarticularis. A laminotomy of the inferior portion of the upper lamina may be necessary if the disc is not centered on the interlaminar space. A blunt ball-tipped probe is inserted into the neuroforamen to mobilize the nerve root, which is then retracted medially with a nerve root retractor. Disc excision can now be performed with the removal of the fragmented or herniated disc tissue.
In some cases, the annulus must be incised to remove a portion of the disc from behind the posterior longitudinal ligament. Up- and down-facing curettes and pituitary rongeurs can be used to perform the discectomy. Care is taken not to violate anteriorly beyond the disc space where major vessels lie, especially when using the microscope. Using a blunt instrument such as a Penfield dissector or a Woodson elevator, freedom of the nerve and dural sac is checked by probing in all directions to check for any remaining disc or ligamentous tissue and confirm an adequate decompression.
Irrigate the disc space with saline via a hollow flexible tube or bulb syringe to express any unrecognized loose disc fragments. Meticulous hemostasis is obtained with bipolar cautery, and the wound is thoroughly irrigated with saline. Vancomycin powder can be applied to the wound before closure. The fascia of the lumbar musculature and subcutaneous layers are closed with absorbable sutures, and the skin is closed according to surgeon preference. Some disc herniations, such as those extending through the foramen, may need to be approached from a combined midline and lateral approach.
Far-lateral Microdiscectomy
The same general steps can be applied but approached through the muscle-splitting technique to avoid the extensive muscle retraction that would be necessary from a midline approach. In this case, an incision is made 3.0 to 6.0 cm off the midline on the side of the affected level. A skin incision is made with a sharp scalpel, and subcutaneous dissection with electrocautery reveals the thoracolumbar fascia. Muscle fibers of the superficial lumbar musculature are split longitudinally. Specifically, the fibers of the multifidus and longissimus muscles are bluntly separated. Self-retaining retractors can now be introduced, and the microscope is positioned over the working window (similarly, the surgeon can proceed instead with the assistance of magnifying loupes). Surgical landmarks are identified, including the pars interarticularis or isthmus, transverse processes, facet joint, and intertransverse ligament. The intertransverse ligament can be detached from the inferior transverse process and retracted laterally. If needed, a Kerrison rongeur or high-speed drill can be used to remove a portion of bone along the superior aspect of the isthmus as well as the inferior portion of the superior transverse process. At this point, the ligamentum flavum is visualized along with the inferior aspect of the pedicle beneath the transverse process. Resect the ligamentum flavum using a Kerrison rongeur for better visualization of the nerve and to avoid injury. The nerve is typically displaced superiorly and laterally by the underlying disc material. Dissect lumbar arteries and veins from the lower foramen when possible and inspect for any further migration of the herniated disc. Carefully examine the foramen for any disc fragments with a blunt nerve hook as the nerve exits inferior to the pedicle. Irrigate and close the wound as detailed above.
Micro-endoscopic discectomy (MED)
The patient is positioned and prepped as described above. A 1.5 to 2.0 cm surgical incision is marked longitudinally 1.5 cm paramedian to the midline on the affected side for paracentral herniations. For extraforaminal or far-lateral disc herniations, the incision is marked 3.0 to 5.0 cm paramedian to the midline. An incision is made with a scalpel to facilitate the blunt muscle-sparing dissection through the serial placement of dilators. The dilators are placed under direct vision with fluoroscopy to ensure appropriate depth and localization and create a working channel. At this point, the microscope can be introduced to the surgical field, or magnifying loupes can be used to aid in visualization. Once the bony exposure of the spine is visible within the tubular retractor, hemilaminectomy and discectomy can be performed as needed, similar to the open exposures detailed above. Once hemostasis is achieved, the tubular retractor system can be removed, and subcutaneous tissue and skin can be closed.
Salient surgical steps can be summarized as: Microdiscectomy for medial, paramedian, and intra-foraminal discs
- This was first described by Caspar.
- There is an integration of a microscope for providing illumination as well as magnification.
- These are approached through a 3 cm paramedian incision (5 mm from the midline on the affected side).
- The dorsolumbar fascia is incised 1cm off the midline on the affected side and the multifidus is released from the spinous process on one side without hampering its insertions.
