Introduction
Foot ulceration is among the most common health issues, and its prevalence has increased recently. It is 1 of the major causes of amputations, particularly in patients with uncontrolled diabetes (see Image. Diabetic Foot Ulcer). The lifetime risk of developing a foot ulcer in patients with diabetes is more than 33%.[1] Diabetic foot ulcer causes a lot of morbidities and accounts for approximately two-thirds of all United States non-traumatic amputations.[2][3][4] Infections in these patients are thought to be limb-threatening conditions.[4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Simultaneous action of multiple contributing factors such as peripheral vascular disease, neuropathy, biomechanical structural deformities, and soft tissue changes is behind the formation and progression of foot ulcerations.[1] Vasculopathy consists of both macro and microvascular processes. Cardiovascular, cerebrovascular, and peripheral vascular or arterial disorders are among the macrovascular, and arterioles and capillaries dysfunctions are the microvascular processes. Peripheral arterial disease (PAD) commonly affects the peroneal and tibial arteries. The atherosclerotic plaque begins to expand within the vessel walls, and the occlusion facilitates the healing of ulceration. Diabetes, smoking, hypertension, and hyperlipidemia can contribute to PAD, leading to an increased risk of ulceration. Patients with diabetes mellitus and PAD are at a higher risk of lower extremity amputations. Hyperglycemia is associated with increased thromboxane A2, a platelet aggregating factor and vasoconstrictor; this increase can lead to a hypercoagulable state and occlusion.[5]
As the capillary size decreases, an increase in vascular permeability and an impairment in the local blood flow regulations alter the microvasculature in patients with diabetes mellitus. Endothelial dysfunction is thought to be the leading cause of changes in the microvascular system. Endogenous nitric oxide causes dilatation of both arteries and veins at the microvascular level by regulating the vascular tone. Vasoconstriction and hypertension occur as the level of nitric oxide decreases. Lower responsiveness of patients with diabetes to nitric oxide puts them at a higher risk of increased vasoconstriction and, subsequently, ulceration due to a lack of adequate nutrients and oxygen for healing.
Peripheral neuropathy is a progressive loss of peripheral nerve fibers, including the sensory, motor, and autonomic fibers. It can progress to a complete sensation loss, typically beginning distally at the toes and advancing proximally with a stocking and glove pattern. Patients are not aware of minor traumas at advanced levels of peripheral neuropathy. Motor neuropathy causes a muscle imbalance, leading to increased pressure and a tissue breakdown in certain weight-bearing areas. Autonomic neuropathy causes a decreased supply of nutrients and oxygen to the foot's soft tissues by shunting the arterial blood flow away from the nutrient capillaries. Hyperglycemia is the leading cause of neuropathy in patients with diabetes mellitus. Nitric oxide has also been demonstrated to be decreased in diabetic patients with peripheral neuropathy. Osseous deformities of the foot play an important role in the development and chronicity of foot ulcers. Structural deformities such as hallux valgus, hammertoes, equinus, hallux limitus, and Charcot foot can increase pressure and, thus, ulcerations. A decreased soft tissue density and fat pad atrophy can also predispose patients to lower extremity ulcerations.
Epidemiology
Foot ulceration is a worldwide health-related issue, and its prevalence has increased due to an increase in diabetes. The estimation of global foot ulceration prevalence is more than 6%, which is thought to be higher in males.[6] Ulceration was noted to be more common in patients with type-2 diabetes mellitus versus patients with type-1 diabetes mellitus. Most patients with foot ulcerations were older, had diabetes for a longer duration, and had comorbidities, including hypertension, diabetic retinopathy, higher body mass index, and positive smoking history.
History and Physical
The patient's medical, surgical, and social history, allergies, and current medications should be obtained from the patient. A complete assessment of the ulcer and its surrounding tissue is crucial. Serial wound measurements, biopsy, and cultures are essential for quantitative wound evaluation. Qualitative evaluations include visual appearance and odor.[7] A fruity smell, for instance, is associated with pseudomonas infection. In the visual assessment of the wound, we look for any possible erythema, edema, fluid discharges, crepitations, or abscess collections. Inspect wound edges for any possible formation of hyperkeratotic tissues, which tends to halt tissue healing. A hyperkeratotic border results from increased stress on the tissue; therefore, the focal pressure should be evaluated. Debridement of hyperkeratotic tissue, which can entrap fluid, is essential to improve wound healing.[7]
Necrotic-base ulcers are black and are non-viable, indicating a peripheral arterial disease or an infection. Fibrotic-base ulcers have a white to yellowish stringy appearance and tend to halt the granulation tissue formation. Granular-base ulcers have a beefy red appearance and indicate a positive healing potential. Wound tracking into sinus tracks should be bluntly probed as it can indicate a deeper infection.[7] Quantitative measurements should be checked at every clinic visit. Comparing the wound dimensions, including the width, length, and depth over time, allows for evaluating the wound contracture. Ulceration discharge cultures can be obtained to target antibiotic therapy in the presence of an infection. A biopsy is performed to rule out any malignant changes in long-standing ulcers.[7]
Evaluation
Ulcer infection should be treated to prompt wound healing. Soft-tissue infections can be examined clinically. Classic clinical signs of an infection are pain, swelling, heat, redness, and loss of function. Systemic symptoms include fever, nausea, vomiting, diarrhea, and chills. Laboratory work for cellulitis should include creatinine, bicarbonate, comprehensive metabolic panel, erythrocyte sedimentation rate, C-reactive protein, and complete blood count with differential. Radiographic evaluation is also essential in the overall management of ulcers. X-rays can assist in osteomyelitis assessment or detecting gas gangrene. MR Images are useful in assessing deeper abscess collections and making definitive diagnoses. CT and bone scans can occasionally be used to visualize bony alterations.[8]
A proper evaluation of the vascular system must be addressed, along with wound care. A clinical vascular assessment includes evaluating the temperature, skin color, skin atrophy, hair distribution, and palpation of pedal pulses, including the posterior tibialis and dorsalis pedis arteries.[8] Doppler ultrasonography is useful in evaluating non-palpable pedal pulses. Ankle-brachial index is also good for assessing peripheral arterial flow. An ankle-brachial index of 0.91 to 1.30 is normal, 0.71 to 0.90 indicates a mild PAD, 0.41 to 0.70 indicates a moderate PAD, and 0.4 or less is considered severe.[9] A magnetic resonance angiography (MRA), arterial duplex ultrasound, or arteriogram can be performed to assess the level and area of vascular occlusion. Clinically, arterial ulcers are painful and develop on the distal extremity. Alternatively, diabetic ulcers tend to be pain-free due to neuropathy and occur on weight-bearing surfaces. Electromyography, along with a nerve conduction velocity test, can be performed to assess peripheral neuropathy.
Radiographic Imaging is essential to rule out the structural deformities in ulcers. A plantar pressure measuring device can detect the peak pressures at specific locations and can be used to identify any underlying bony deformities. Evaluating and treating all 3 imaging modalities is crucial since any bony deformities in the foot and a PAD or neuropathy can place a patient at an increased risk of ulcer formation.
Treatment / Management
There are a variety of treatment options for ulcerations. Chronic non-healing ulcers are typically treated with debridement.[10] This can be done surgically, enzymatically, mechanically, or biologically. Mechanical debridement can be performed using a wet-to-dry dressing, allowing the non-viable tissues to be removed when changing the dressing.[11] Enzymatic debridement is typically done by the application of collagenase, which helps in the breakdown of collagen.[11] In surgical debridement, sharp instruments like blades physically remove the fibrotic and necrotic non-viable tissues. Offloading to lower the abnormal peak pressures is integral to the healing process.[10] Extra-depth shoes with insoles and accommodative and functional devices can decrease abnormal pressures.[12] Non-weight bearing using a wheelchair, crutches, or total contact cast is another offloading approach.[12](A1)
Bioengineered tissues can also be used as alternatives for ulcer closure.[10] These living tissues stimulate wound healing and deliver the growth factors to the site of ulceration. Dermoinductive grafts such as allografts and commercially available products contain living keratinocytes, which allow for the recruitment and activation of the wound bed tissues.[13] Dermoconductive grafts serve as scaffold matrices at the wound site, allowing for wound closure.[14] Topical platelet-rich plasma and other blood products can also heal wounds.[15] Debridement, infection control, removal of bony prominences, and offloading are necessary preparations for the wound to apply blood products and grafts. Negative pressure wound therapy is a primary wound-closure method that can also be used to prepare the wound bed before other treatment modalities and is helpful for acute and chronic ulcers.[10] It helps decrease the bacterial bioburden and increases the granulation tissue and capillary budding at the base of the ulcer.[16] A combination therapy involving negative pressure wound therapy and a split-thickness skin graft is another option for wound closure.(A1)
Hyperbaric oxygen therapy is thought to be an effective treatment method in conjunction with local wound care, like offloading and debridement.[10] Hyperbaric oxygen therapy involves 100% pure oxygen inhaled inside an airtight chamber.[16] The surgical treatment options for non-healing ulcers are Targeting the underlying structural deformity and procedures like tendon-lengthening, exostectomy of bony prominence, or reconstruction. See Image. Jodhpur Technique. Peripheral neuropathy contributes significantly to the development of ulcers, and proper wound care and management are vital for the treatment. Nitric oxide plays a crucial role in peripheral vasculitic neuropathies, and its induction is essential in ulcer management.[17] Using monochromatic near-infrared photo energy therapy can induce the release of nitric oxide, increasing blood flow to the local peripheral nerves. Topical nitric oxide can be used for painful peripheral neuropathies as well.[17] Supplements such as B6, B12, and folate are also used in managing peripheral neuropathies, and oral medications like tricyclic antidepressants, selective serotonin reuptake inhibitors, and antiarrhythmics can be used for symptomatic management of these conditions.