- The inter-laminar window of the concerned level is reached.
- The speculum is applied and opened.
- Stringent care to preserve the capsular and the interspinous ligament is required.
- The microscope or magnifying goggles is applied.
- The ligamentum flavum is curetted off its attachment and opened laterally.
- The nerve root is exposed and safely mobilized to visualize the disc either in the shoulder or the axilla.
- The posterior ligament is incised and herniated disc is removed.
- Extruded or intra-discal sequestra are removed.
- The adequate decompression of the nerve root and the dural sac is confirmed by passing a ball-tipped non-traumatic hook in all directions.[4]
Extra-Foraminal discs
- This was first described by Wiltse and Spencer.
- A skin incision is made 3 cm and 6 cm lateral to the midline.
- The dorsolumbar fascia is incised in a semicircular manner.
- The inter-transverse plane is approached via a trans-muscular corridor between the multifidus and longissimus.
- The inter-transverse ligament and muscle are then excised lateral to the facet joint, to expose the dorsal root ganglion.
- The ganglion is then securely mobilized to expose the disc.[4]
Foraminal disc
Depending on the extension of the disc, the Wiltse approach or the standard posterior approach can be taken.[4]
In young patients owing to strong paravertebral muscles that share loading with the spinal column, only MLD suffices. In elderly patients with wide-based annulus laxity with disc herniation, microdiscectomy alongside dynamic stabilization and interspinous devices is justified.[19]
Advantages of the MLD compared to SD:
- Magnified surgical view.
- Improved illumination of the surgical field.
- Minimal surgical incision.
- Minimal trauma to paraspinal multifidus muscles.
- Reduced intraoperative blood loss and better hemostasis.
- Reduced risks of intra-operative complications.
- Avoids peridural fibrosis.[2]
- Shortened hospital stay.
- Homogenous improved clinical outcomes with a success rate of 76% and 100%.
- Can be performed as a daycare procedure with patient satisfaction exceeding 80% and an overall success rate of nearly 90%.[20]
- Does not prolong the operative time.
- Does not increase the odds of wrong-level surgeries or missed disc fragments.
Disadvantages:
- Small operating corridor with a compromised field of vision harbingers the risk of neurovascular injury.
- Learning curve.
Complications
Microdiscectomy complications range from iatrogenic injuries such as durotomy, nerve root injury, or instability, to recurrent disc herniations, hematoma, infections, or even other medical complications. Reported complication rates vary. The incidence of durotomy ranges from 0.7% to 4% in the literature but is undoubtedly higher in revision microdiscectomy cases.[6][21][22][23] One large series of 2500 cases of microdiscectomy reported a complication rate of less than 1.5%.[6] A recent systematic review and meta-analysis analyzed the complication rates following several different microdiscectomy approaches. Overall, the published complication rates for open and percutaneous microdiscectomy were 12.5% and 10.8%, respectively. This included intraoperative nerve root injury (2.6% and 1.1%), new or worsening neurologic injury (2.6% and 1.1%), hematoma (0.5% and 0.6%), wound complications including infection, dehiscence, or seroma (2.1% and 0.5%), recurrent disc herniations (4.4% and 3.9%), and reoperation (7.1% and 10.2%). Interestingly, these numbers show the general incidence of different complications, yet no differences were statistically significant between the types of microdiscectomy.[24] Studies show conflicting evidence for risk factors of recurrent lumbar disc herniations regarding sex, age, and body mass index; however, smoking, heavy labor, taller disc height, and the presence of degenerative facet changes seem to be associated with recurrent herniation.[25][26] Other than the risk of recurrent herniation, back pain issues postoperatively can be due to further disc degeneration or facet arthritis leading to segmental instability.