Differential Diagnosis
Foot ulcer differential diagnoses include malignancies like squamous cell carcinoma, basal cell carcinoma, melanoma, Kaposi sarcoma, lymphoproliferative malignancies, and primary skin disorders like sarcoidosis, necrobiosis lipoidica, bullous diseases, and pyoderma gangrenosum.[18]
Staging
Many classification systems have been developed to stage ulcerations for more efficient evaluation and treatment. The 2 leading classifications are the Wagner, Meggitt, and University of Texas ulcer classification systems.[19] The Wagner and Meggitt classification is based on the depth of the ulcer. In contrast, the University of Texas ulcer classification system is based on depth in combination with the presence of ischemia and infection.[19] In the Wagner and Meggitt classification, grade 0 has intact skin with a hyperkeratotic lesion or bony deformity. Grade 1 has a superficial necrotic or viable base ulcer with granulation tissue. Grade 2 extends to deeper structures like the bone, ligament, tendon, or deep fascia with no osteomyelitis or abscess. Grade 3 has osteomyelitis or deep abscess. Grade 4 has gangrenous forefoot changes, and grade 5 indicates a complete foot involvement with no healing.[19]
The University of Texas classification includes 4 grades (0-3) and 4 stages (A-D). Grade 0 stage A is a pre-or post-ulcerative lesion completely epithelialized (non-ischemic, non-infected), stage B indicates infection, stage C indicates ischemia, and stage D indicates both. Grade 1 stage A is a superficial wound without tendon, capsule, or bone involvement (non-ischemic, non-infected), stage B indicates infection, stage C indicates ischemia, and stage D indicates both. Grade 2 is a capsule- or tendon-penetrating wound (non-ischemic, non-infected); stage B indicates infection, stage C indicates ischemia and stage D indicates both. Grade 3 is a bone- or joint-penetrating wound (non-ischemic, non-infected), stage B indicates infection, stage C indicates ischemia, and stage D indicates both.[19]
Prognosis
The prognosis depends on many variants, including the patient's comorbidities and utilized treatment modalities. The overall clinical outcomes of infected foot ulcers are poor, with a 17% lower limb amputation rate and a 15% death rate in 1 year.[20] Approximately 44% of the patient's ulcers heal within a year.[20] Healing is smoother without multiple or chronic foot ulcers and limb ischemia.[20] The ulceration prognosis can be improved by strictly adhering to the treatment plan and controlling the patient's cholesterol and glucose levels.
Complications
Foot ulceration in patients with diabetes is the leading cause of non-traumatic lower-limb amputations.[21] Approximately 35.4% of hospitalized patients with diabetes with foot ulcers undergo lower extremity amputation.[22] The common predictors of lower extremity amputation are ulcer duration, wound infection, Wagner grade 4 or higher, peripheral arterial disease, proteinuria, osteomyelitis, and leukocytosis.
Deterrence and Patient Education
Since most foot ulcer management is done as an outpatient, where the patient must continue a proper level of care outside of a clinical setting, patient education plays a crucial role in managing these patients' conditions. Patients should receive help with daily changes in dressing. The patient should receive educational materials on the importance of keeping the dressing dry, clean, intact, and ambulating with proper assistive devices such as a CAM walker, surgical shoe, crutches, and canes.