Despite the benefits a microscope can add, many surgeons have been reluctant to adopt its use secondary to concerns regarding a potential increased risk of infection. Studies have confirmed that microscopes and surgical loupes, and headlamps can all be reservoirs of microorganisms.[27][28] One study, in particular, examined cultures of samples taken intraoperatively from the cover of the microscope and the disc space. While 17% of patients had a positive sample from the disc space, and 12% had a positive sample from the microscope, there was only one case of clinically significant infection among the 400 patients who were studied.[28] Microscope use was associated with increased operative time but no significant increased risk of infection.[29]
Complications pertaining to lumbar discectomy can be enumerated as:
Dural tear:
Place a Patti neurosurgical sponge, and extend the laminectomy edges to expose the tear and primary repair with 5/0 non-absorbable suture. Use of biological glue.[30]
A history of epidural steroid injections within 3 months of the surgery has a risk for intraoperative dural injury.[1]
Excessive traction on the nerve while exposing the disc increases the risk of epidural bleeding and CSF leak.[4][31]
Iatrogenic Neuropraxia.[32]
Epidural bleeding:
- Compresses with Patti sponge for venous “lakes”.
- Use of hemostatic agents such as surgical and surgiflow.
Vascular injury:
- The reported incidence is less than 1%.
- Aorta and inferior venacava are at risk in L1-L4, the iliac vessels are at risk at L4-L5 and L5-S1.[33]
- Large vessel injury- may require embolization or laparotomy.
Disc not identified:
- Confirm imaging dates (which should be less than 2 months old).
- Confirm the correct surgical level.
- Extend the surgical corridor.
Failed-back surgery syndrome. A recurrence rate of 3-15% and instability rate of 20% during ten years of follow-up have been observed.[34]
Recurrence.
- The reported incidence of 3% to 15%.[4]
- Most recurrences at the same level of herniation and on the same side.[35]
- In one study Recurrence rate at 5-year follow-up was 6.27% .63% of them occurred within 6 months.
- Modic changes, disc height index (DHI), and facet orientation (FO) showed a significant co-relationship.[36]
- Modic type-II and contained disks had higher odds of recurrence.[37]
- Smoking, disc protrusion, and diabetes are significant predictors of recurrence.[38]
- Obesity is a risk for the occurrence as well as recurrence of LDH.
Reoperation:
- In one study comprising 1850 patients, 130 patients underwent re-operation and were successful in 62%of them. Herniation at different levels, recurrences at the same level, and scar formation showed excellent results in 98%, 54%), and 38% cases respectively.[39]
Postoperative discal pseudo-cyst.[40]
Iliac arteriovenous fistula.[41]
Epidural hematoma.[42]
Retained Non-absorbable Haemostatic Material (RNHM) such as gossypibomas and muslinomas.[43]
Clinical Significance
Microdiscectomy is a safe and effective treatment modality for disc herniations. The landmark study of the Spine Patient Outcomes Research Trial used a large, multicenter, prospective, randomized controlled trial to compare open discectomy with nonoperative management. It has demonstrated that while both treatment groups did achieve good clinical outcomes, patients who underwent discectomy had greater improvement than those who had nonoperative management.[7][8][44][45] A recent Cochrane database systematic review focused on open versus minimally invasive discectomy techniques. It presented low-quality data suggestive of lower infection rates, and shorter hospital stays, but possibly inferior improvements in back and leg pain with the minimally invasive techniques. However, the authors acknowledged that these differences were small and potentially not clinically significant.[46] A more recent systematic review and multiple prospective randomized trials comparing the common techniques for microdiscectomy, both open and tubular, have demonstrated Level 1 evidence to support that both techniques have similar clinical outcomes and complications.[47][48][49][50]
In a survey study among spine surgeons for surgical management of symptomatic LDH:
- 63% preferred MLD
- 53% percent preferred early mobilization (first postoperative day).