Enhancing Healthcare Team Outcomes
An interprofessional team is required to manage patients with foot ulcers for successful healing. Diabetologists, diabetes nurses, orthopedists, vascular surgeons, general surgeons, orthopedic surgeons, interventional radiologists, podiatrists, orthotists, radiology coordinators, microbiologists, shoemakers, psychologists, nurse educators, and rehabilitation teams all work together to provide interdisciplinary foot care in foot specialized centers.[23] The team's full effort is warranted in the foot ulcer healing process. Different interdisciplinary management approaches have been developed to decrease the risk of foot ulcers.[24] All interprofessional team members must keep meticulous records of every patient encounter, record progress or lack thereof, and contact other team members as appropriate to ensure optimal patient care, leading to the best possible outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
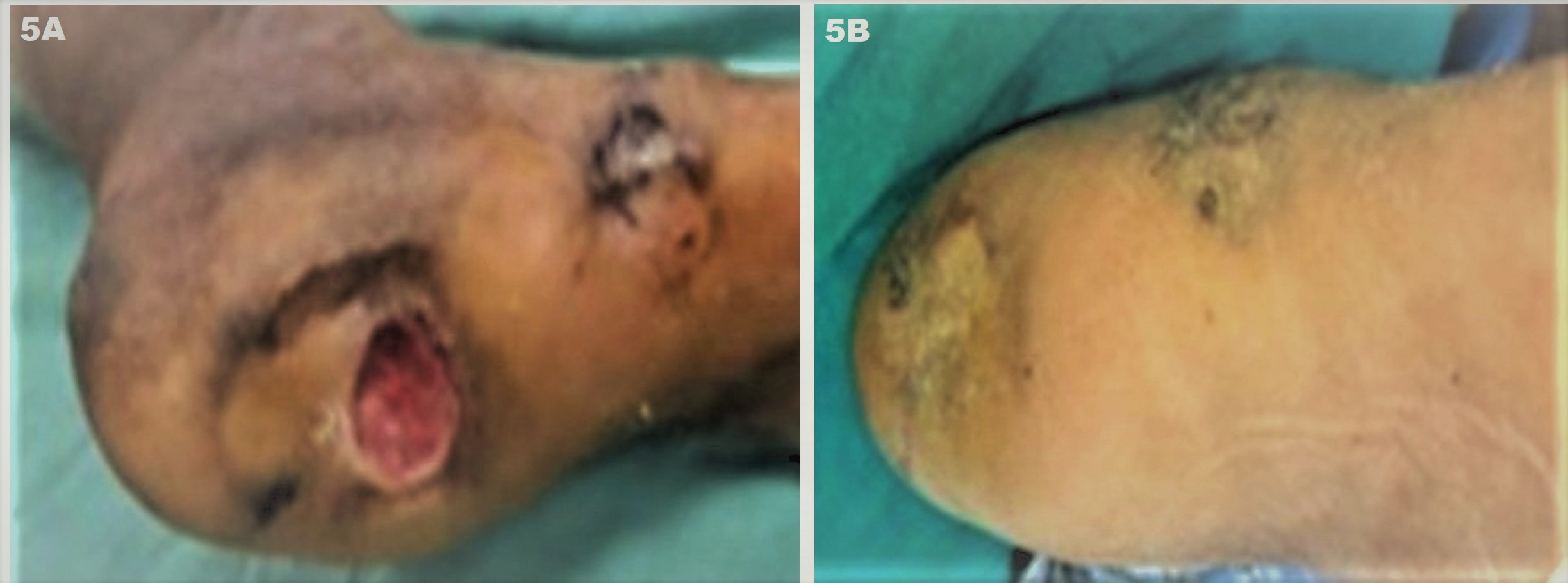
Jodhpur Technique. Depiction of success of the technique in a non-healing foot ulcer of a patient with diabetes with diabetic foot (diabetes controlled with HbA1C < 6.5 X one year). (A) Baseline multiple ulcers over the foot involving the heel and medial malleolus (pressure sites). The lesions are chronic non-healing ulcers (CNHUs) as they failed to heal despite multiple treatment sessions using collagen dressings, platelet-rich fibrin matrix (PRFM), hyperbaric oxygen as well as one flap transplant that necrosed within 4 weeks; and (B) Complete healing of ulcers can be appreciated after 3 months of 2 sessions of JT performed 1 month apart.