- 59% preferred to follow up with patients clinically.[5]
Comparative study between SD, MLD, MED, and fully endoscopic discectomy (FE):
A comparison between SD and MLD-A meta-analysis found no benefit.[4]
Comparison between SD and MED-Mean hospital stay, bleeding, and time to return to work were lower in MED, but long-term pain results were equivalent.[4]
Comparison between MLD and FE-No significant difference in clinical results in terms of pain, complications, or recurrence. Endoscopy and MED only reduced hospital stay and intraoperative bleeding.[4]
In a meta-analysis from 1997 to 2020, SD, MLD, MED, and FE were associated with:
- Recurrence in 4.1%, 5.1%, 3.9% and 3.5%;
- Re-operations in 5.2%, 7.5%, 4.9% and 4%;
- Wound complications in 3.5%, 3.5%, 1.2% and 2%;
- Durotomy in 6.6%, 2.3%, 4.4% and 1.1% ;
- Neurological complications in 1.8%, 2.8%, 4.5% and 4.9% respectively; and
- Nerve root injury in 0.3% for MLD, 0.8% for MED, and 1.2% for FE.[51]
Enhancing Healthcare Team Outcomes
Achieving the best outcomes with a microdiscectomy relies on an interdisciplinary approach. Establishing the correct diagnosis is critical and begins in the primary care setting. Physicians must recognize the signs and symptoms of a painful herniated disc so that they may begin the appropriate workup. Imaging technicians and radiologists are also integral to the diagnostic process, especially with advanced imaging modalities like MRIs. Conservative treatment relies on a combination of physicians and pharmacists to help manage the patient’s pain and prescribe appropriate multimodal medications to minimize opioid utilization. These can include a combination of anti-inflammatory medications, muscle relaxants, antidepressants, or gabapentinoids. It also relies on physical therapists to provide the gold-standard first line of conservative therapy, allowing for successful treatment of most herniated discs without surgery.[7][8] [Level 1] However, when conservative management fails to alleviate a patient’s symptoms or if the symptoms worsen, prompt recognition by healthcare providers is essential.
Nursing, Allied Health, and Interprofessional Team Interventions
A coordinated interdisciplinary approach across the healthcare professions is integral to a successful microdiscectomy. From the proper patient selection, diagnostic workup, and referrals to the exhaustion of conservative management, primary care practitioners, specialty-trained nurses, physicians such as those who provide epidural steroid injections, and physical therapists are all critical aspects in patient care and not just spine surgeons.
Nursing, Allied Health, and Interprofessional Team Monitoring
Assessing the need for and performing a discectomy requires an interprofessional team approach, including physicians, specialists, specialty-trained nurses, therapists, and pharmacists, all collaborating across disciplines to achieve optimal patient results. [Level 5]
A proper surgical indication is the mainstay of the surgical management of LDH. The nuisances in the pertinent surgical technique must be mastered.[4]
Media
References
Shakya A, Sharma A, Singh V, Rathore A, Garje V, Wadgave V, Kakadiya G, Marathe N. Preoperative Lumbar Epidural Steroid Injection Increases the Risk of a Dural Tear During Minimally Invasive Lumbar Discectomy. International journal of spine surgery. 2022 Jun:16(3):505-511. doi: 10.14444/8249. Epub [PubMed PMID: 35772973]
Vialle LR,Vialle EN,Suárez Henao JE,Giraldo G, LUMBAR DISC HERNIATION. Revista brasileira de ortopedia. 2010 Jan; [PubMed PMID: 27019834]
Ma D, Liang Y, Wang D, Liu Z, Zhang W, Ma T, Zhang L, Lu X, Cai Z. Trend of the incidence of lumbar disc herniation: decreasing with aging in the elderly. Clinical interventions in aging. 2013:8():1047-50. doi: 10.2147/CIA.S49698. Epub 2013 Aug 7 [PubMed PMID: 23966775]
Level 2 (mid-level) evidenceBlamoutier A, Surgical discectomy for lumbar disc herniation: surgical techniques. Orthopaedics [PubMed PMID: 23352565]
Gopal VV. Degenerative Lumbar Disc Disease: A Questionnaire Survey of Management Practice in India and Review of Literature. Journal of neurosciences in rural practice. 2021 Jan:12(1):159-164. doi: 10.1055/s-0040-1722103. Epub 2021 Jan 29 [PubMed PMID: 33531776]
Level 3 (low-level) evidenceKoebbe CJ,Maroon JC,Abla A,El-Kadi H,Bost J, Lumbar microdiscectomy: a historical perspective and current technical considerations. Neurosurgical focus. 2002 Aug 15; [PubMed PMID: 15916400]
Level 3 (low-level) evidenceWeinstein JN,Tosteson TD,Lurie JD,Tosteson AN,Hanscom B,Skinner JS,Abdu WA,Hilibrand AS,Boden SD,Deyo RA, Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006 Nov 22; [PubMed PMID: 17119140]
Level 1 (high-level) evidenceWeinstein JN,Lurie JD,Tosteson TD,Skinner JS,Hanscom B,Tosteson AN,Herkowitz H,Fischgrund J,Cammisa FP,Albert T,Deyo RA, Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006 Nov 22; [PubMed PMID: 17119141]
Level 2 (mid-level) evidencePostacchini F,Postacchini R, Operative management of lumbar disc herniation : the evolution of knowledge and surgical techniques in the last century. Acta neurochirurgica. Supplement. 2011; [PubMed PMID: 21107933]
Caspar W,Campbell B,Barbier DD,Kretschmmer R,Gotfried Y, The Caspar microsurgical discectomy and comparison with a conventional standard lumbar disc procedure. Neurosurgery. 1991 Jan; [PubMed PMID: 1994285]
Level 2 (mid-level) evidenceWilliams RW, Microlumbar discectomy: a conservative surgical approach to the virgin herniated lumbar disc. Spine. 1978 Jun; [PubMed PMID: 663769]
Calikoglu C,Cakir M, Open Discectomy vs. Microdiscectomy: Results from 519 Patients Operated for Lumbar Disc Herniation. The Eurasian journal of medicine. 2018 Oct; [PubMed PMID: 30515039]
Kahanovitz N,Viola K,Muculloch J, Limited surgical discectomy and microdiscectomy. A clinical comparison. Spine. 1989 Jan; [PubMed PMID: 2913673]
Vucetic N,de Bri E,Svensson O, Clinical history in lumbar disc herniation. A prospective study in 160 patients. Acta orthopaedica Scandinavica. 1997 Apr; [PubMed PMID: 9174445]
Katayama Y,Matsuyama Y,Yoshihara H,Sakai Y,Nakamura H,Nakashima S,Ito Z,Ishiguro N, Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon. Journal of spinal disorders [PubMed PMID: 16826006]
Level 1 (high-level) evidenceWeber H, Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine. 1983 Mar; [PubMed PMID: 6857385]
Level 1 (high-level) evidenceQuinlan JF,Duke D,Eustace S, Bertolotti's syndrome. A cause of back pain in young people. The Journal of bone and joint surgery. British volume. 2006 Sep; [PubMed PMID: 16943469]
Zhong M, Liu JT, Jiang H, Mo W, Yu PF, Li XC, Xue RR. Incidence of Spontaneous Resorption of Lumbar Disc Herniation: A Meta-Analysis. Pain physician. 2017 Jan-Feb:20(1):E45-E52 [PubMed PMID: 28072796]
Level 1 (high-level) evidencePlasencia Arriba MÁ,Maestre C,Martín-Gorroño F,Plasencia P, Analysis of Long-Term Results of Lumbar Discectomy With and Without an Interspinous Device. International journal of spine surgery. 2022 Jul 31; [PubMed PMID: 35908809]
Jaiswal A,Kumar S,Reddy S,Jaiswal P, Feasibility and Safety of Outpatient Lumbar Microscopic Discectomy in a Developing Country. Asian spine journal. 2019 Oct; [PubMed PMID: 31154705]
Level 2 (mid-level) evidenceDesai A,Ball PA,Bekelis K,Lurie JD,Mirza SK,Tosteson TD,Weinstein JN, Outcomes after incidental durotomy during first-time lumbar discectomy. Journal of neurosurgery. Spine. 2011 May; [PubMed PMID: 21375385]