Contributed by D Kachhawa, MD, and S Sonthalia, MD, DNB, MNAMS
References
Boulton AJ, Armstrong DG, Albert SF, Frykberg RG, Hellman R, Kirkman MS, Lavery LA, Lemaster JW, Mills JL Sr, Mueller MJ, Sheehan P, Wukich DK, American Diabetes Association, American Association of Clinical Endocrinologists. Comprehensive foot examination and risk assessment: a report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes care. 2008 Aug:31(8):1679-85. doi: 10.2337/dc08-9021. Epub [PubMed PMID: 18663232]
Ramsey SD, Newton K, Blough D, McCulloch DK, Sandhu N, Reiber GE, Wagner EH. Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes care. 1999 Mar:22(3):382-7 [PubMed PMID: 10097914]
Level 2 (mid-level) evidenceGregg EW, Sorlie P, Paulose-Ram R, Gu Q, Eberhardt MS, Wolz M, Burt V, Curtin L, Engelgau M, Geiss L, 1999-2000 national health and nutrition examination survey. Prevalence of lower-extremity disease in the US adult population }=40 years of age with and without diabetes: 1999-2000 national health and nutrition examination survey. Diabetes care. 2004 Jul:27(7):1591-7 [PubMed PMID: 15220233]
Level 3 (low-level) evidencePendsey SP. Understanding diabetic foot. International journal of diabetes in developing countries. 2010 Apr:30(2):75-9. doi: 10.4103/0973-3930.62596. Epub [PubMed PMID: 20535310]
Level 3 (low-level) evidenceIkem R, Ikem I, Adebayo O, Soyoye D. An assessment of peripheral vascular disease in patients with diabetic foot ulcer. Foot (Edinburgh, Scotland). 2010 Dec:20(4):114-7. doi: 10.1016/j.foot.2010.09.002. Epub 2010 Oct 15 [PubMed PMID: 20951569]
Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis (†). Annals of medicine. 2017 Mar:49(2):106-116. doi: 10.1080/07853890.2016.1231932. Epub 2016 Nov 3 [PubMed PMID: 27585063]
Level 1 (high-level) evidenceSnyder RJ, Jensen J, Applewhite AJ, Couch K, Joseph WS, Lantis Ii JC, Serena TE. A Standardized Approach to Evaluating Lower Extremity Chronic Wounds Using a Checklist. Wounds : a compendium of clinical research and practice. 2019 May:31(5 Suppl):S29-S44 [PubMed PMID: 31033453]
Noor S, Khan RU, Ahmad J. Understanding Diabetic Foot Infection and its Management. Diabetes & metabolic syndrome. 2017 Apr-Jun:11(2):149-156. doi: 10.1016/j.dsx.2016.06.023. Epub 2016 Jun 18 [PubMed PMID: 27377687]
Level 3 (low-level) evidenceAbabneh M, Al Ayed MY, Robert AA, Al Dawish MA. Clinical Utility of the Ankle-Brachial Index and Toe Brachial Index in Patients with Diabetic Foot Ulcers. Current diabetes reviews. 2020:16(3):270-277. doi: 10.2174/1573399815666190531093238. Epub [PubMed PMID: 31146664]
Braun LR, Fisk WA, Lev-Tov H, Kirsner RS, Isseroff RR. Diabetic foot ulcer: an evidence-based treatment update. American journal of clinical dermatology. 2014 Jul:15(3):267-81. doi: 10.1007/s40257-014-0081-9. Epub [PubMed PMID: 24902659]
Onesti MG, Fioramonti P, Fino P, Sorvillo V, Carella S, Scuderi N. Effect of enzymatic debridement with two different collagenases versus mechanical debridement on chronic hard-to-heal wounds. International wound journal. 2016 Dec:13(6):1111-1115. doi: 10.1111/iwj.12421. Epub 2015 Feb 3 [PubMed PMID: 25649929]
Elraiyah T, Prutsky G, Domecq JP, Tsapas A, Nabhan M, Frykberg RG, Firwana B, Hasan R, Prokop LJ, Murad MH. A systematic review and meta-analysis of off-loading methods for diabetic foot ulcers. Journal of vascular surgery. 2016 Feb:63(2 Suppl):59S-68S.e1-2. doi: 10.1016/j.jvs.2015.10.006. Epub [PubMed PMID: 26804369]