Vangen-Lønne V,Madsbu MA,Salvesen Ø,Nygaard ØP,Solberg TK,Gulati S, Microdiscectomy for Lumbar Disc Herniation: A Single-Center Observational Study. World neurosurgery. 2020 Feb 17; [PubMed PMID: 32081830]
Level 2 (mid-level) evidenceKogias E,Klingler JH,Franco Jimenez P,Vasilikos I,Sircar R,Scholz C,Hubbe U, Incidental Durotomy in Open Versus Tubular Revision Microdiscectomy: A Retrospective Controlled Study on Incidence, Management, and Outcome. Clinical spine surgery. 2017 Dec; [PubMed PMID: 29176490]
Level 2 (mid-level) evidenceShriver MF,Xie JJ,Tye EY,Rosenbaum BP,Kshettry VR,Benzel EC,Mroz TE, Lumbar microdiscectomy complication rates: a systematic review and meta-analysis. Neurosurgical focus. 2015 Oct; [PubMed PMID: 26424346]
Level 1 (high-level) evidenceShimia M,Babaei-Ghazani A,Sadat BE,Habibi B,Habibzadeh A, Risk factors of recurrent lumbar disk herniation. Asian journal of neurosurgery. 2013 Apr; [PubMed PMID: 24049552]
Camino Willhuber G,Kido G,Mereles M,Bassani J,Petracchi M,Elizondo C,Gruenberg M,Sola C, Factors associated with lumbar disc hernia recurrence after microdiscectomy. Revista espanola de cirugia ortopedica y traumatologia. 2017 Nov - Dec; [PubMed PMID: 28899699]
Weiner BK,Kilgore WB, Bacterial shedding in common spine surgical procedures: headlamp/loupes and the operative microscope. Spine. 2007 Apr 15; [PubMed PMID: 17426639]
Tronnier V,Schneider R,Kunz U,Albert F,Oldenkott P, Postoperative spondylodiscitis: results of a prospective study about the aetiology of spondylodiscitis after operation for lumbar disc herniation. Acta neurochirurgica. 1992; [PubMed PMID: 1414515]
Basques BA,Golinvaux NS,Bohl DD,Yacob A,Toy JO,Varthi AG,Grauer JN, Use of an operating microscope during spine surgery is associated with minor increases in operating room times and no increased risk of infection. Spine. 2014 Oct 15; [PubMed PMID: 25188600]
Level 2 (mid-level) evidenceTsitsopoulos PP. Accidental dural tear in lumbar spine surgery. Acta neurochirurgica. 2022 Jul:164(7):1889-1890. doi: 10.1007/s00701-022-05262-2. Epub 2022 Jun 1 [PubMed PMID: 35648214]
Charalambous LT, Rajkumar S, Liu B, Adil SM, Wong M, Hodges S, Amrhein TJ, Leithe LG, Parente B, Lee HJ, Lad SP. Treatment Patterns and Health Care Resource Utilization of Iatrogenic Spinal Cerebrospinal Fluid Leaks in the United States. Clinical spine surgery. 2022 Nov 1:35(9):E725-E730. doi: 10.1097/BSD.0000000000001363. Epub 2022 Jul 14 [PubMed PMID: 35858207]
Asan Z. Early Postoperative Iatrogenic Neuropraxia After Lumbar Disc Herniation Surgery: Analysis of 87 Cases. World neurosurgery. 2023 Feb:170():e801-e805. doi: 10.1016/j.wneu.2022.11.128. Epub 2022 Nov 30 [PubMed PMID: 36460197]
Level 3 (low-level) evidenceHasan GA, Qatran Raheem H, Yuser A, Al-Naser LM, Sheta RA. Vascular injury in tubular lumbar microdiscectomy, case report and literature review. SAGE open medical case reports. 2019:7():2050313X19851695. doi: 10.1177/2050313X19851695. Epub 2019 May 26 [PubMed PMID: 31205717]
Level 3 (low-level) evidenceOrhurhu VJ, Chu R, Gill J. Failed Back Surgery Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 30969599]
Mariscal G, Torres E, Barrios C. Incidence of recurrent lumbar disc herniation: A narrative review. Journal of craniovertebral junction & spine. 2022 Apr-Jun:13(2):110-113. doi: 10.4103/jcvjs.jcvjs_38_22. Epub 2022 Jun 13 [PubMed PMID: 35837428]
Level 3 (low-level) evidenceGuo J, Li G, Ji X, Wu X, Zhang G, Zhou C, Ma X. Clinical and Radiological Risk Factors of Early Recurrent Lumbar Disc Herniation at Six Months or Less: A Clinical Retrospective Analysis in One Medical Center. Pain physician. 2022 Oct:25(7):E1039-E1045 [PubMed PMID: 36288589]
Level 2 (mid-level) evidenceAbdallah A, Güler Abdallah B. Factors associated with the recurrence of lumbar disk herniation: non-biomechanical-radiological and intraoperative factors. Neurological research. 2023 Jan:45(1):11-27. doi: 10.1080/01616412.2022.2116525. Epub 2022 Sep 1 [PubMed PMID: 36047564]
Huang W, Han Z, Liu J, Yu L, Yu X. Risk Factors for Recurrent Lumbar Disc Herniation: A Systematic Review and Meta-Analysis. Medicine. 2016 Jan:95(2):e2378. doi: 10.1097/MD.0000000000002378. Epub [PubMed PMID: 26765413]
Level 1 (high-level) evidenceFandiño J, Botana C, Viladrich A, Gomez-Bueno J. Reoperation after lumbar disc surgery: results in 130 cases. Acta neurochirurgica. 1993:122(1-2):102-4 [PubMed PMID: 8333299]
Level 2 (mid-level) evidenceWang H, Wang S, Yu H, Chen Y, Zheng L, Ma J. Surgical treatment of recurrent postoperative discal pseudocyst: A case report and literature review. Medicine. 2022 Nov 11:101(45):e31756. doi: 10.1097/MD.0000000000031756. Epub [PubMed PMID: 36397328]
Level 3 (low-level) evidenceNaouli H, Jiber H, Bouarhroum A. Iliac arteriovenous fistula following lumbar disc surgery. A case report. Journal de medecine vasculaire. 2022 Oct:47(4):199-202. doi: 10.1016/j.jdmv.2022.09.004. Epub 2022 Oct 23 [PubMed PMID: 36344032]
Level 3 (low-level) evidenceWu S, Bu W, Wu D, Du J. Spontaneous absorption of lumbar epidural hematoma after percutaneous endoscopic lumbar discectomy in a patient with lumbar disc herniation. Asian journal of surgery. 2023 Feb:46(2):880-881. doi: 10.1016/j.asjsur.2022.07.067. Epub 2022 Aug 8 [PubMed PMID: 35953362]
Shyam K, Bhari Thippeswamy P, Shetty AP, Algeri R, Rajasekaran S. Gauze for concern: A Case Report and systematic review of delayed presentation of paraspinal textiloma. Journal of clinical orthopaedics and trauma. 2022 Sep:32():101967. doi: 10.1016/j.jcot.2022.101967. Epub 2022 Aug 14 [PubMed PMID: 36051862]
Level 3 (low-level) evidenceWeinstein JN,Lurie JD,Tosteson TD,Tosteson AN,Blood EA,Abdu WA,Herkowitz H,Hilibrand A,Albert T,Fischgrund J, Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine. 2008 Dec 1; [PubMed PMID: 19018250]
Level 2 (mid-level) evidenceLurie JD,Tosteson TD,Tosteson AN,Zhao W,Morgan TS,Abdu WA,Herkowitz H,Weinstein JN, Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial. Spine. 2014 Jan 1; [PubMed PMID: 24153171]
Level 1 (high-level) evidenceRasouli MR,Rahimi-Movaghar V,Shokraneh F,Moradi-Lakeh M,Chou R, Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. The Cochrane database of systematic reviews. 2014 Sep 4; [PubMed PMID: 25184502]
Level 1 (high-level) evidenceClark AJ,Safaee MM,Khan NR,Brown MT,Foley KT, Tubular microdiscectomy: techniques, complication avoidance, and review of the literature. Neurosurgical focus. 2017 Aug; [PubMed PMID: 28760036]
Arts MP,Brand R,van den Akker ME,Koes BW,Bartels RH,Peul WC, Tubular diskectomy vs conventional microdiskectomy for sciatica: a randomized controlled trial. JAMA. 2009 Jul 8; [PubMed PMID: 19584344]
Level 1 (high-level) evidenceLee P,Liu JC,Fessler RG, Perioperative results following open and minimally invasive single-level lumbar discectomy. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2011 Dec; [PubMed PMID: 21944927]
Level 2 (mid-level) evidenceLau D,Han SJ,Lee JG,Lu DC,Chou D, Minimally invasive compared to open microdiscectomy for lumbar disc herniation. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2011 Jan; [PubMed PMID: 20851604]
Level 2 (mid-level) evidenceBombieri FF, Shafafy R, Elsayed S. Complications associated with lumbar discectomy surgical techniques: a systematic review. Journal of spine surgery (Hong Kong). 2022 Sep:8(3):377-389. doi: 10.21037/jss-21-59. Epub [PubMed PMID: 36285095]
Level 1 (high-level) evidence