Level 1 (high-level) evidenceTchanque-Fossuo CN, Dahle SE, Lev-Tov H, West KIM, Li CS, Rocke DM, Isseroff RR. Cellular versus acellular matrix devices in the treatment of diabetic foot ulcers: Interim results of a comparative efficacy randomized controlled trial. Journal of tissue engineering and regenerative medicine. 2019 Aug:13(8):1430-1437. doi: 10.1002/term.2884. Epub 2019 May 9 [PubMed PMID: 31070860]
Level 2 (mid-level) evidenceNiezgoda JA, Van Gils CC, Frykberg RG, Hodde JP. Randomized clinical trial comparing OASIS Wound Matrix to Regranex Gel for diabetic ulcers. Advances in skin & wound care. 2005 Jun:18(5 Pt 1):258-66 [PubMed PMID: 15942317]
Level 1 (high-level) evidenceSuresh DH, Suryanarayan S, Sarvajnamurthy S, Puvvadi S. Treatment of a non-healing diabetic foot ulcer with platelet-rich plasma. Journal of cutaneous and aesthetic surgery. 2014 Oct-Dec:7(4):229-31. doi: 10.4103/0974-2077.150786. Epub [PubMed PMID: 25722604]
Level 3 (low-level) evidenceHealth Quality Ontario. Hyperbaric Oxygen Therapy for the Treatment of Diabetic Foot Ulcers: A Health Technology Assessment. Ontario health technology assessment series. 2017:17(5):1-142 [PubMed PMID: 28572866]
Zhou X, Zhang J, Feng G, Shen J, Kong D, Zhao Q. Nitric Oxide-Releasing Biomaterials for Biomedical Applications. Current medicinal chemistry. 2016:23(24):2579-2601 [PubMed PMID: 27480214]
Morton LM, Phillips TJ. Wound healing and treating wounds: Differential diagnosis and evaluation of chronic wounds. Journal of the American Academy of Dermatology. 2016 Apr:74(4):589-605; quiz 605-6. doi: 10.1016/j.jaad.2015.08.068. Epub [PubMed PMID: 26979352]
Oyibo SO, Jude EB, Tarawneh I, Nguyen HC, Harkless LB, Boulton AJ. A comparison of two diabetic foot ulcer classification systems: the Wagner and the University of Texas wound classification systems. Diabetes care. 2001 Jan:24(1):84-8 [PubMed PMID: 11194247]
Ndosi M, Wright-Hughes A, Brown S, Backhouse M, Lipsky BA, Bhogal M, Reynolds C, Vowden P, Jude EB, Nixon J, Nelson EA. Prognosis of the infected diabetic foot ulcer: a 12-month prospective observational study. Diabetic medicine : a journal of the British Diabetic Association. 2018 Jan:35(1):78-88. doi: 10.1111/dme.13537. Epub 2017 Nov 20 [PubMed PMID: 29083500]
Level 2 (mid-level) evidenceMegallaa MH, Ismail AA, Zeitoun MH, Khalifa MS. Association of diabetic foot ulcers with chronic vascular diabetic complications in patients with type 2 diabetes. Diabetes & metabolic syndrome. 2019 Mar-Apr:13(2):1287-1292. doi: 10.1016/j.dsx.2019.01.048. Epub 2019 Jan 24 [PubMed PMID: 31336479]
Ugwu E, Adeleye O, Gezawa I, Okpe I, Enamino M, Ezeani I. Predictors of lower extremity amputation in patients with diabetic foot ulcer: findings from MEDFUN, a multi-center observational study. Journal of foot and ankle research. 2019:12():34. doi: 10.1186/s13047-019-0345-y. Epub 2019 Jun 14 [PubMed PMID: 31223342]
Level 2 (mid-level) evidenceRan XW, Zhao JC. [The importance of multidisciplinary foot-care services in the management of diabetic patients with peripheral artery disease and diabetic foot ulcers]. Sichuan da xue xue bao. Yi xue ban = Journal of Sichuan University. Medical science edition. 2012 Sep:43(5):728-33 [PubMed PMID: 23230749]
Pinzur MS, Cavanah Dart H, Hershberger RC, Lomasney LM, O'Keefe P, Slade DH. Team Approach: Treatment of Diabetic Foot Ulcer. JBJS reviews. 2016 Jul 26:4(7):. pii: e5. doi: 10.2106/JBJS.RVW.15.00080. Epub [PubMed PMID: 27509330]
